Adverse Skin Reactions to Personal Protective Equipment Among Health-Care Workers During COVID-19 Pandemic: A Multicenter Crosssectional Study in Indonesia
2021-01-09PaulusMarioChristopherReginaStefaniRorenClarissaTaniaNanaNoviaJayadiCucunawangsihCucunawangsih
Paulus Mario Christopher∗, Regina Stefani Roren Clarissa Tania Nana Novia Jayadi,Cucunawangsih Cucunawangsih
1Faculty of Medicine, Pelita Harapan University, Banten 15811, Indonesia; 2Department of Dermatology and Venereology, Faculty of Medicine, Pelita Harapan University, Banten 15811, Indonesia; 3Department of Microbiology, Faculty of Medicine, Pelita Harapan University, Banten 15811, Indonesia.
Abstract
Keywords: adverse skin reactions, health-care workers, PPE, COVID-19, Indonesia
Introduction
Nearing the end of a decade, in December 2019, reports about a newly emerged viral-like pneumonia caused by Severe Acute Respiratory Syndrome Coronavirus 2(SARS-CoV-2) was announced by the People’s Republic of China.1The virus wreaked havoc causing a pandemic of Coronavirus disease 2019 (COVID-19). Indonesia is one of the countries affected by this pandemic,with a total case reaching approximately 287,000 cases nationwide by September 30,2020.2In an attempt to minimize the risk of contracting the virus, the World Health Organization(WHO) recommended the use of personal protective equipment(PPE)for the community,including health-care workers (HCWs).3
Together with the recommendations from WHO, the former Indonesian COVID-19 Response Acceleration Task Force released a guideline necessitating the use of PPE for HCWs caring for patients in health-care facilities. This guideline divided PPE into three levels based on the risk of transmission.4This use of PPE accompanied by the practice of maintaining hand hygiene increases the risk of adverse skin reactions in HCWs.Several adverse skin reactions/manifestations that have been reported in the previous studies were dryness or scales, papules or erythema, and maceration with the most commonly affected areas were hands, cheeks, and nasal bridge.5
Adverse skin reactions in HCWs can be minimized,prevented, and treated accordingly to provide a better working environment and expectantly to reduce stress in the working environment.However,little is known about the current issue of adverse skin reactions in HCWs,specifically, the prevalence and characteristics of the adverse skin reactions and their associated risk factors with only a few published reports have been published.This study aimed to address the prevalence and characteristics-, possible risk factors-, and suggest possible solutions towards adverse skin reactions to PPE among HCWs in a multi-center setting of Banten province,Indonesia.
Material and methods
Study design and setting
In this cross-sectional study, HCWs of Banten Province were surveyed from June 1 to August 31, 2020. Three hospitals around Banten Province,Siloam Hospitals Lippo Village, Siloam Hospitals Kelapa Dua, and Siloam Teaching Hospital, were included. The present study was approved by the Ethics Committee of the Faculty of Medicine, Pelita Harapan University (Ref: 151/K-LKJ/ETIK/VII/2020). All respondents granted their electronic informed consent and all data were anonymized before analysis by de-identifying respondent data. The design,setting,analyses,and reporting of this study adhered to the STROBE guidelines for cross-sectional studies in epidemiology.6
Study population
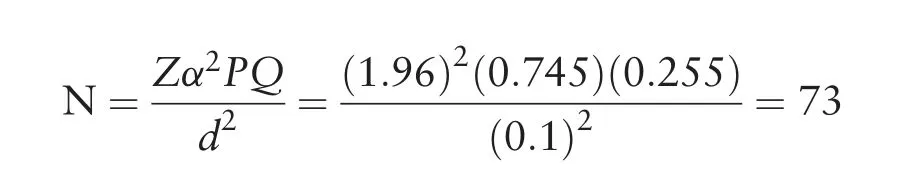
The sample size was determined using Cochran sample size formula for categorical data with a 10% margin of error and a 95% confidence level together (level of significance α=0.05) along with the proportion of case reported from previous literature yielding the minimum sample size (N) of HCWs required for this study was 73 respondents.5,7
The study used a purposive sampling method and addressed HCWs constituting medical students undergoing clinical clerkship, general practitioners, specialists,nurses, midwives, laboratory personnel, radiographers,and pharmacists,caring for patients during the COVID-19 pandemic and working in either one of the three hospitals.
Data collection and management
The data collected for the study was obtained using a validated online survey questionnaire according to the relevant guides and literature and was further reviewed and revised by consulting a board certified dermatovenereologist and an infection control expert. The questionnaire consisted of(1)demographic characteristics(sex, age, and occupation), (2) occupational-related characteristics (main working department, hospital type in terms of COVID-19 referral,level of PPE,hand hygiene frequency, layers of gloves worn, duration of PPE worn daily and weekly,break opportunity during the use of PPE in every shift, daily showering frequency, use of a moisturizer and a dressing material),and(3)adverse skin reactions (history of pre-existing chronic skin disease,heavy sweating condition, anatomical site, sign and symptoms, and steps adopted for preventive/therapeutic measures). The questionnaire provided multiple-choice responses as well as space for comments to the questions.To ensure a comprehensive understanding, especially in focus to the adverse skin reactions, each adverse skin reactions’choice had a definition and synonym of a more common word.
For analytical purposes,the occupation was divided into three namely, (1) doctor (medical student undergoing clinical clerkship, general practitioner, and specialist), (2)nurses and midwives, and (3) other medical personnel(laboratory personnel, radiographer, and pharmacist).The hand hygiene frequency, daily and weekly wearing time of PPE, break opportunity in every shift, and daily showering frequency was each dichotomized into two groups based on the median.
Statistical analysis
The data collected from the questionnaires were tabulated into Excel files (Microsoft Excel, Microsoft Corp. Redmond,WA,USA).Statistical analyses were performed using Statistical Package forSocial Sciences Statistics Version21.0(IBM Corp., Released 2012, Armonk, NY, USA). Demographic characteristics, occupation-related characteristics,and adverse skin reactions were summarized by using descriptive statistics.To determine the potential association of demographic and occupational-related characteristics on adverse skin reactions, demographic and occupationalrelated characteristics was screened individually using univariate logistic regression analysis. The explanatory variables which were significant at P≤0.25 were then offered to the multivariable logistic regression model to control the potential effects of confounders and to understand the associations of adverse skin reactions with the demographic and occupational-related characteristics.Confounding factors were explored by comparing the difference between the adjusted odds ratio in multivariate analysesandthecrudeoddsratio inunivariateanalyses.The model goodness-of-fit was assessed by the Hosmer-Lemeshow test.P values<0.05 were considered significant statistically and odds ratio with 95%confidence interval to establish the strength of associations as well as a measure of precision.
Results
An estimated maximum of 500 surveys was distributed and 201 HCWs responded,yielding to a 40.2%response rate. The study included 201 respondents with one respondent refused to participate.Hence,the total number of respondents eligible in the research was 200 samples.
Demographics and occupational-related characteristics
During the study period, the majority of the respondents were female (67.0%) and youth (≤24 years old) (57.0%)with a mean age±SD(range)of 26.9±7.2(20-58)years old and a median of 24 years old. Regarding their occupational-related aspect, samples were predominated by the general practitioner (37.0%) from Group B department (57.0%) in a non-referral center for COVID-19 hospital (66.0%). Ninety respondents(45.0%)worn level two PPE and similarly 86 respondents(43.0%)used a single layer glove.The mean±SD(range)of the hand hygiene frequency, duration of PPE worn dailEy and weekly, break opportunity in every shift, and daily showering frequency of 22.4±14.0(5.0-100)times/day, 6.8±3.2 (1.0-17.0) hours/day, 4.8±1.5 (1.0-7.0)days/week,every 3.5±2.2(0.5-10.0)hours/shift,and 2.5±0.9(0-6.0)times/day,respectively.The median of hand hygiene frequency, duration of PPE worn daily and weekly, break opportunity in every shift, and daily showering frequency were 20times/day, 7hours/day, 5 days/week, every 4hours/shift, and 2times/day, respectively. A larger portion of the respondent (56.0%) had used a moisturizer, nonetheless, only 17 respondents(8.5%) used a dressing material for the prevention of adverse skin reactions (Table 1).
Prevalence and characteristics of adverse skin reactions
During the study period, 133 respondents (66.5%)experienced self-perceived adverse skin reactions. Out ofthis, 48 respondents (36.1%) reported a history or preexisting chronic skin disease, namely dermatitis (29.3%),acne (3.0%), urticaria (1.5%), psoriasis (1.5%), and chronic dry skin (0.8%). The majority (74.4%) experienced a heavy sweating condition. The cheeks and chin(69.9%)were the most common site affected with dryness/tightness (63.9%) and acne (77.4%) being the most reported symptom and adverse skin reaction,respectively.Itch(59.4%)was the second most complaint symptom and a numerical rating scale for itch was obtained yielding a mean±SD (range) of 4.3±2.9 (0-10.0). With regards to the self-perceived adverse skin reactions, interestingly, 81 respondents (60.9%) used a moisturizer as a preventive and/or management of this issue while 32 respondents(24.1%) did not take any step for prevention and/or management of this issue. These adverse skin reactions even cost work absenteeism in 6 respondents (4.5%)(Table 2).

Table 1 Demographics and occupational-related characteristics of the subjects in this study.
Associations between demographics, occupationalrelated characteristics, and the prevalence of adverse skin reactions
Adverse skin reactions were observed primarily in females (73.7%) under the youth age group (61.7%)working as a doctor (82.7%) followed by nurse and midwife (11.3%) in department group A (54.1%) of a non-referral center for COVID-19(60.2%).The majority of the adverse skin reactions were contributed from wearing level 2 and 3 PPE (43.6% and 37.6%,respectively) for ≥7hours/day (59.4%), ≥5days/week(57.9%) with no break opportunity in every shift(56.4%). Hand hygiene frequency of ≥20times/day(60.2%) as well as double or more layers of gloves(45.1%)also played a role in these adverse skin reactions.Furthermore, a large proportion of the respondent had not used dressing material for the prevention(91.0%)to the adverse skin reactions.
The univariate logistic regression analysis revealed ten variables from a total of 14 variables that were significant(P≤0.25)with adverse skin reactions,namely sex, age group classification, main working department,hospital type,level of PPE worn,hand hygiene frequency,layers of gloves, and duration of PPE worn daily, break opportunity in every shift, and use of a moisturizer.This analysis was done to assess the association between the variables and adverse skin reactions prevalence. The final models were created using multivariable logistic regression analysis. There were five significant variables,namely sex, age group classification, level of PPE worn, hand hygiene frequency, and duration of PPE worn daily for the prevalence of adverse skin reactions(Table 3).
Discussion
The first confirmed case of SARS-CoV-2 infection in Indonesia was announced on March 2,2020.8Since then,the spread of COVID-19 has increased almost immediately. This pandemic has affected medical practice in a multitude of manners such as,PPE use and frequent hand hygiene to name a few.With the escalation of PPE use and hand hygiene,numerous adverse skin reactions have been reported. With this present study, we will discuss our findings against previous literature and the data we have at hand.

Table 2 Characteristics of adverse skin reactions to personal protective equipment among health-care workers.

Table 3 Univariate and multivariate factors associated with adverse skin reactions to personal protective equipment among health-care workers.
The response rate of this study was 40.2%similar to the response rate in previous literature (>37.6%).5The reported rate of adverse skin reactions is much higher compared to occupational contact dermatitis in HCWs during normal working conditions(16.5%-44.4%)or any other previous outbreak[SARS in 2003(1.6%-35.5%)].9-10Female dominated the study with 67.0%as seen in other literature in which sex was found to be statistically significant as shown in our present study.5,11Likewise,this study found that respondents’mean age±SD(range)was 26.9±7.2(20.0-58.0)years old,similar with the previous study of 32.2±6.5 years.5A possible explanation for these variables is due to females and adults paying more attention to their skin and related daily skincare and also an improvement in their health-seeking behavior.
Two groups between doctors and nurses and midwives(67.9%vs.65.2%)showed similar adverse skin reactions,probably explained by similar PPE levels used. Lower adverse skin reactions (53.3%) in paramedical personnel could be explained by lower number of participants in the paramedical group.The main working department as well the hospital type have their share of the adverse skin reactions in which HCWs in group B (critical care unit,laboratory, testing room, operation room, COVID-19 isolation ward)and referral center for COVID-19 reported a higher rate(79.5%and 77.9%,respectively)of adverse skin reactions and were found to be statistically significant.These findings were found to be similar to previous literature.5A potential underlying explanation is due to high job strain,high stress levels or improper handling of work pressures, stress factors and emotions during the conflict and in decision-making situations may have a negative impact on the onset or course of skin disorders.12
With the varying level of PPE standards recommended,different components of PPE are related to the different adverse skin reactions. Level 1 PPE comprised of 3-ply surgical mask, gloves, and normal clothing while level 2 PPE comprised of level 1 PPE with an additional head cap,goggles,and gown.Lastly,level 3 PPE constituted of head cap, goggles and face shield, N95 mask or equivalent,coverall/gown and apron, surgical gloves, and boots/rubber shoes with a protector. In the highlight of this study, these levels of PPE coupled with duration of PPE worn daily(≥7hours)towards adverse skin reactions have shown to be statistically significant as reported from previous literature.5,11The airtightness of a PPE, highintensity work, and longer working hours leading to prolonged use of PPE resulted in a change in skin microclimate and decreased skin tolerance influencing the development of adverse skin reactions.11
The top three most affected sites and reported symptoms were cheeks and chin, forehead, and nasal bridge with dryness/tenderness, itch, and rash, respectively. On the other hand, acne ranked first as the most commonly reported signs.These findings were similar to the previous literature.5,13-14The top three most affected site findings can be extrapolated to the use of masks in which HCWs must wear masks for a long period during shift and off work due to the infectivity of the COVID-19.Additionally,masks were tied tightly and the metal clip was squeezed hardly to ensure the tightness of the mask leading to excessive pressure of the mask and metal clip on the nasal bridge. Further skin damage may be contributed due to the excessive binding of the mask,such as that the edge of the mask is in close contact with the skin together with wearing the mask for a long period.15-16Dryness/tenderness, itch, and rash may be due to discomfort of wearing the PPE over a long period of time, protective clothing being muggy and combined with the excessive humid internal environment,in particular for masks.The finding of acne as the most recognized sign reported was expected, since mechanical factors of mask coalesce with the excessive humid internal environment lead to swelling of epidermal keratinocytes of the pilosebaceous follicle and eventually lead to obstruction.Hence,contributing to the pathogenesis of acne.17
These sites, symptoms, and signs can be prevented or minimized through reduction of the intensity of binding to achieve moderate tightness and to pinch gently on the metal clip at the nasal bridge, and if possible, a timely break from masks and PPE.Self-medication as seen in this study through the use of a topical steroid and oral antihistamine was in line with other literature.15In terms of acne, it is advised to do (1) a proper skin cleansing with gentle, mild fragrance-free, non-comedogenic cleanser in the morning and at the end of the day, (2) reasonable selection of skincare products, (3) a low-sugar diet, (4)avoidance of irritation (eg, squeezing pimples), and if required (5) medication of topical and/or oral preparations.18
The practice of hand hygiene among HCWs has been there,long before the COVID-19 pandemic.Hand hygiene plays an important role in the reduction and prevention of healthcare-associated infections worldwide.19Therefore in 2009,WHO created guidelines on hand hygiene in health care.20However,repetitive action of hand hygiene practice is known to be a significant risk factor of occupational irritant hand dermatitis/hand eczema as previously stated by several studies done in different countries of the different climate, humidity, skin-type majorities, and medical backgrounds (doctors, nurses, dentists, medical students).21-22Similar results shown in our study,washing hands more than 20 times a day double the risk of adverse skin reactions in HCWs. This results in reduced HCWs compliance to hand hygiene practice.19
Hand eczema can be caused by irritant or allergic contact dermatitis, or endogenous factors such as atopic dermatitis.22Hand hygiene products disrupt skin barrier by(1)causing denaturation of stratum corneum proteins,(2)changes in intercellular lipids,(3)decreased corneocyte cohesion, and (4) decreased stratum corneum waterbinding capacity.19-20This skin damage can promote entries of virus and bacteria, including COVID-19.23-24Washing hands with soaps are known to cause more adverse skin reactions than using alcohol rubs.20,23,25
Coronavirus was found to survive for several hours on used PPE, therefore double gloving is recommended to reduce the risk of viral contamination during PPE removal.A previous study showed layers of gloves are not significantly related to adverse skin reactions on HCWs during the COVID-19 pandemic.5In contrast with the previous study,our study shows layers of gloves associated with adverse skin reactions in univariate analysis. Longterm use of gloves may lead to overhydration of the stratum corneum, which may cause maceration and erosion. Chemical materials in latex gloves are likely to cause contact dermatitis in macerated or erosive skin.26
In order to maintain compliance of hand hygiene practice in healthcare workers, several recommendations have been made to prevent skin irritation/ hand eczema.According to the WHO,there are three primary strategies for minimizing hand hygiene-related irritant contact dermatitis among HCWs: selecting less irritating hand hygiene products (preferably alcohol-based hand rubs containing humectants), avoiding certain practices that increase the risk of skin irritation(washing hands before or after applying alcohol and/or using hot water to wash hands), and using moisturizing skincare products following hand cleansing (regularly and more often during holiday/day-offs).20,25-26Most HCWs are unaware of these preventive measures,thereby education and promotion hold a crucial part,especially in the setting of COVID-19 pandemic whereas the working environment can become more stressful than usual.
Performance of HCW for clinical and laboratory work while wearing PPE might be reduced due to the exerted constrictions compared to the same work without PPE.27In light of the above situations,break during PPE wearing is needed. In our study, a higher rate of adverse skin reactions happened in HCWs without break during their shift, although not statistically significant. It is advised to take appropriate breaks from masks (surgical and N95)every 2 hours for 15 minutes off to prevent acne and moisture-associated skin irritation as well as breaks and frequent replacement of protective clothing.26,28
Further measures to protect from the skin and mucous membrane injury have been acknowledged. The Chinese have published a Consensus on the protection of skin and mucous membrane barrier for HCW fighting against COVID-19, one of the recommendations was the use of moisturizers and the use of dressing materials for prevention.18,26Interestingly, in our study, the majority has used moisturizers,yet only a small proportion has used a dressing material for prevention contributing to the high prevalence of adverse skin reactions. This may be contributed due to a previous pre-existing chronic skin condition leading to a compromised skin barrier,experiencing heavy sweat condition leading to overhydration causing cutaneous dysbacteriosis and further skin barrier dysfunction, different types of moisturizer formulation, possible inadequacy and/or untimely application of moisturizer, and/or lack of dressings to reduce mechanical load and minimize friction applied to the skin and soft tissues.29Our study also reported showering frequency which was found not to be statistically significant in line from the previous study.5
It is recommended to control working hours with PPE and showering timely upon leaving the contaminated areas with weak acidic or neutral detergents while avoiding showering with over hot waters and alkaline detergents.Application of moisturizers after showering, before and after wearing facial protective equipment to lubricate and minimize friction between the skin and masks or goggles,and especially when not in direct patient care.19The use of hydrogel-, hydrocolloid-, or foam dressings is recommended to prevent stress injuries.18,29In case of serious adverse skin reactions to PPE occurred or medicinal administration resulted ineffectively,they should seek help from a dermato-venereologist.
Lastly, health and safety training is considered as an important factor for occupational-related contact dermatitis as this will improve the knowledge and understanding of employees regarding the prevention and control of the risks and hazards associated with adverse health conditions, as this generally improves early recognition and warning of the conditions.The provision of safety training for workers at the earliest possible period of employment might also enhance workplace safety cultures and practices.The authors would like to suggest future studies to assess the associations between health and safety training and occupational-related contact dermatitis, in particular, adverse skin reactions to PPE.30
This present study has following limitations: First, this study included response bias in which HCWs with adverse skin reactions were more likely to respond. Second,adverse skin reactions reported by respondents could not be validated by dermato-venereologists.Third,we did not study based on each components of varying levels of PPE,in which it can impact one site by a single or multiple exposure factors. Fourth, possible associated risk factors outside hospital, such as the use of masks and hand hygiene after work in daily life were not included.Lastly,the study was based on a cross-sectional design leading for difficulty between the outcome of interest and factors influencing its occurrences.
In conclusion, adverse skin reactions are a common occupational-related skin problem among HCWs during this COVID-19 pandemic. The findings suggest that sex,age group classification, level of PPE worn, hand hygiene frequency, and duration of PPE worn daily show as significant risk factors to adverse skin reactions.Nonetheless,our study provides an insight into the prevalence and characteristics of adverse skin reactions related to PPE during the current pandemic.Further strengthening of the skin condition and awareness on how to minimize,prevent, and treat adverse skin reactions should be advocated.
Acknowledgments
The authors thank all the HCWs who gave their time and effort in participating in this study.We also acknowledge Siloam Hospitals Lippo Village, Siloam Hospitals Kelapa Dua, and Siloam Teaching Hospital for giving us the opportunity to conduct the study.
杂志排行
国际皮肤性病学杂志的其它文章
- Instructions for Authors
- Platelet-Rich Plasma for Androgenetic Alopecia in Women: A Single-Center Case Series Study in Qatar
- Intracranial Abnormalities of Infantile Hemangiomas in the Head and Neck Regions:A Retrospective MRI Study
- Efficacy and Safety of Prednisolone Monotherapy Versus Prednisolone Plus Methotrexate in Erythema Nodosum Leprosum(Type 2 Lepra Reaction)
- The Past 70 Years in Control of Syphilis in China: Elimination and Responses to Resurgence
- Hair Matrix Cyst