Trends and challenges of emergency and acute care in Chinese mainland: 2005-2017
2021-01-06ChangPanJiaojiaoPangKaiChengFengXuYuguoChen
Chang Pan, Jiao-jiao Pang, Kai Cheng, Feng Xu, Yu-guo Chen
1 Department of Emergency Medicine, Qilu Hospital of Shandong University, Jinan 250012, China
2 Shandong Provincial Clinical Research Center for Emergency and Critical Care Medicine; Institute of Emergency and Critical Care Medicine of Shandong University; Chest Pain Center; Qilu Hospital of Shandong University, Jinan 250012, China
3 Key Laboratory of Emergency and Critical Care Medicine of Shandong Province; Key Laboratory of Cardiopulmonary-Cerebral Resuscitation Research of Shandong Province; Shandong Provincial Engineering Laboratory for Emergency and Critical Care Medicine; Qilu Hospital of Shandong University, Jinan 250012, China
4 The Key Laboratory of Cardiovascular Remodeling and Function Research, Chinese Ministry of Education, Chinese Ministry of Health and Chinese Academy of Medical Sciences; the State and Shandong Province Joint Key Laboratory of Translational Cardiovascular Medicine; Qilu Hospital of Shandong University, Jinan 250012, China
Corresponding Author: Feng Xu, Email: xufengsdu@126.com; Yu-guo Chen, Email: chen919085@126.com
KEYWORDS: Emergency medical service system; Emergency visits; Capabilities; Challenges
INTRODUCTION
Emergency medical service system (EMSS),including pre-hospital emergency care and hospital-based emergency departments (EDs), is essential in providing acute care services for a range of health conditions,such as life-threatening injuries, acute cardiovascular and cerebrovascular diseases, and complications due to pregnancy.
The quality and responsiveness of EMSS reflect the level of health care in a country. Following China’s national meeting on health and the announcement of the“Healthy China 2030” plan, marked changes have been initiated to expand or advance the Chinese healthcare system, including broadening enrollment in the universal medical insurance system, health profession workforce development, and hierarchical medical treatment system. In particular, larger tertiary hospitals, which are responsible for acute and critical patients according to these reform policies, will face an influx of emergency and critically ill patients as the healthcare regionalization in China continues. In 2017, China’s EDs of hospitals managed an estimated 166.5 million visits, and the requirement for high-quality acute and critical care services will grow exponentially through improved and more regionalized healthcare delivery.[1]
However, trends of emergency and acute care in China have not been studied systematically to date. In this study, we quantified and described the trends of emergency visits, capabilities, and challenges of China’s EMSS in the past decade in detail. Our f indings can offer a theoretical basis for improving the quality of emergency care in China, and help the world to understand China’s EMSS. Additionally, our reports are able to provide experience to the EMSS development worldwide, especially for the developing countries with similar conditions.
METHODS
Search strategy and selection criteria
We searched for publications and other materials describing or evaluating EMSS of China both in Chinese and English. We reviewed the official documents issued by the Ministry of Health (MOH, now the National Health and Family Planning Commission), yearbooks,published reports, and news reports from domestic and international sources. We also searched PubMed, China National Knowledge Infrastructure (CNKI), Wanfang databases, and Baidu data, and manually screened the references of relevant articles. Our search strategy included the terms “emergency medical service”,“emergency medicine”, “emergency care”, “acute care”,“emergency department”, “emergency room”, “prehospital emergency care”, and “ambulance”, combined with the terms “China” and “Chinese”, or combined with the terms “overcrowding”, “crowding”, “length of stay”, “boarding time”, “access block”, “medical disputes”, “medical complaints”, “medical disturbance”,“medical violence”, “doctor-patient relationship”,“environment”, “condition”, “situation”, “workforce”,“human resources”, “exhaustion”, “burnout”, “overload”,“staff retention”, “staff recruitment”, “staff enrollment”,“staff shortage”, and “staff stability”. We also searched the websites of Chinese Government agencies for related documents and statistics.
Data collection of emergency visit numbers in China
TheChina Health and Family Planning Statistical Yearbooks(2006-2018) described and analyzed the medical and health services, the health status of residents, and family planning in the Chinese mainland in the previous years,which were the key references of our study.[1,2]All hospitals in China were assessed, excluding maternal and child health hospitals, specialized prevention stations, and sanatoriums.The raw data on the number of emergency visits, including patients presenting to EDs of hospitals and pre-hospital emergency care, were extracted from theChina Health and Family Planning Statistical Yearbooks2008-2018 and 2010-2018,[1,2]respectively. In the yearbook2008, the number of patients presenting to EDs of hospitals in 2007 was first recorded, while the number of patients presenting to pre-hospital emergency care was first included in the yearbook2010. Thus, the related data were extracted and analyzed from the corresponding years.
Data collection of capabilities of emergency and acute care in China
Capabilities of EMSS were evaluated by the number of licensed emergency physicians, beds in hospital-based EDs,and the health workforce in pre-hospital emergency care.The health workforce in pre-hospital emergency care covers licensed doctors, assistant doctors, and nurses. The original data were also derived from theChina Health and Family Planning Statistical Yearbooks2006-2018.[1,2]The number of emergency physicians in EDs in 2005 was f irst recorded in the yearbook 2006, but the data in 2006-2008 were not counted in the yearbooks2007-2009. The number of beds in EDs in 2007 was recorded in the yearbook 2008 for the f irst time. Thus, the related data were extracted and analyzed from the corresponding years.
RESULTS
Growing number of emergency visits during the past decade
During the past decade, the number of patients presenting to EDs has increased among all levels of hospitals in China. From 2007 to 2017, the number of ED visits tripled, from 51.9 million to 166.5 million(Figure 1A). The Chinese population reliant on the ED for clinical care was also increased as reflected by the rise from 3.28% in 2007 to 4.95% in 2017 in the proportion of ED visits relative to all clinical visits.Commensurate with rising demand for ED care, the utilization of pre-hospital emergency care increased by 113% from 3.2 million to 6.8 million between 2009 and 2017 (Figure 1B). In addition, from 2007 to 2015, the number of patients presenting to EDs of hospitals in the eastern, central, and western regions of China increased by 183%, 262%, and 277%, respectively (Figure 1C).
Enhanced capabilities of EMSS during the past decade
Between 2005 and 2017, the number of licensed emergency physicians in EDs of hospitals increased by 196% from 20,058 to 59,409 (Figure 2A) with the data in 2006-2008 missing, and the proportion of emergency physicians among all doctors increased by 40% from 1.5% in 2005 to 2.1% in 2017. The total number of beds in hospital-based EDs in China increased from 10,783 in 2007 to 42,367 in 2017 (Figure 2B). Likewise, in the pre-hospital settings, the size of the health workforce doubled from 3,687 to 8,671, with a 109% increase in the number of physicians from 1,774 to 3,712 and 165% of registered nurses from 1,314 to 3,478 between 2005 and 2017 (Figure 2C).

Figure 1. Statistical graphs of changes in numbers of patients presenting to hospitals’ EDs and to pre-hospital emergency care in China. A: from 2007 to 2017, the number of ED visits tripled; the data before 2007 were not counted in China’s yearbooks; B: from 2009 to 2017, the utilization of pre-hospital emergency care increased by 113%; the data before 2009 were not counted in China’s yearbooks; C: from 2007 to 2017, the number of patients presenting to EDs of hospitals in the eastern, central, and western regions of China increased by 183%, 262% and 277%, respectively; EDs:emergency departments.
Challenges faced by China’s EMSS
Despite improvements in infrastructure and expansion of resources dedicated to acute and critical care in China’s EMSS, several substantial challenges persisted, which made contributions to the phenomenon that the overall mortality of emergency patients increased in tertiary hospitals although decreased all over China during the past decade.[3]
Overcrowding and the long length of stay in EDs
A recent survey of 33 tertiary hospitals in 31 provinces conducted by the Chinese College of Emergency Physicians documented that overcrowding in EDs was very common, as reflected by frequent ambulance diversion,a rare event prior to recent reforms.[4]In a cross-sectional survey of 43 tertiary and secondary hospitals in Beijing,30.2% reported overcrowding, and 34.9% had instances of more than f ive emergency patients experiencing admission delays over 72 hours.[5]
The length of stay in EDs in China is considerable,with 50% of Beijing EDs reporting longer than 6 hours on average, which stands in contrast to a national average length of stay of 154 minutes in the USA with only 11.1%of patients spending over 6 hours in the ED.[6,7]A study of 17 tertiary hospitals from 12 provinces documented that in 77% of EDs over 50% of patients suffered access block to inpatient wards in 2012 (compared to 34% of EDs in 2000,and 25% in the 1980s).[8]Moreover, in an analysis from a typical hospital in Shanghai, 2,702 patients during one year waited in the EDs for over 48 hours.[9]
Poor work environment
The poor work environment of China’s hospitals has been well documented;[10]however, the degree to which patient distrust complicates EMSS care is even more extreme.[4,8,11]Particularly notable to EMSS are frequent medical disputes, complaints, and even violence.[12]The latter disturbances have a substantial influence on EMSS doctors who try to make more rapid and efficient decisions while also engage patients and families at the time of acute illness. A notable example of distrust with real implications for patient outcomes is that of EMSS patients with ST-segment elevation myocardial infarction(STEMI). These patients face the prolonged door to balloon (D to B) time and are less likely to meet the optimal treatment window for coronary revascularization and myocardial reperfusion.[13,14]As a reflection of this adversarial work environment, the proportion of EDs facing five or more medical disputes increased from zero in 1980 to nearly 12% in 2012. Furthermore, the rate of medical complaints increased dramatically from 11.1% to 70.6% within the same timeframe.[8]Such an adversarial atmosphere is also not limited to words or written complaints; a commensurate rise in physical violence towards healthcare providers has been seen with survey data indicating that two-thirds of violence towards healthcare providers occurs in the ED.[11]With such a toxic work environment, emergency healthcare providers, including physicians, nurses, and ancillary staff, face increasing exhaustion and burnout, which further threatens the quality and safety of acute care.
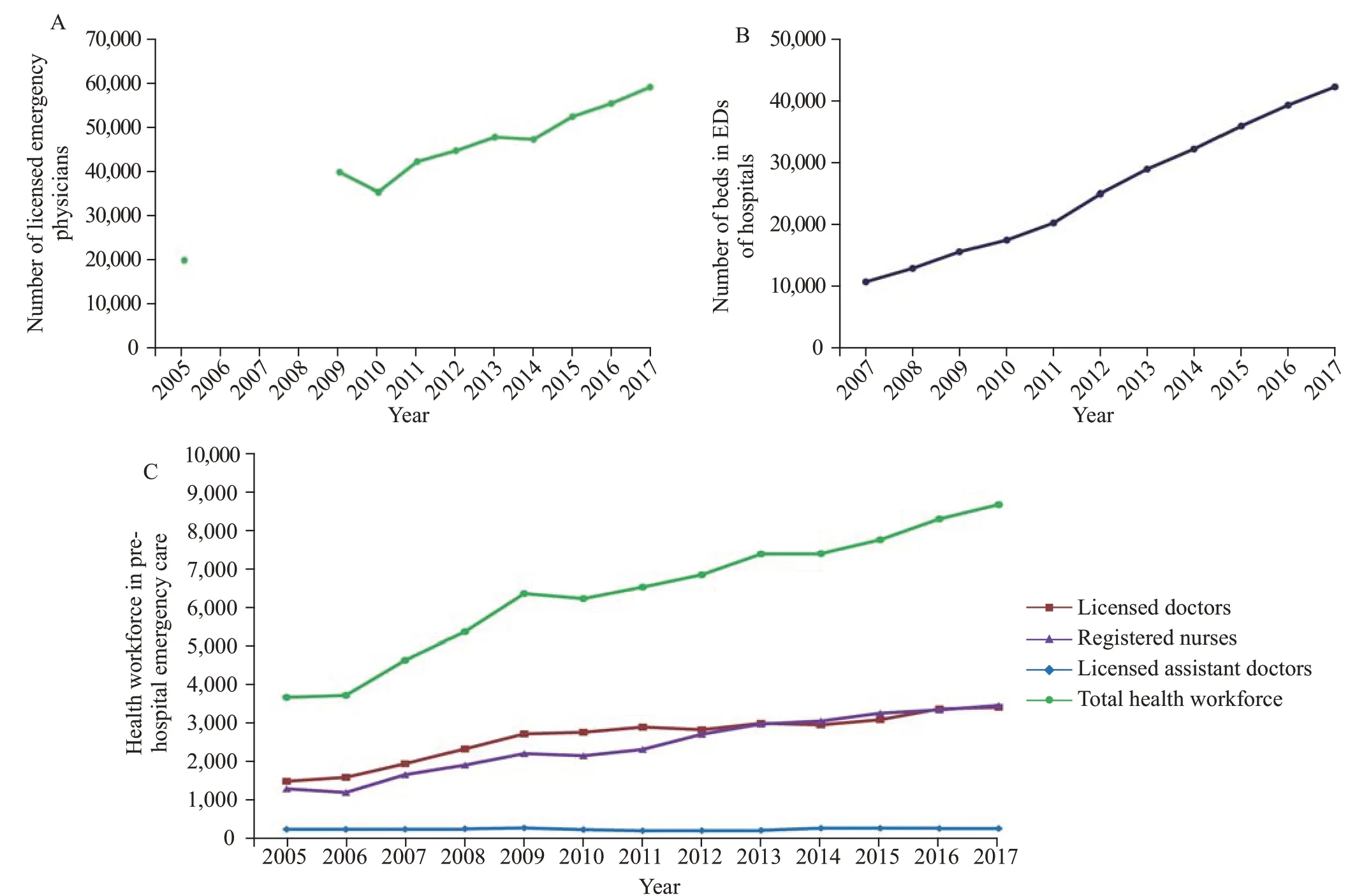
Figure 2. Statistical graphs of changes in workforce and number of beds in EMSS in China. A: over the past decade, the number of licensed emergency physicians at hospitals in China increased by 196%; the data of 2006, 2007, and 2008 were not counted in China’s yearbooks; B: the number of beds in EDs increased from 10,783 in 2007 to 42,367 in 2017; the data before 2007 were not counted in China’s yearbooks; C: for prehospital emergency care, the volume of health workforce doubled, including a 109% increase in the number of physicians. EMSS: emergency medical service system; EDs: emergency departments.
Work exhaustion of emergency workforce
Compared to the USA, China has a higher ratio of emergency physicians per patient capita, with 3.4 in China and 2.9 in the USA in 2015, per 10,000 emergency patients.[15,16]However, exhaustion and burnout remain serious concerns for the Chinese EMSS workforce in the larger hospitals of most regions, who manage an increasingly large population with longer admission time, overcrowding, and medical violence. Workplace exhaustion in China is common with 85% of Chinese physicians reporting medium to high emotional exhaustion scores, and 88% reporting medium to high depersonalization scores.[17]The situation is more severe than that in developed countries, for example, 59% and 66% respectively in the United Kingdom, 46% and 93%in Canada, and 65% with medium to high burnout scores in the USA. Notably, emergency physicians in China reported higher proportions of both scores compared with other physicians.[17,18]As a result of the poor work conditions and lifestyle that result from workforce shortages, many EDs face increasing challenges in staあretention and recruitment. Even among top-ranking EDs in China, nearly 50% of newly recruited physicians commonly come from other departments, and only 10%-20% of undergraduates compared to other disciplines register annually for the graduate admission exam of emergency medicine. Reports in China demonstrated that the low staff retention rate in EDs was a persistent problem.[4,12]Workforce shortages are the most severe in pre-hospital emergency care, with annual staff turnover approaching 50% in large cities such as Beijing, Xi’an,and Shanghai.[11,19-21]Mental exhaustion and consequent staff instability and shortage affect the Chinese medical system overall. The situation is acute in the f ields of the EMSS, similar to pediatrics.[22]
DISCUSSION
In this study, we described and quantified the trends and challenges of EMSS from 2005 to 2017 in China, and found that the number of emergency visits was growing with continually enhancing capabilities during the past decade.However, overcrowding, the long length of stay in EDs, poor work environment, and the work exhaustion of emergency physicians and nurses are still the critical challenges faced by China’s EMSS.
The policies on China’s EMSS were initially developed by the Ministry of Health in the 1980s.[23]China’s EMSS grew very slowly during the first twenty years, but has advanced relatively quickly for the past decade. Because of the accelerating pace of life, unhealthy lifestyles and diets, environmental pollution, the aging process, and more frequent traffic accidents, the annual incidence of virtually all major acute and critical illnesses has been rising in China.[24]In addition, with the expansion of public medical insurance systems, more and more rural residents and rural migrants have gained access to health insurance similar with that of urban residents. As a result, the ED visit rates have been rising among all levels of hospitals in China, from 51.9 million in 2007 to 166.5 million in 2017.As in the USA, the number of ED visits grew faster than the population from 90.8 million in 1992 to 133.2 million in 2012 with a number of reasons, such as the immediate access to diagnostic resources that EDs provide.[25]
To meet the rapid increasing demand and the public health emergencies, a large number of medical resources have been assigned for improving the quality and efficiency of EMSS in China.[26,27]After experiencing the pandemic threats of severe acute respiratory syndrome in 2003, the Chinese government expanded emergency rescue and preparedness via staffing and physical improvements to medical facilities. Thanks to the improved medical resources,the annual mortality of emergency patients decreased from 0.12% in 2005 to 0.08% in 2015.[3]
Despite the expansion of resources and improvements in infrastructure in acute and critical care in China’s EMSS, some substantial challenges still remain, including overcrowding and the long length of stay in EDs, poor work environment, work exhaustion, and consequent instability of emergency workforce. These issues are still critical challenges faced by China’s EMSS, and they could be contributing to the phenomenon that the mortality of EDs was steady and even slightly increased in tertiary hospitals although decreased all over China during the past decade.[3]Not only China, but also the whole developing world and even some developed countries are facing these critical challenges.[18,28-30]
As is the case among many developing and developed countries, overcrowding and significantly increasing throughput in China’s EDs have become widespread,particularly at regional central hospitals.[31]The average length of stay in EDs around China, such as EDs in Beijing,seems similar with that of 15 medical centers from 59 lowand middle-income countries with the median time as long as 7.7 hours.[32]However, this is not satisfactory compared with developed countries, such as the USA. EDs’ overcrowding and the long length of stay are associated with worse quality and safety of emergency care, as well as patients’ morbidity and mortality.[33,34]
Beyond rising patient volumes, the overcrowding and long length of stay in EDs should be also partially attributed to that a large number of Chinese patients are more likely to skip primary care and go directly to tertiary hospitals, and that more people have easier access to EDs especially in tertiary hospitals. In China, people face imbalances in high-quality medical resources, variations in behavioral idiosyncrasies, insufficient inpatient bed capacity, insufficient staff, and limitations driven by medical insurance policies, which are also faced by other developing countries.[35]Secondary to a significant imbalance in medical quality at different hospitals, a weak health referral system, and traditional behavioral patterns,Chinese patients are more likely to avert primary care and go directly to tertiary hospitals, resulting in bed overuse at regional central hospitals and bed underuse at primary care hospitals. At regional central hospitals, the number of beds and the volume of medical personnel are limited.Furthermore, medical insurance systems impose restrictions on medical care, inf luencing mean hospitalization duration,cost, and single-disease expense. The latter restrictions more profoundly affect critically ill patients who usually require longer hospitalization and incur higher medical costs than patients with milder presentations.[31,36]In Chinese emergency medicine, there is a common saying that ref lects this phenomenon: “the front door to the ED is always open even if the back door into the hospital is closed”.
Beyond patient-provider relationships, the provision of high-quality emergency care is often hampered by lack of an adequate workforce, despite the increase of emergency physicians and nurses during the past ten years. Unlike the USA, the emergency physicians in China work alone without emergency technicians and physician extenders such as physician assistants in their teams. Because of a limited workforce managing an increasingly large population with longer admission time, mental and physical exhaustion remains a serious concern for the EMSS workforce,particularly in the larger hospitals of most regions.[27,37,38]The most acute situation in the fields of the EMSS raised concerns about emergency health workers’ endurance and shortages, and quality and efficiency of treating increasing numbers of emergency patients now and in the future.
To face the aforementioned challenges, which are rooted in a rapidly increasing demand against a backdrop of increasingly limited and strained acute care resources, the Chinese EMSS must evolve to advance the “Healthy China 2030” goals. Otherwise, the problems of Chinese EMSS may be more severe. Capabilities of hospitals and providers need to be improved to match the demands of acute care.This includes strengthening the quality improvement and residency training in county-level hospitals, encouraging junior physicians to select emergency care as a specialty career, and increasing medical assistants of EMSS.Broader and sustainable workforce development should be cultured based on policies, such as establishing a safe work environment and increasing available funding. However,it is not enough to only rely on self-directed initiatives by hospitals and medical staff. Public health authorities and the government should increase their focus on this matter. They should design and implement stronger and more efficient targeted plans in the context of broader medical reform,such as strengthening the construction of hierarchical medical treatment system, speeding up the reform of the medical insurance policies, setting up family doctor service system, and strengthening the service capabilities of regional medical centers. Moreover, it is also necessary to take steps to keep people healthier at home, and provide funding for social determinants of health, such as social workers for mental health patients and home care nurses to help with proper administration of medications. It is also necessary to monitor quality and outcomes. The establishment of a national electronic information system and a surveillance tracking system of outcomes in EMSS would be helpful to achieve this target. Encouragingly, China has been implementing some reforms, such as widespread residency training, hierarchical medical treatment system, diagnosis related group payment, general practitioner cultivation, and community health services of family physician model, which should benefit to address these challenges and improve Chinese EMSS.[39-41]
CONCLUSIONS
Over the past decade, the number of emergency visits has grown with continually enhancing capabilities. However,the overcrowding and the long length of stay in EDs, poor work environment, work exhaustion, and consequent staff instability are still the critical challenges faced by China’s EMSS. The study can provide new insights for promoting the quality of emergency care in China, and offer the Chinese experience to the world’s EMSS, especially to other developing countries in similar circumstances.
Funding:This study was supported by National Key R&D Program of China (2017YFC0908700, 2017YFC0908703); Taishan Young Scholar Program of Shandong Province (tsqn20161065,tsqn201812129); Taishan Pandeng Scholar Program of Shandong Province (tspd20181220); National S&T Fundamental Resources Investigation Project (2018FY100600, 2018FY100602); Key R&D Program of Shandong Province (2019GSF108075, 2020SFXGFY03,2017G006013, 2018GSF118003); and Qilu Young Scholar Program.
Ethical approval:Approval from an ethical review board of the hospital was obtained before commencing the study.
Conflicts of interest:The authors confirm that no conflict of interest or any f inancial relationship that relates to the content of the manuscript has been associated with this publication.
Contributors:FX and YGC had the original idea and designed the paper structure. CP and FX drafted the paper. CP, JJP, and KC reviewed the literature, collected the information, analyzed data,and prepared the references. CP produced the f igures. All authors reviewed and approved the f inal version.
杂志排行
World journal of emergency medicine的其它文章
- Factors associated with refractory pain in emergency patients admitted to emergency general surgery
- Identifying critically ill patients at risk of death from coronavirus disease
- Clinical correlates of hypotension in patients with acute organophosphorus poisoning
- Effects of viral infection and microbial diversity on patients with sepsis: A retrospective study based on metagenomic next-generation sequencing
- Effects of metabolic syndrome on onset age and long-term outcomes in patients with acute coronary syndrome
- Predictors of recurrent angina in patients with no need for secondary revascularization
