Acute uterine inversion at cesarean section:an emergency condition in obstetrics
2020-11-27XiaoMeiSunXuWangJinLaiMengXiaoLiuYongZhongGuDepartmentofObstetricsandGynecologyShandongProvincialHospitalAffiliatedtoShandongFirstMedicalUniversityJinan500ShandongChinaDepartmentofAnesthesiologyShandongProvincialHospita
Xiao-Mei Sun,Xu Wang,Jin-Lai Meng,Xiao Liu,Yong-Zhong Gu*Department of Obstetrics and Gynecology,Shandong Provincial Hospital Affiliated to Shandong First Medical University,Jinan 500,Shandong,China.Department of Anesthesiology,Shandong Provincial Hospital Affiliated to Shandong First Medical University,Jinan 500,Shandong,China.
Abstract A 18-year-old local Han Chinese primigravida woman suffered with severe pre-eclampsia.After blood pressure stabilization,convulsion prophylaxis and fetal lung maturity enhancement,emergency cesarean section was performed for inntractable headache at 32 weeks.Uterine inversion spontaneously occured at cesarean section.Immediately,uterine inversion was corrected manually without difficulty.Uterine atony and postpartum haemorrhage did not occur,and the patient made an remarkable recovery.This case report provides residents with excellent case-based learning.The management of uterine inversion requires immediate treatment for uterine repositioning.All staff members in the maternal unit should be updated with skills and knowledge about uterine inversion.
Keywords:Uterine inversion,Emergency condition,Caesarean section,Preeclampsia
Background
Uterine inversion is a rare condition but potentially life-threatening obstetrical emergency.Among women with a uterine inversion,37.7% had an associated postpartum hemorrhage,22.4% received a blood transfusion and 6% required surgical management,however,only 2.8% necessitated a hysterectomy [1].To the best of our knowledge,this condition occur at cesarean section is extremely rare.We hereby report a case of acute uterine inversion at cesarean section.
Case presentation
A 18-year-old primigravida woman,at 32 weeks,applied to Shandong Provincial Hospital with the complaint of headache for 1 week and elevation of blood pressure for 1 day.She had no history of high blood pressure and non-puerperal uterine inversion.Clinical examination showed an anasarca woman with pulse rate of 110 bpm and blood pressure of 169/133 mmHg.The results of blood test showed albumin of 21 g/L and normal levels of blood urea nitrogen (BUN),creatinine(Cr),sodium(Na).Routine obstetrical ultrasound showed no fetal malformation,fundal implantation of the placenta,and mild seroperitoneum.After diagnosis of severe pre-eclampsia was made,She received urapidil by pump for blood pressure stabilization and corticosteroids to enhance fetal lung maturity.Meanwhile,for preventing convulsion prophylaxis,the intravenous regimen of magnesium sulfate (MgSO4) was given as a 4 g dose,followed by a maintenance infusion of 1 to 2 g/h by controlled infusion pump.52 hours after admission,she underwent lower segment caesarean section due to inntractable headache under spinal anesthesia.After delivery of the fetus,about 2 minutes,before oxytocin injection and controlled cord traction,the uterus spontaneously turned inside out with prolapse of the fundus attached by placenta through the incision of the lower uterine segment (Figure 1).The placenta was separated manually from the uterine fundus,then the uterine inversion was corrected manually without difficulty,and 20 units of oxytocin was injected intramuscularly.Uterine atony and postpartum haemorrhage did not occur.During surgery,the heart rate was between 80 and 100 beats per minute,the systolic blood pressure was between 130 and 150 mmHg,and the diastolic blood pressure was between 70 and 100 mmHg.Estimated blood loss was approximately 800 mL.The umbilical cord is about 55 cm long,without wrapping itself around the neck and limbs.The patient made an remarkable recovery.The female neonate appropriated for gestational age with a birth weight of 1,600 grams and a length of 42 cm.APGAR scores were 9 at 1 minute and 10 at 5 minutes.She was discharged from the well baby nursery with no sequlae on day 25.Written informed consent was obtained from the patient for her anonymized information to be published in this article.
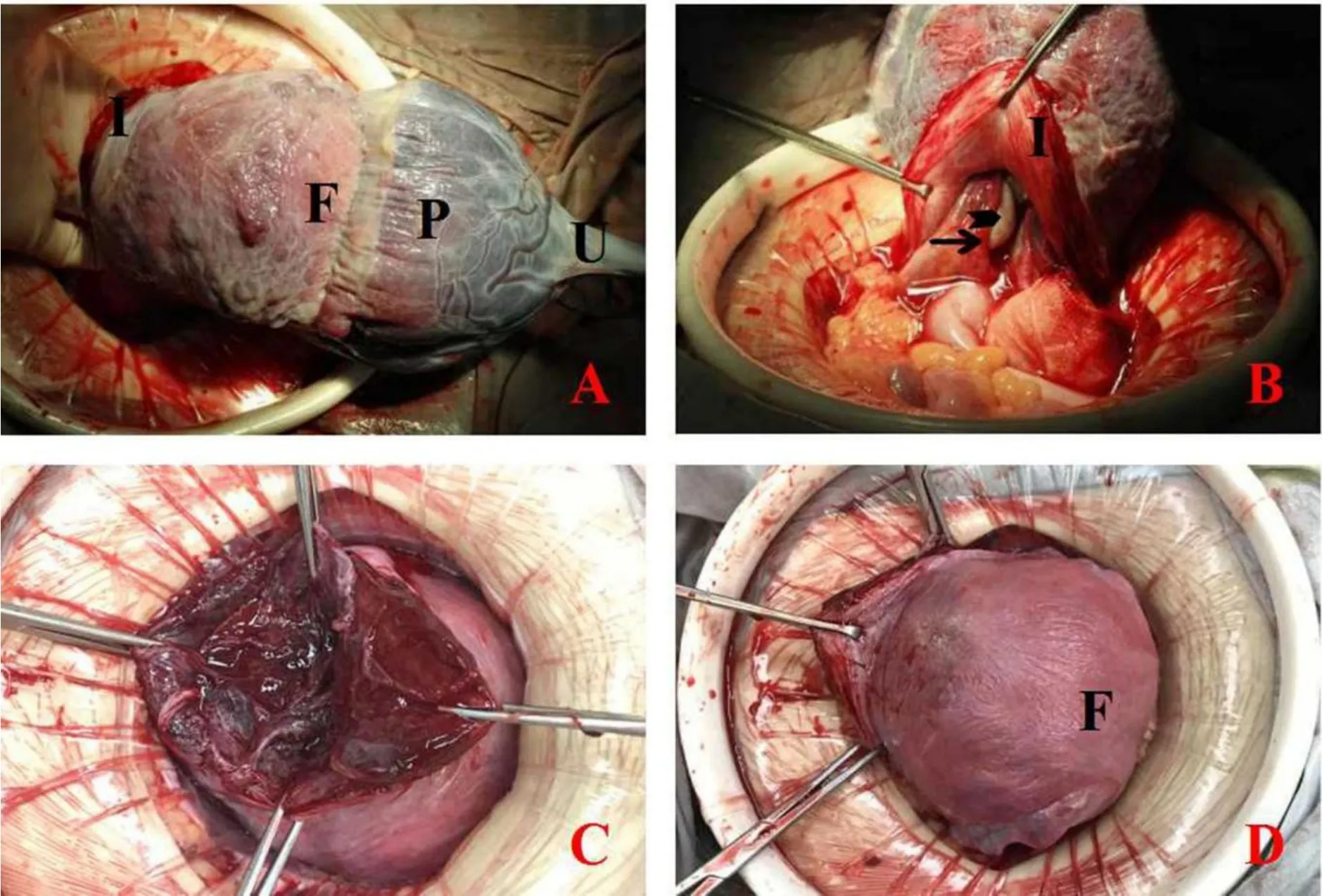
Figure 1 (A) The inverted uterus attached with placenta,seen from abdominal route.(B) Kissing ovaries (arrow head) and tubes (closed arrow) under intraopeative observation.(C) Normal incision of the lower uterine segment appearance after repositioning.(D) Normal uterine contour and appearance after repositioning.(I,incision of the lower uterine segment,F,fundus of uterus,P,unseparated placenta,U,umbilical cord)
Discussion
Acute inversion of the uterus following delivery is a rare event and even more rare during caesarean delivery[2].The incidence of uterine inversion is reported as 2.9 per 10,000 deliveries[1].The etiology is not well understood,and in as many as 50%of cases,no precipitating factor can be identified[3].The most common risk factors include morbidly adherent placenta,short umbilical cord,congenital weakness of the uterine wall or cervix,weakening of the uterine wall at the placental implantation site,fundal implantation of the placenta,uterine tumors,uterine atony,sudden uterine emptying,fetal macrosomia,manual removal of the placenta,inappropriate fundal pressure,excessive cord traction,and the use of uterotonic agents prior to placental removal[4].In this case,the patient was a primigravida with a single pregnancy of normal caesarean section surgical procedure with placenta fundal implantation.Primiparity has also long been proposed as a risk factor,primarily due to the increased incidence of placenta fundal implantation in this population[5].Hence,complete placenta fundally attached was one reasonable explanation for the cause of uterine inversion.
MgSO4was used to prevent and treat seizures in women with preeclampsia or eclampsia,it also used for fetal neuroprotection before anticipated early preterm [6].Several cases of uterine inversion receiving MgSO4for the diagnosis of preeclampsia have been reported [7].In this case,MgSO4was applied several hours before surgery to prevent the onset of eclampsia.Hence,uterine hypotonia secondary to application of MgSO4was another reasonable explanation for the cause of uterine inversion.
The diagnosis of uterine inversion is usually based on clinical signs and symptoms,such as severe lower abdominal pain,haemorrhage and severe shock.In cases of subacute or chronic inversion,the symptom was atypical,which lead to unclear diagnose.Ultrasound and magnetic resonance imaging (MRI)have proven to be effective diagnostic methods [8,9].In this case,during caesarean delivery,the uterine inversion contour is directly visualized and is fairly easy to make the diagnosis.
Treatment options for this obstetric complication also varied which depend upon the judgment and skills of surgeon.Management should include resuscitation of maternal hypovolemic shock,as well as repositioning of the inverted uterine fundus.Abdominal operation procedures (Huntington and Haultain techniques) and vaginal approach procedures(Kustner and Spinelli techniques) are commonly used for reverting the uterus.In Haultain techniques,a horizontal hysterotomy,5 to 6 cm in length,was made in the posterior portion of the lower uterine wall through the cervical ring.This technique allowed easier facilitation of uterine repositioning [3].In case of uterine inversion at cesarean section,the inverse ring was the incision of anterior of the lower uterine wall.As thus,the down and outside uterine fundus was inverted to upside and inside through the incision of the lower uterine segment easily under the existing regional anesthesia,without subsequent complications.By reviewing the literature,we identified 30 cases of acute uterine inversion at cesarean delivery,in most cases of acute uterine inversion an existent uterine incision and anesthesia allows re-inversion of the uterus to be accomplished immediately,8 (26.7%)reported postpartum hemorrhage,6 (20%) reported uterine atony.If a delay in diagnosis or re-inversion occurs,the outcome may be critical and result in maternal death [10].The possibility of amniotic fluid embolism should be considered,when hypotension unrelated to the extent of the initial blood loss and coagulopathy only than to be followed by uterine atony[11].The prevention of uterine inversion was mentioned by a randomized controlled trial designed by Deneux-Tharaux et al.[12],and the results showed that controlled cord traction did not increase the incidence of uterine inversion,and reinversion in a subsequent pregnancy is unpredictable.
Because of uterine inversion requires a prompt diagnosis and immediate treatment for uterine repositioning [13].In this case,although the surgeon was a fresh chief resident,he has been trained well in skills and knowledge about uterine inversion.All staff members in the maternal unit should be updated with skills and knowledge about uterine inversion.
杂志排行
Clinical Research Communications的其它文章
- The prognostic value of baseline circulating tumor cells in patients with metastatic breast cancer:a meta-analysis
- Meta-analysis of the clinical efficacy and safety of Urinary Kallidinogenase in the treatment of acute cerebral infarction
- Candidate genes associated with cold-coagulation or heataccumulation blood stasis syndrome in hypertension
- Research on the aetiology and treatment of premature ovarian insufficiency