Analysis of the evidence of related factors,associated conditions and at-risk populations of the NANDA-I nursing diagnosis insomnia
2020-11-26LidiSntigoGundliniEdurdFerreirSilvJulindeLimLopesViniciusBtistSntosCmilTkoLopesAlbciBotturLeitedeBrros
Lidi Sntigo Gundlini ,Edurd Ferreir d Silv ,Julin de Lim Lopes ,Vinicius Btist Sntos ,Cmil Tko Lopes ,Alb Lúci Bottur Leite de Brros ,*
a Escola Paulista de Enfermagem,Universidade Federal de S~ao Paulo,S~ao Paulo,Brazil
b S~ao Paulo Hospital,S~ao Paulo,Brazil
Keywords:Adult Insomnia Nursing diagnosis Sleep initiation and maintenance disorders
ABSTRACT Objectives:To summarize evidence in the literature on the predictors of insomnia in adults and to determine correspondences with diagnostic indicators of the NANDA-I diagnosis Insomnia.Methods:An integrative review performed in Pubmed,Virtual Health Library and CINAHL.Forty-eight articles published in Portuguese,English or Spanish from 2011 to 2018 were included.An analysis of correspondence between the predictors and the NANDA-I related factors and associated conditions for Insomnia was performed.Results:There was a correspondence of the predictors found in this review with NANDA-I related factors and associated conditions,except for grieving and frequent naps during the day.Smoking,caffeine intake,dysfunctional sleep beliefs,obesity and caregiver role strain are possible new related factors;chronic illness is a possible new associated condition and individuals going through changes in marital status,economically disadvantaged,female gender,increasing age and night shift worker are possible new at-risk populations.Conclusion:The predictors of insomnia that had a correspondence with the NANDA-I elements can support the evidence base of the nursing diagnosis.The predictors found without a correspondence with the diagnosis can be considered for inclusion in the NANDA-I classification,thereby supporting the clinical reasoning of nurses and students.
What is known?
· Insomnia is highly prevalent in adults and older adults,directly impacting the development of other health dysfunctionalities.NANDA International diagnosis Insomnia was included in the classification in 2006 and only revised for phrase refinement in 2017.Thereby,it requires updated evidence on its diagnostic indicators.
What is new?
· All clinical indicators of the NANDA International diagnosis Insomnia are supported by current literature,except for two.New possible indicators have been identified that can assist nursing students and nurses in improving clinical reasoning.
1.Introduction
Sleep disorders,especially insomnia,are common health problems and risk factors to further health disturbances that negatively affect the quality of life,such as impaired immune system,depression,increased irritability,risk-prone sexual activity,suicidal ideation,ineffective performance at work,study,social and family relationships,and an increased risk of accidents at work or automobile accidents [1-3].A US populational-based study found that approximately one-third of a sample of 1,000 adults reported having one or more of insomnia symptoms,such as difficulty initiating sleep,difficulty staying asleep,waking up too early and in some cases non-restorative or poor sleep[4].Among patients with chronic pain conditions,65.3% have clinical insomnia,including mild,moderate and severe degrees [5].
Considering that sleep disorders are common and also a cause of further health issues,nurses are expected to be aware of their possible causes,in order to early recognize them and support the proposal of interventions to minimize them.From a nursing perspective,insomnia can be considered a human response to a health condition or a life process,i.e.,a nursing diagnosis.The NANDA International,Inc.(NANDA-I) Diagnosis Classification defines Insomnia(code 00095)as a disruption in amount and quality of sleep that impairs functioning [6].
NANDA-I diagnoses have different diagnostic indicators functioning as antecedents.Related factors(ReF)are possible causes or contributing factors that are amenable to independent nursing interventions.Associated conditions (AC) are medical diagnoses,injury procedures,medical devices,or pharmaceutical agents,which are not modifiable by nurses.At-risk populations (ARP) are groups of people who share a characteristic that causes each member to be susceptible to a particular human response,but are not independently modifiable by the nurses [6].
Insomnia currently has 11 ReF:anxiety,environmental barrier,frequent naps,alcohol consumption,depression,physical discomfort,stressors,inadequate sleep hygiene,average daily physical activity is less than recommended for gender age and,fear and grieving.It also has two AC:pharmaceutical agents and hormonal change [6].No ARP are currently included.
In order to have a terminology at an appropriate level of evidence to represent the current strength of nursing knowledge,the NANDA-I Classification requires continuous updating by studies on the diagnostic indicators.These studies can be submitted to appreciation by the Diagnosis Development Committee and be adopted by the Classification [7].Because Insomnia was approved by NANDA-I in 2006 and only revised for phrase refinement in 2017,it requires updated evidence on its diagnostic indicators.The aims of this study were to summarize evidence in the literature on the predictors of insomnia in adults and to determine correspondences with diagnostic indicators of the NANDA-I diagnosis Insomnia.
2.Material and methods
This study was performed in two phases,summarized in Fig.1.
2.1.First phase
An integrative literature review was performed by following Whittemore and Knafl’s method [8],which includes problem identification,literature search,data evaluation,data analysis and presentation of findings.
2.1.1.Problem identification
A research question was formulated according to the PEO framework(P -patient (adults); E -exposure (possible causes or risk factors); O -outcomes (insomnia)):“What are the causes or risk factors for insomnia in adults?”
2.1.2.Literature search
The search was conducted in Pubmed,the Virtual Health Library and CINAHL,by using combinations of Medical Subject Headings(MeSH),CINAHL titles,Health Sciences Descriptors (DeCS) and keywords (non-standardized terms).The search strategy was:((((((Risk factors[Mesh Terms]) OR Causality[Mesh Terms]) OR Etiology[Title/Abstract]) OR Cause$[Title/Abstract]) OR Risk factor$[-Title/Abstract]))AND(((Sleep Initiation and Maintenance Disorders[Mesh Terms])) OR Insomnia[Title/Abstract]).
The review included cross-sectional and longitudinal studies published from 2011 to 2018 in either English,Spanish or Portuguese,having as independent variables possible causes/risk factors for the dependent variable insomnia and analyzing the results through multivariate analyses.We excluded studies that did not specify insomnia among various sleep disorders studied or those that studied poor sleep quality.
2.1.3.Data evaluation
Two independent investigators read all titles and abstracts.After selection by title,the researchers read the abstracts to ensure that the studies met the inclusion criteria.Then,the selected articles were fully read for extraction of the data of interest.
2.1.4.Data analysis
Once the studies were included,their levels of evidence were evaluated according to the classification of the Oxford Center for Evidence-based Medicine for aetiology:Level 1a,systematic review with homogeneity of randomized control trials (RCTs); Level 1b,individual RCT;Level 2a,systematic review of cohort studies;Level 2b,individual cohort study (including low quality RCT; e.g.,<80%follow-up); Level 3b,individual case-control study; Level 4:Caseseries (and poor quality cohort and case-control studies); Level 5:Expert opinion without explicit critical appraisal,or based on physiology,bench research or“first principles”.Because the Oxford Center does not classify cross-sectional studies,but level 4 includes studies that “failed to carry out a sufficiently long and complete follow-up of patients” [9],cross-sectional studies were assigned a Level 4,as previously performed by Teixeira et al.[10].
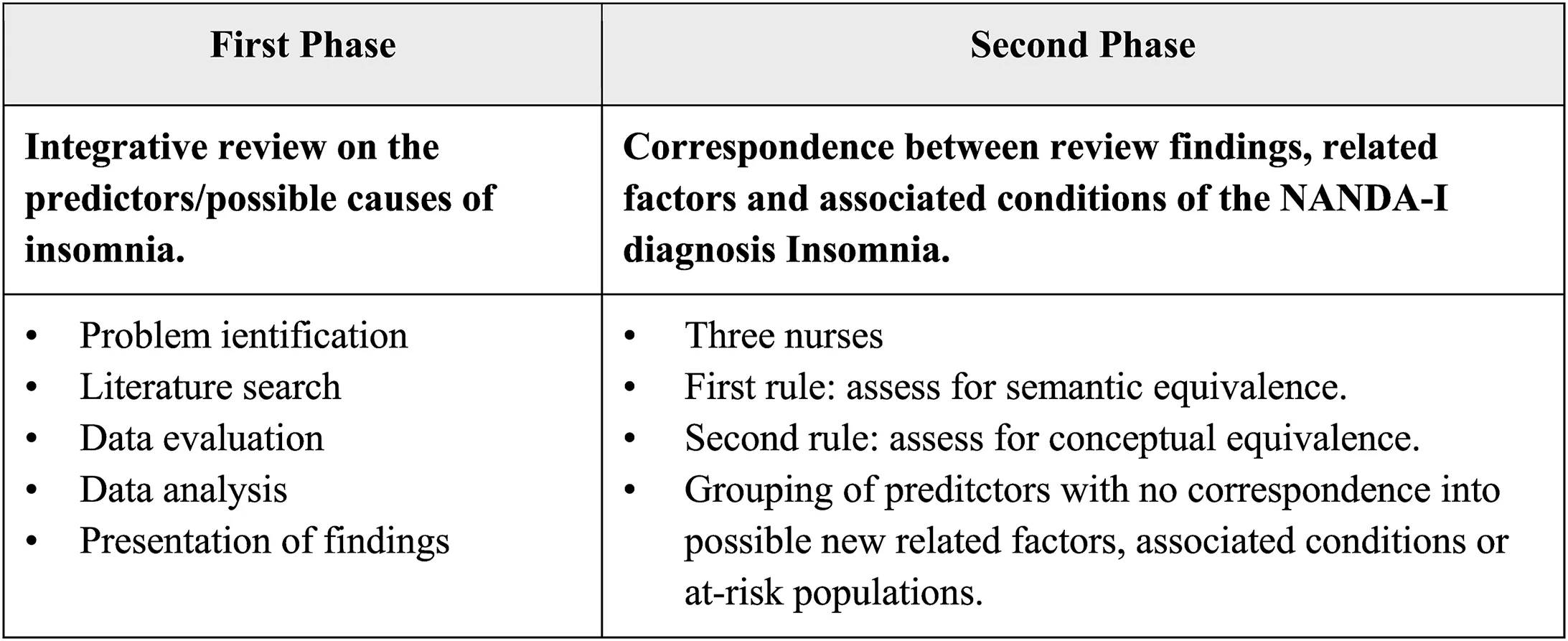
Fig.1.Summary of the methodological steps.
2.1.5.Presentation of findings
The studies included were summarized in a table with the following data:design,level of evidence,number of participants,instruments to evaluate the insomnia and the predictors of insomnia.
2.2.Second phase
Based on the predictors identified,their correspondence with the ReF and AC of the diagnosis of diagnosis Insomnia was evaluated [11].The analysis was performed by three nurses by considering the concepts in the ReF and AC.Two were doctorate-prepared nurses with academic and professional expertise in classification systems for over 15 years and the third nurse was an MsC candidate.The analysis followed two rules.First rule:Assess for semantic equivalence between the predictors identified in the literature with the ReF and AC of Insomnia in the NANDA-I classification; Second rule:Assess for conceptual equivalence between the predictors identified in the literature and their correlation with the ReF and AC through the researchers’expertise.The allocation of terms required a 100% consensus among researchers.
After the analysis,the indicators identified in the review without a correspondence with the ReF or AC of the diagnosis Insomnia were grouped as proposals of new ReF,AC or ARP for incorporation into the NANDA-I classification.In addition,populations with a high frequency of insomnia were also considered possible new ARP.
3.Results
One thousand and one articles were found,out of which 48 were included in the review (Fig.2).Thirty-eight were cross-sectional studies and ten were prospective longitudinal studies.The characteristics of the studies included are shown in Table 1.
The number of participants ranged from 94[12]to 57,207 adults[13].The follow-up period in the longitudinal studies ranged from 6 months [14]to 12 years [15],see Table 1.
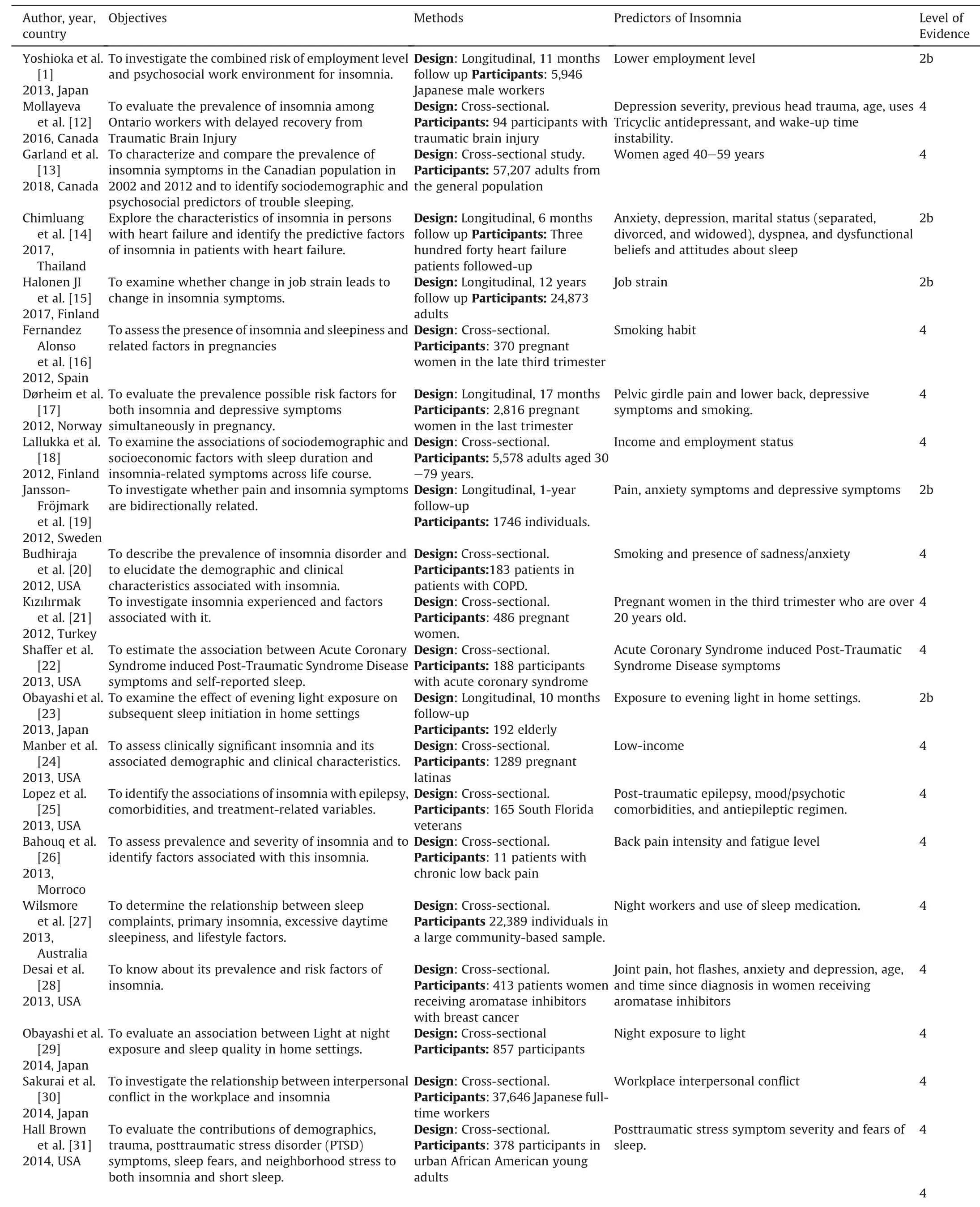
Table 1 Predictors of Insomnia found in the literature.
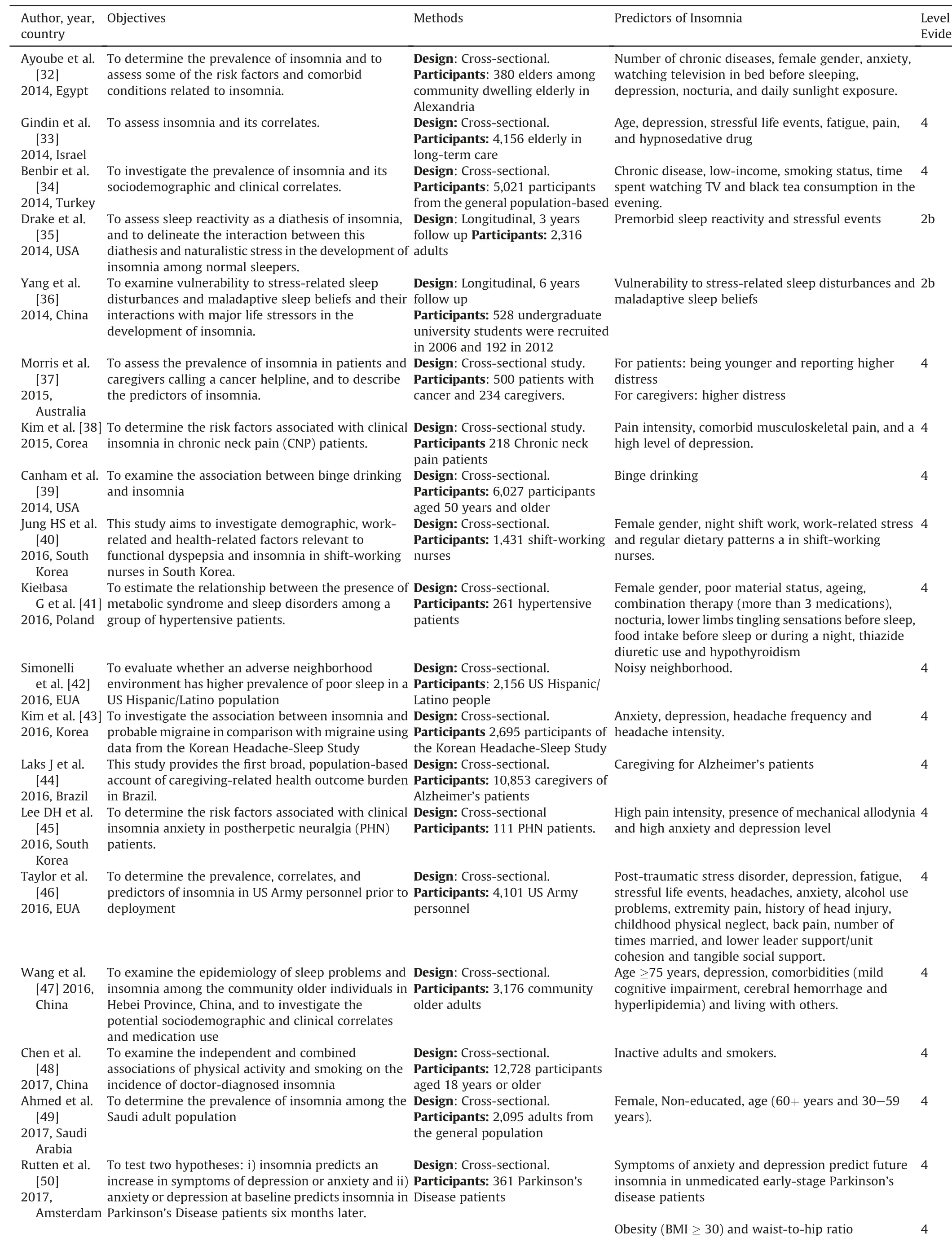
Table 1 (continued)
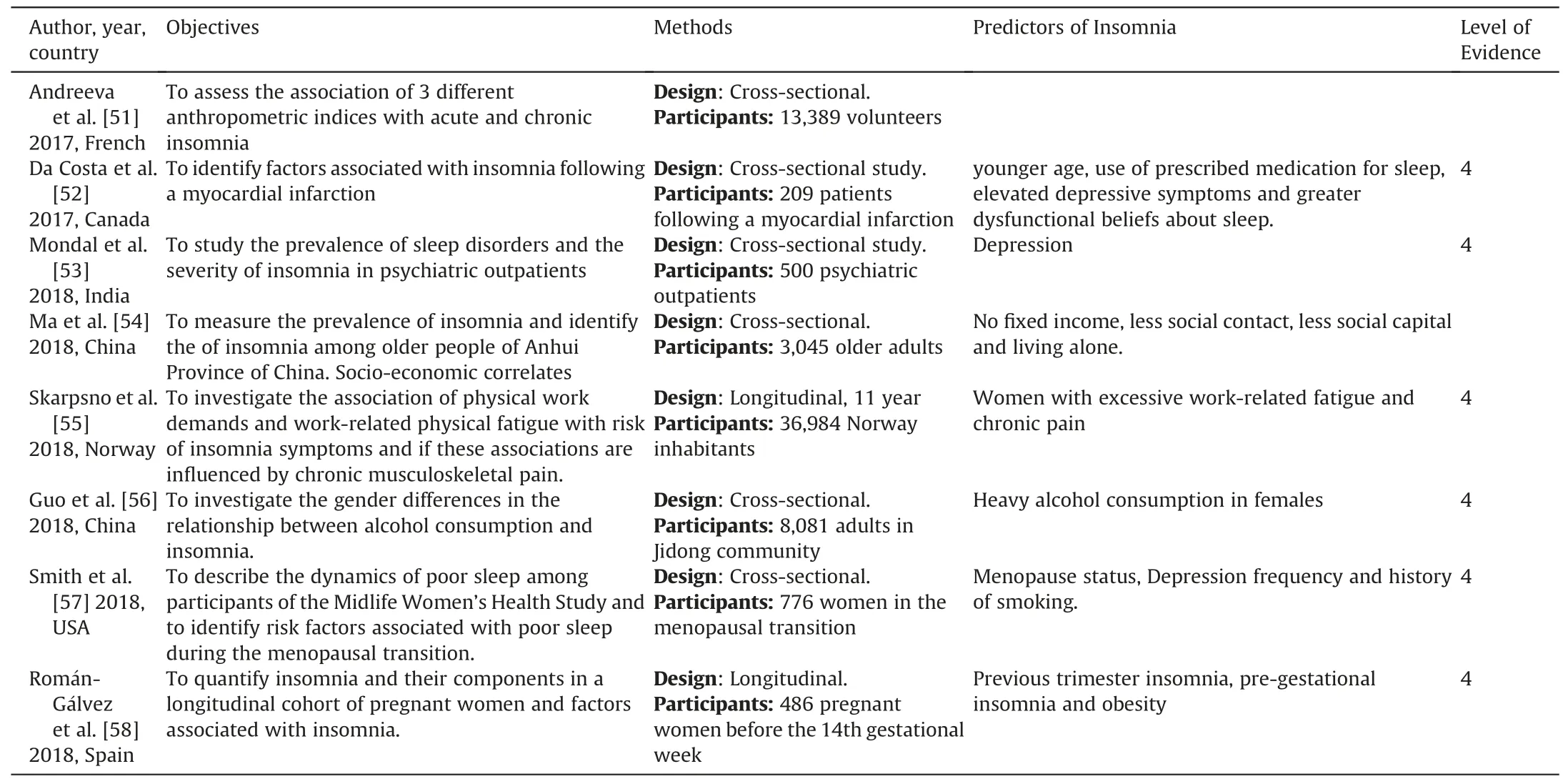
Table 1 (continued)
The most frequently used instruments for the assessment of insomnia were Athens Insomnia Scale (AIS),Pittsburgh Sleep Quality Index (PSQI),Insomnia Severity Index (ISI),Diagnostic Criteria for Primary Insomnia(DSM-IV),International Classification of Sleep Disorders (ICSD),Women’s Health Initiative Insomnia Rating Scale (WHIIRS) and Bergen Insomnia Scale (BIS) (Table 1).
There were several studied populations,mainly adults in general,older adults,and pregnant women.Groups of patients with diseases included those who abuse alcohol,patients with chronic obstructive pulmonary disease,cancer,postherpetic neuralgia,Parkinson’s Disease,psychiatric disorders,chronic musculoskeletal pain,heart failure,late recovery from traumatic brain injury,and hypertension.Other groups included young adults in general,war veterans,undergraduate university students,army personnel,women in the menopausal transition,caregivers of Alzheimer’s patients,and workers.
Considering all the studies,the most common predictors were depression (19 studies),physical discomfort (19 studies),stressors(11 studies) and increasing age (10 studies).All the ReF and AC of the NANDA-I diagnosis were supported by the study findings,except for frequent naps and grieving (Table 2).
After grouping of the predictors that did not have a correspondence with the NANDA-I diagnosis,the new possible ReF identified were smoking,caffeine intake,dysfunctional sleep beliefs,obesity and caregiver role strain.The possible new AC were chronic illness.The possible new ARP identified were individuals going through changes in marital status,economically disadvantaged,female gender,increasing age and night shift work(Table 3).
4.Discussion
This study identified possible causes and predictors of insomnia in adults and determined their correspondences with diagnostic indicators of the NANDA-I diagnosis Insomnia.In addition,new possible indicators were proposed.In the literature search,a relevant number of studies were retrieved,ranging from small to significant samples.The variety of populations investigated reinforces the epidemiological importance of insomnia.Although the followup period in longitudinal studies was as great as 12 years,most studies were cross-sectional.Further longitudinal studies that establish causal relationships between independent variables and insomnia are required.There was a wide variation in the frequency of insomnia symptoms,possibly due to the use of different instruments to investigate the phenomenon.
Most of the current ReF and AC of the diagnosis Insomnia were supported by the literature,but no studies were found that investigated frequent naps or grieving as possible predictors of insomnia.This apparent lack of evidence might be related to the limitations of our literature review.A search strategy using terms for each possible risk factors/cause of insomnia might have retrieved other studies specifically about each risk factor.Extended period limits,other databases,and inclusion of other idioms might also be accounted for this result.It is also likely that the predictive relationship between grieving and insomnia has not been recently studied,because it has been widely established that insomnia is a common symptom in the grief response[59].
The relationship between frequent naps and insomnia might also have been investigated through other statistical methods,such as correlation analysis and analysis of covariance [60],therefore they did not meet our inclusion criteria.In a recent populationbased Canadian study with 2468 community-dwelling elderly persons,self-reported naps were not significantly associated with sleep efficiency,in both the non-adjusted and fully adjusted model[61].On the other hand,Jang et al.suggest that napping might have a negative effect on sleep maintenance only for insomnia patients,but not for normal controls,based on both self-reported sleep and actigraphy-measured sleep [62].That would be explained by hyperarousal during periods of insomnia,which leads to underestimation of sleep amount and quality.Consequently,patients with insomnia might extend their time in bed or take naps to compensate for poor sleep.This safety behavior is considered counterproductive and may exacerbate insomnia[63].Given this bidirectional relationship between napping and insomnia,we would argue that frequent naps is not only a ReF of the NANDA-I diagnosis Insomnia,but it could also be a defining characteristic.
Some predictors of Insomnia were identified that were not related to the clinical indicators of the nursing diagnosis.Some ofthese predictors were classified as ReF,because they are amenable to independent nursing interventions.Other predictors were classified as associated conditions because they are directly related to medical conditions,whereas the remaining predictors were classified as at-risk populations [6].
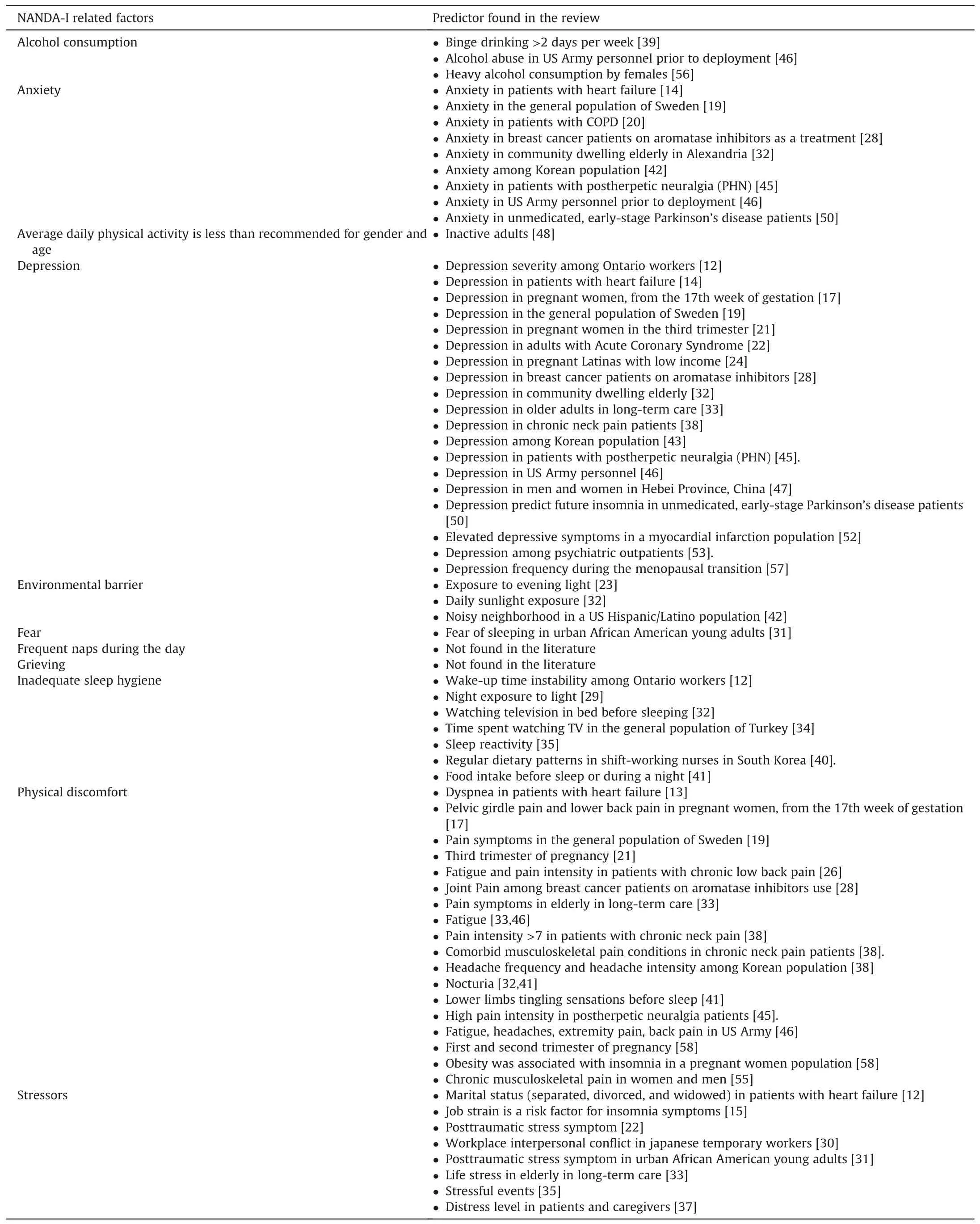
Table 2 Correspondences between NANDA-I related factors or associated conditions and the predictors of insomnia found in the literature.
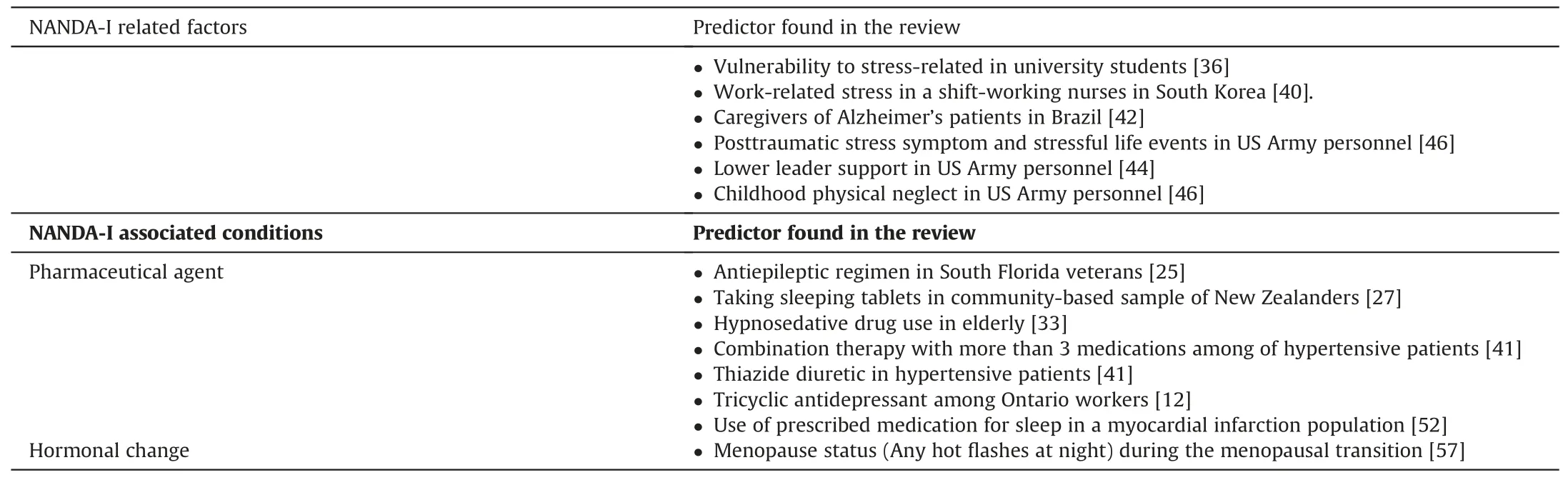
Table 2 (continued)
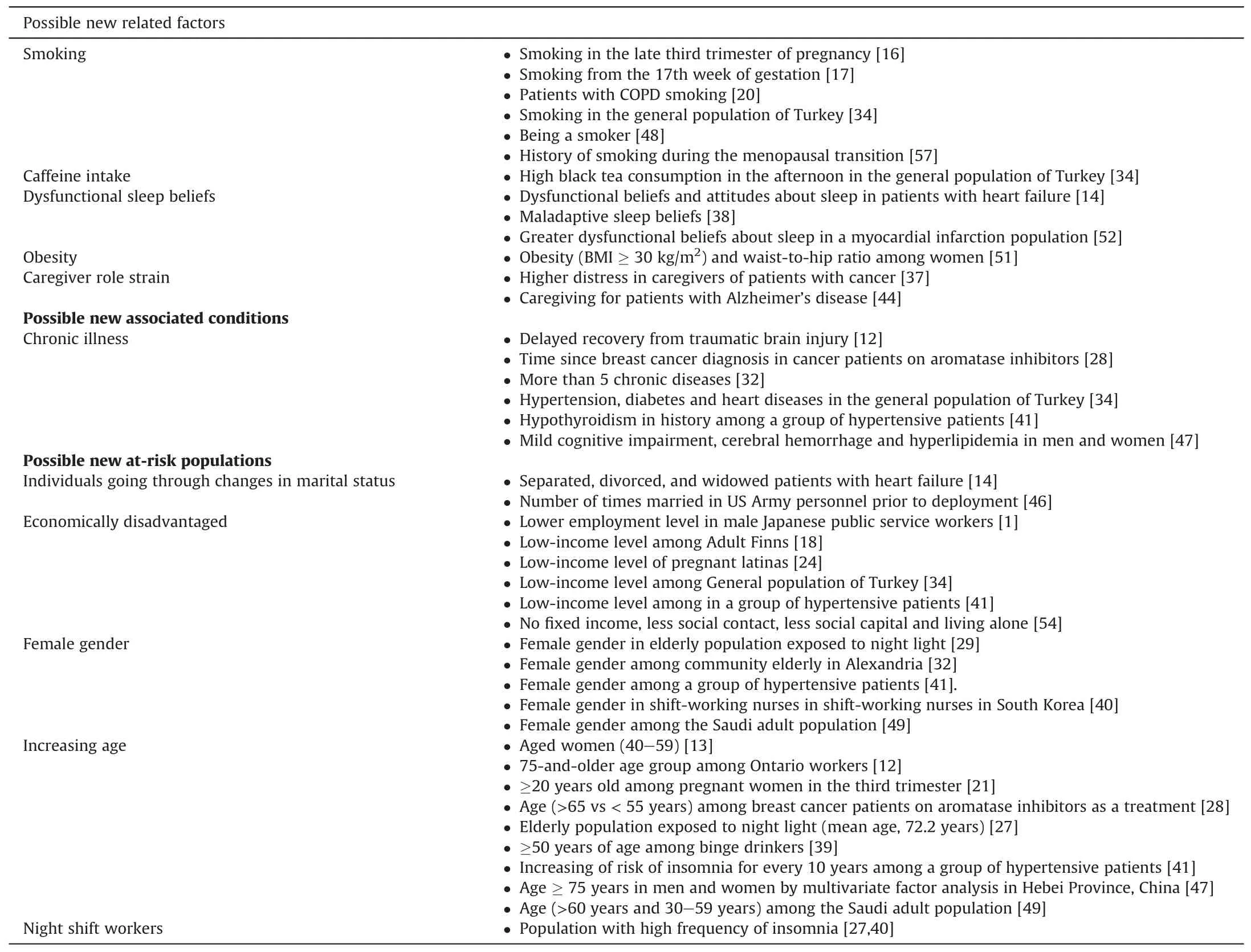
Table 3 Possible new related factors,associated conditions and at-risk populations of the Nursing diagnoses Insomnia.
Smoking was found in six studies and classified as a possible new ReF of Insomnia,since there is evidence on independent nursing interventions aimed at smoking cessation,such as Smoking Cessation Assistance (code 4490) of the Nursing Interventions Classification (NIC) [64].Smoking as a predictor for Insomnia was identified along with other indicators,such as depression [16,57],anxiety[19],poor sleep hygiene[33,47].In a study carried out with 77 young people,it was found that smokers had a shorter sleep continuity with increased wake time after sleep onset,which may be caused by the hypothalamic-pituitary-adrenocortical axis [65].
Other predictors that did not correspond to the NANDA-I diagnosis were obesity,caffeine intake,dysfunctional sleep beliefs and caregiver stress,which were classified in the present study as ReF.Possible interventions to address these ReF are included in NIC in the Behavioral domain,in the classes Behavior therapy,Cognitive therapy,Patient education [64],as well as and in a review on insomnia and sleep [66].Although we identified obesity as a predictor of insomnia[51],a meta-analysis including 67 studies did not confirm this association.Thereby,more robust studies are needed to evaluate this association [67].
The predictor most commonly found that was also not a match with the Insomnia diagnosis was “increasing age”,which was classified as an ARP.Possible causes for increased occurrence of insomnia in this population are inadequate sleep hygiene (27),chronic comorbidities,depression [11,20,27,45],anxiety [27],stressors,physical discomfort [20,27,40,66,68].
“Economically disadvantaged” as an ARP was identified in six studies.Other elements associated with this ARP were depression[24],inadequate sleep hygiene[34],food intake before bedtime[41]and pain [41].Economic disadvantages can lead to depression,worsening of clinical signs such as pain and attitudes that do not favor the quality of sleep.Another study with 706 individuals also found that individuals with low income are more vulnerable to the deleterious effects of exposure to noise,thereby impairing their sleep quality [69].
The female gender was found in several studies as a predictor of insomnia[66]including a meta-analysis that found that insomnia is 1.5-fold more common in women than in men[70].This predictor was classified as an ARP.In some studies,women with insomnia frequently had hypertension [41],were elderly [29,32]and night workers [40].The relationship between female gender and insomnia can also be related to lower educational levels,unemployment,hormonal factors and psychological factors such as perfectionism and anxiety,which are more frequent in women[71].
Other predictors identified that were categorized as ARP for the nursing diagnosis were changes in marital status and night shifts.In a study conducted with 35,228 people,divorced men and women had more insomnia symptoms [72].In a study with 494 participants,night workers had poorer sleep quality,longer sleep latency,shorter sleep duration,more sleep disorders and greater dysfunction during the day[73].
Chronic diseases were also predictors identified that were not included in the NANDA-I diagnosis and were classified in this study as AC.Those are situations that cannot be modified by independent nursing interventions.Other situations associated with chronic diseases that are predictive of insomnia and can be managed by nurses are anxiety [28],depression [28,32],smoking,and caffeine intake [34].
As the nursing science evolves,constant content refinement of the NANDA-I diagnoses is expected.The predictors found in this study can be submitted to the NANDA-I appreciation for inclusion in the Classification,thereby supporting clinical reasoning related to the causes of Insomnia.Further studies can be developed to investigate the predisposing,disabling,precipitating,or reinforcing nature of the diagnostic Ref [74],as well as to test interventions toward these factors.
5.Conclusion
Several predictors of insomnia in adults were identified in different populations.All ReF and AC of the current nursing diagnosis Insomnia are supported by the literature,except for“frequent day napping” and “grieving”.We found five possible new ReF,one possible new AC and five possible new at-risk populations,which can be submitted for NANDA-I appreciation and inclusion in the Classification.
Relevance for clinical practice
Awareness of the predictors of insomnia can support nurses in the early identification and support for patients’ needs.The predictors found in this study can be submitted to the NANDA-I appreciation for inclusion in the Classification,thereby supporting clinical reasoning related to the causes of Insomnia.
Funding
The Brazilian National Council for Scientific and Technological Development (CNPq).
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2020.09.003.
杂志排行
International Journal of Nursing Sciences的其它文章
- An exploration of the breastfeeding behaviors of women after cesarean section:A qualitative study
- The risk factors of postpartum urinary retention after vaginal delivery:A systematic review
- Demands of experiential training for ICU nurses in Hunan of China
- Understanding autism spectrum disorder and coping mechanism by parents:An explorative study
- Association of swallowing problems with frailty in Chinese hospitalized older patients
- Theory-guided interventions for Chinese patients to adapt to heart failure:A quasi-experimental study
