Association of swallowing problems with frailty in Chinese hospitalized older patients
2020-11-26TintinWngYnweiZhoAiminGuo
Tintin Wng ,Ynwei Zho ,Aimin Guo
a Department of Nursing,Chinese Academy of Medical Sciences & Peking Union Medical College,Peking Union Medical College Hospital,Beijing,China
b School of Nursing,Peking Union Medical College,Beijing,China
Keywords:Aged Deglutition Deglutition disorders Frailty Inpatients
ABSTRACT Objective:To estimate the prevalence of dysphagia and frailty among hospitalized older patients and to analyze the relationship between dysphagia and frailty in these people.Methods:Data were collected on 386 participants aged 65 and older in a general hospital from April to December 2017.Patients were asked to complete a self-designed demographic questionnaire.Frailty and swallowing function assessments were performed using the Fried frailty phenotype and the 30-ml water swallowing test,respectively.Multiple stepwise logistic regression analyses were used to identify the association between frailty and dysphagia.Results:Dysphagia developed in 31.1% of older people,and 24.4% developed frailty.Frailty was statistically significantly related with dysphagia.Dysphagia was more prevalent in frail and pre-frail patients(48.9%and 32.4%,respectively)than those who were non-frail(13.6%).In multivariate analyses,frail(OR,5.420; 95% CI,2.684-10.944;P<0.001) and history of choking/coughing while drinking(OR,2.954;95% CI,1.844-4.733;P<0.001)were associated with dysphagia.result.Conclusions:Frailty is associated with dysphagia.More attention should be paid to frailty and dysphagia of the elderly and further studies are needed to evaluate the correlated mechanism and develop targeted nursing interventions.
What is known?
· Dysphagia is a major health problem among older individuals.
· The relationship between dysphagia and frailty warrants further investigation.
What is new?
· A high proportion of dysphagia occurred in older people suggests that the swallowing function in the elderly cannot be ignored.
· We found that frailty was associated with dysphagia.Dysphagia was more prevalent in frail and pre-frail patients than in those who were non-frail.
1.Introduction
Dysphagia is a major health problem among older individuals.Prevalence of dysphagia increases with age and is highly prevalent in older people.The European Society for Swallowing Disorders-European Union Geriatric Medicine indicated oropharyngeal dysphagia should be given more attention as a geriatric syndrome[1].It has been reported that 10%-27% of community-dwelling elders [2-4]and 40%-60% of nursing home residents [5]have clinical symptoms.Dysphagia can cause severe medical outcomes in elderly people,including dehydration,malnutrition,aspiration pneumonia,and hospitalization.Dysphagia has been classified as a digestive condition in the International Classification of Diseases(ICD-10).There are a variety of diseases that can lead to swallowing disorders.Neurological diseases,dementia including Alzheimer’s disease,Parkinson’s disease,and stroke are the most common causes of dysphagia.However,it can also occur in people with underlying disease,such as advancing age[6].
Numerous studies have described the impact of age on swallowing function [2,6].Presbyphagia,characterized by age-related changes in the swallowing mechanism,increases the risk of developing dysphagia [7].All these progressive alterations on swallowing function in healthy older people,including reductions in muscle mass and connective tissue elasticity and impaired dental status,can negatively impact safety and efficiency of swallowing and may contribute to dysphagia.
Older people are large users of hospital care[8].Hospitalization increased the risk of adverse outcomes[9].According to studies of dysphagia [10,11],the dysphagia referral rates of the elderly increased an average of 63%from 2007 to 2014,especially for those who are above the age of 60.This population is they are often admitted to hospital due to acute condition and are more susceptible to swallowing disorders.Thus,it is necessary to assess and screen dysphagia for hospitalized older patients.
Frailty is a state of increased vulnerability following stress and increases steadily with age [12]; it is regarded as one of the important geriatric syndromes.Frail elderly adults invariably have multi-organ problems,associated with adverse outcomes,including falls,disability,hospitalization,and mortality.Loss of skeletal muscle mass and strength have been considered as an important component of frailty [13].Also,muscle mass decreases during aging,which may affect the muscles involved in swallowing[14].The human tongue is extremely essential in mastication,swallowing and speech.The lack of tongue strength is likely to be a manifestation of age-related loss of muscle function[15].Decreased tongue pressure was related to or correlated with sarcopenia or the cause of sarcopenia[16],which may increase the risk of dysphagia in the elderly.Otherwise,sarcopenia is the loss of the muscle mass and function and overlaps with frailty.Therefore,maybe there is a correlation between dysphagia and frailty.Frailty or its components(hand grip strength,gait speed) has been reported in previous studies as one of the related factors contributing to prevalence of dysphagia [4,17-19].However,there is no agreement with the conclusions,and these studies are limited with participants and various frailty assessment tools.Therefore,we aimed to investigate the relationship between dysphagia and frailty in hospitalized older patients and to evaluate whether frailty increases the risk of dysphagia.
2.Materials and methods
2.1.Participants
A total of 402 participants were recruited from Peking Union Medical College Hospital,Beijing,China.Among these patients,386 were screened for eligibility,and 16 chose not to participate.Data were collected from April to December 2017 using a convenience sampling method.Each patient was screened for their eligibility to participate in this study based on the following inclusion criterion:1) age ≥65 years; 2) hospitalized in medical wards;3) was able to follow instructions of the study.The exclusion criteria were as follows:1)all clearly diagnosed diseases at present that can lead to swallowing disorders,including neurological diseases(Parkinson’s disease,stroke,dementia),neuromuscular diseases (myasthenia gravis),and oropharyngeal diseases (head and neck cancer); 2)with gastric tubes or tracheal intubation; 3) had a diagnosis of swallowing dysfunction; 4) disorder of consciousness.
2.2.Measurements
2.2.1.Socio-demographic characteristics
Data were collected on socio-demographic characteristics,including age,sex,education,living,body mass index (BMI),total number of medications,and diseases which were diagnosed(in the patient chart),and activities of daily living(ADLs) were described.
2.2.2.Dysphagia
The 30-ml water swallow test [20]was used to assess swallowing function.The sensitivity,specificity,positive predictive value,and negative predictive value of the water swallowing test for diagnosing dysphagia compared with the Video Fluoroscopy Swallow Study (VFSS) were 97.5%,20.0%,90.7%,and 50.0% [21].Participants were instructed to sit in a relaxed upright posture and drink 30 ml of room-temperature water from a cup as able without interruption.According to the time spent to drink the water and presence or absence of coughing,the results included the following five levels:
Level I,drinking water successfully without interruption or coughing.
Level II,drinking water with two times of interruption and with coughing.
Level III,drinking water without interruption but with coughing.
Level Ⅳ,drinking water over two times of interruption and with coughing.
Level Ⅴ,coughing frequently and cannot drink the water successfully.
At the same time,swallowing abilities are classified as normal(Level I within 5 s),possible abnormality(Level I over 5 s or Level II),abnormality (Level III to Ⅴ).Possible abnormality and abnormality are both considered as having dysphagia.
2.2.3.Frailty
The Fried frailty phenotype was used as the definition of frailty[22]:1) Unintentional weight loss:unintentional weight loss of greater than 5.0%body weight in prior year.2)Slow walking speed:we asked patients to walk 15 feet (1 foot=0.3048 m) at their normal pace and record the time they used.The results were adjusted for sex and height.Assistive devices,such as walkers and canes,were allowed.3) Weak grip strength:it was measured by dynamometer using their dominant hand with a standing upright posture.The mean value of three repetitions was defined as the final result,adjusted for sex and BMI.4) Self-report exhaustion:identified by two questions from the Center for Epidemiologic Studies Depression scale(CES-D)“I felt that everything I did was an effort”and“I could not get going”were at least occasionally or more frequent.5)Low physical activity:different type of physical activity in the past week was calculated according to the International Physical Activity Questionnaire-Short (IPAQ-s) [23]based on patients’ report.Weekly energy expenditure for activities ≤600 Metabolic Equivalent Tasks (METs)-min was positive.Presence of three or more of five variables is classified as frail,presence of one or two as pre-frail,and presence of none as non-frail.
2.2.4.ADLs
ADLs were assessed by the Barthel Index [24],containing 10 items:feeding,dressing,personal grooming(wash face,comb hair,shave,clean teeth),bathing,bowel and bladder control,personal toilet use,moving from wheelchair to bed,and walking on the ground,up stairs,or down stairs.The values assigned to each item are based on time and amount of actual physical assistance required if a patient is unable to perform the activity.Scores range from 0 to 100,with a higher score representing better performance of the ADL.A score of 0 is given when the patient cannot meet the criteria of all the above activities.
2.3.Data collection
After completing the ethical approval,the procedure of data collection was as follows:First,all participants were fully informed regarding the research protocol and provided written informedconsent.Then,we collected relevant information from patient medical charts within the first three days after admission and assessed swallowing function,frailty,and ADLs.All assessment was performed in the ward by a researcher who received specialized training.
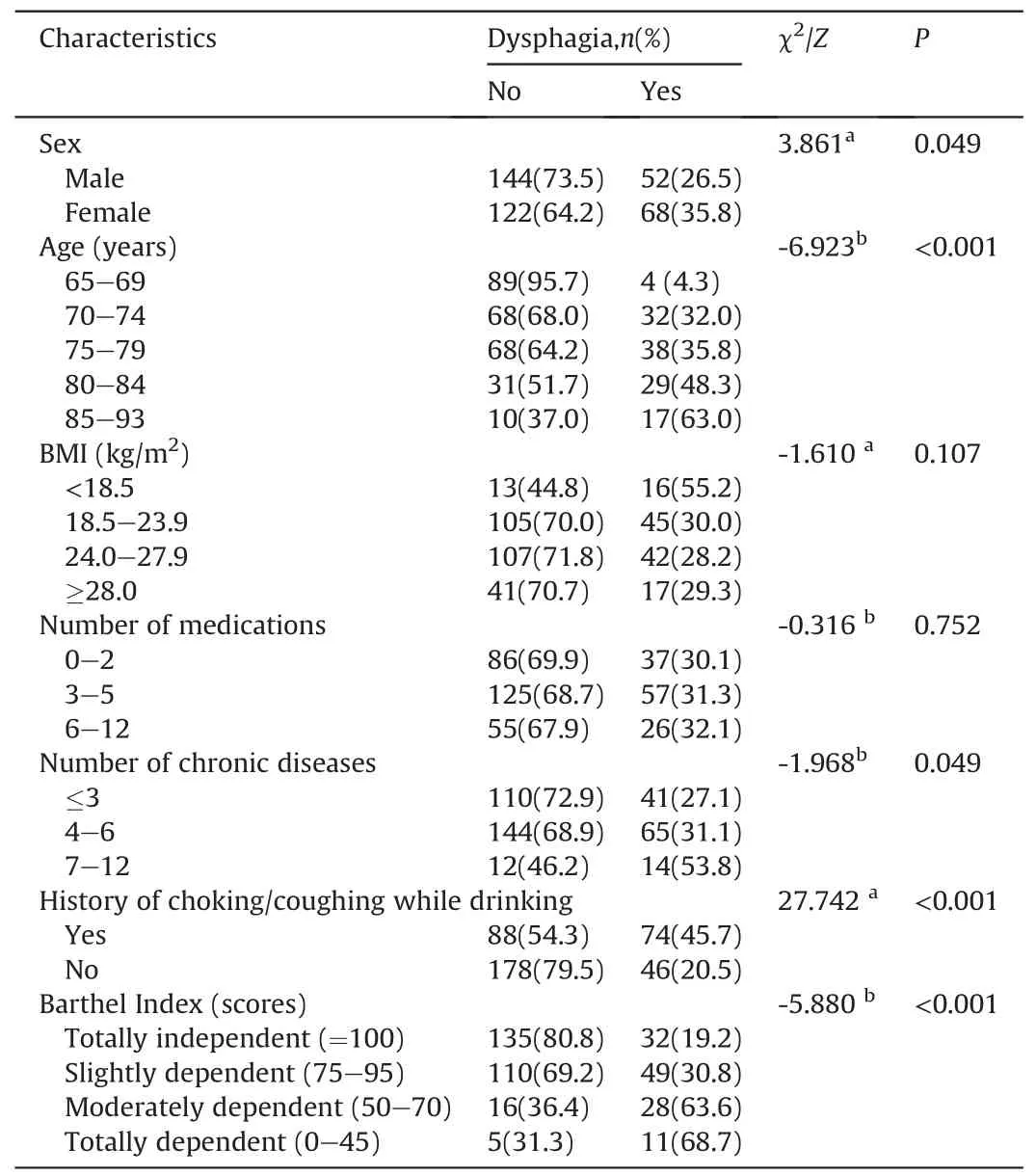
Table 1 Comparison of clinical characteristics among the participants with/without dysphagia (n=386)
2.4.Ethical consideration
The study was reviewed and approved by the Ethical Committee of Peking Union Medical College Hospital (Number:ZS-1361).
2.5.Statistical analysis
Descriptive statistics were used to summarize the study sample.Continuous variables were described as means and standard deviations and categorical variables as frequency (percentage).The chi-squared test or Mann Whitney U test were performed to make comparisons between two groups.Multiple stepwise logistic regression analyses were run to identify the association between frailty and dysphagia.All analyses were performed using SPSS statistical software version 22.0.
3.Results
3.1.Sample characteristics
Of the 386 participants,the proportion of males was almost equal to females.Mean age was 74.76±6.19 years(ranging from 65 to 93 years),and 87(22.5%) were 80 years or older.Many patients(47.2%,182/386) finished junior or senior high school.More than 90%lived with their spouse or children.A total of 150(38.9%)had anormal BMI.A total of 149(38.6%)were overweight(24.0-27.9 kg/m2),and 58(15.0%)were obese(≥28.0 kg/m2).Over 60%(n=263)were taking multiple medications,and the average number of diseases which had been diagnosed was 4.02 ± 1.75.The most common morbidities were hypertension,coronary heart disease,diabetes,hyperlipidemia,arrhythmia,pneumonia,cancer,chronic kidney dysfunction,chronic pulmonary obstruction,and other chronic diseases.Twenty (5.2%) patients were taking oral antipsychotic medications including anxiolytics,antidepressant drug and anti-hypnotics.Those who had a positive history of choking/coughing while drinking were 162 (42.0%).About 43.3% (167/386)were classified as totally independent with functional status as evaluated by the BI.
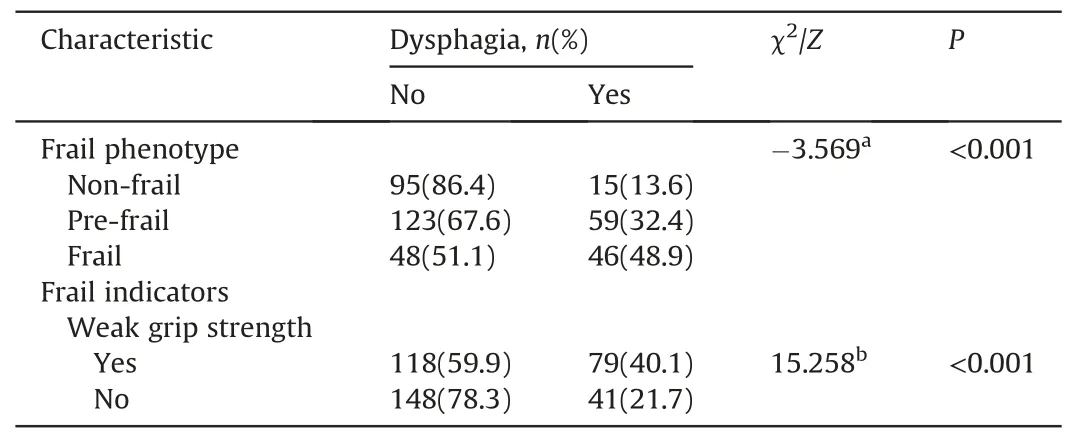
Table 2 Comparison of different frail phenotype among the participants with/without dysphagia.
3.2.Prevalence of age-related dysphagia and frailty
The prevalence of dysphagia based on the water swallowing test was 31.1%(120/386)and 52.9%(46/87)for participants over the age of 80.A total of 109 (28.2%) of the participants had possible abnormalities of swallowing function,and 11 (2.8%) failed the water screen test and were classified as having an abnormality.Based on the Fried frailty phenotype model,94 (24.4%) of the participants were frail,182 (47.2%) were pre-frail,and 110 (28.5%) were nonfrail.
3.3.The relationship between dysphagia and frailty
Frail and pre-frail patients were more susceptible to dysphagia than those who were non-frail.The three most prevalent indicators for patients with dysphagia was weak grip strength 65.8%(79/120),slow walking speed 59.2% (71/120) and self-report exhaustion 37.5% (45/120).In addition,there were also statistically significant differences between grip strength and dysphagia (Table 2).
In the univariate analysis,the prevalence of dysphagia was significantly different across the seven variables:age,sex,number of chronic diseases which had been clearly diagnosed,history of choking/coughing while drinking,the Barthel Index and frailty(Tables 1 and 2).
3.4.Risk factors of dysphagia
The results of Spearman’s correlation coefficient showed that there was a significant correlation between frailty and the Barthel Index (r=0.592,P < 0.001),and frailty increases with age.Therefore,the Barthel Index and age were not used as independent variates in the subsequent multivariable stepwise regression analyses,and the results indicated pre-frail odds ratio and frail phenotype,history of choking/coughing while drinking were associated with dysphagia with statistical significances (Table 3).
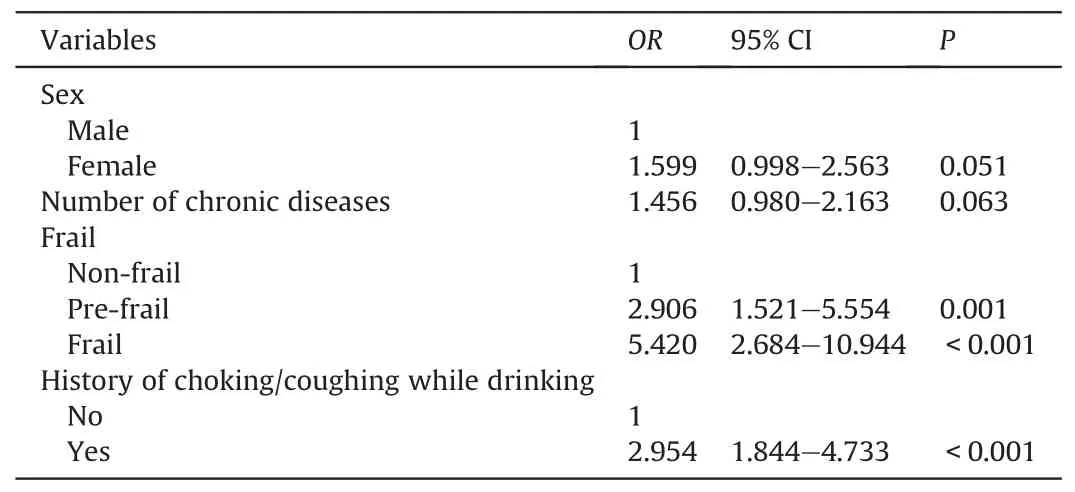
Table 3 Logistic regression models of dysphagia.
4.Discussion
4.1.Prevalence of dysphagia and frailty
The overall prevalence of dysphagia was found to be 31.0% and increased with age in hospitalized patients,similar to findings from other studies.The reported prevalence of participants in long-term care centers with swallowing disorders ranged from 7.0 to 40.0%[25].It ranged from 5.0 to 72.0%in community-dwelling elderly[4]and even higher in acute care units [11].Moreover,multiple previous studies focused on swallowing disorders associated with special diseases,such as stroke and dementia,or explored community-dwelling residents and the elderly in nursing homes and long-term care facilities.However,few studies focused on hospitalized patients.The current research excluded individuals who suffered from some diseases which made them more vulnerable to swallowing disorders,such as neurodegenerative disease,oropharyngeal organic disease,and patients with gastric tube or tracheal intubation.The fact that such a high proportion of dysphagia occurred in the elderly suggests that the swallowing function in the elderly cannot be ignored among hospitalized patients.
The prevalence of frailty was 24.4%,which was lower than other studies [26].This might be explained by differences of participant characteristics and methods used.In their study,patients aged 70 years and older were recruited,and the frailty was determined by the Cardiovascular Health Study(CHS)or the Study of Osteoporotic Fracture(SOF)frailty index.A prospective cohort study[27]showed that the elderly in medical facilities are more likely to be frail compared to community-dwelling residents.Frailty is increasingly regarded as a crucial indicator.Frail elderly participants were older and more susceptible to a host of disorders,such as old age,falls,malnutrition,comorbidities,and taking multiple medications.
4.2.The relationship between frailty and dysphagia
We did identify frailty as a predictor for dysphagia.Patients who were frail had the highest prevalence of dysphagia and were more likely to have dysphagia compared to patients who were non-frail.Frail elderly adults invariably have multi-organ problems,associated with adverse outcomes.For this reason,frail older people may be more vulnerable to swallowing disorders.Very recently,Bahat et al.[28]enrolled 1138 community-dwelling older adults to evaluate the association between dysphagia and frailty.They reported that dysphagia screened by the EAT-10 questionnaire was associated with frailty after adjusting for confounding factors.The dysphagia screening tool they used has been proven to be clinically relevant.Gonzalez et al.[17]observed that pre-frail participants had the highest proportion of failing the water swallowing test,and it was significantly different from other groups.However,that study recruited only 47 community-dwelling elderly women aged 85-94 and may not be a representative sample.
At present,there are few studies focusing on swallowing function of frail elderly.Dysphagia is prevalent among all phenotypes in older adults,and it can lead to severe complications.Hence,the relationship between frailty and dysphagia warrants further investigation.However,the definition of frailty is still discrepant.We found a positive relationship between dysphagia and handgrip strength.Madhavan [4]included 14 cross-sectional studies,and one prospective study indicated that only advancing age,clinical disease,and physical frailty were risk factors in communitydwelling elderly individuals.The study in which the frailty was measured by handgrip strength reported that physical frailty was one of risk factors associated with swallowing disorders.One work used walk speed and handgrip strength as a measure of frailty[18],and a positive correlation between handgrip strength and dysphagia in the univariate analysis was observed.This indicates that patients with lower handgrip strength were more susceptible to dysphagia.However,this relationship was not found by multivariate analysis.In Hathaway’s study [19],a large proportion of participants were diagnosed with stroke or Parkinson’s disease and had a positive history of cervical spine surgery,putting them at high risk of dysphagia,which may impact the results.Moreover,for patients intubated for more than 12 h after cardiac surgery,dysphagia was more prevalent among those with lower handgrip strength.As one of five frailty phenotype diagnostic criterions,handgrip strength was affected by some geriatric factors and could be regarded as a measurement of frailty [[29,30]].Recently,a systematic review suggested that measured handgrip strength might be used to identify sarcopenia and frailty,but the heterogeneity hindered the comparison between studies [31].Handgrip strength is related to muscle mass and function.
Therefore,we speculate that handgrip strength might be considered as the indicator of dysphagia but deserves more investigation.
4.3.Risk factors associated with dysphagia
Logistic regression analysis revealed history of choking/coughing while drinking was a risk factor for dysphagia.Notably,the positive history of choking/coughing while drinking was 2.64 times more frequent for patients with dysphagia than those without.For these patients,further clinical assessment is needed to identify whether they have swallowing disorders.Nevertheless,many factors could result in elderly cough,such as the speed of drinking,the volume of water or being distracted when drinking water.In addition,the frequency of cough should also be considered and combined with other symptoms and signs.
4.4.Limitations
It should be noted that there are some limitations in our research.Firstly,this is a cross-sectional study carried out in one tertiary hospital in China.Participants were admitted to hospital with various chronic diseases and had higher ADL scores than other studies.Hence,selection bias may exist in our study.Second,we only used the water swallowing test to screen dysphagia,so,patients with silent aspiration may not have been identified,and it only involved pharyngeal swallow function without mastication.Multiple reliable methods should be combined to increase the accuracy and reliability of the results.Finally,swallowing function might be affected by mastication,the severity of disease,and various diseases.
5.Conclusions
The present research revealed that there was a high prevalence of age-related dysphagia and frailty among hospitalized elderly individuals.Frail and pre-frail patients were at high risk of dysphagia,which suggests that dysphagia of frail elderly individuals should be given more attention.Frailty may be regarded as a predictor of dysphagia.Further investigations are needed to confirm this relationship.In addition,hospitalized older patients should also be given more attention compared with elderly from the community or nursing homes.
At present,age-related swallowing disorders remain underdiagnosed and ignored.Older patients without typical signs and symptoms may have potential dysphagia and be at risk of complications.Therefore,routine screening for dysphagia in hospitalized older individuals is important.Meanwhile,it is necessary to gain more insight to their dysphagia in clinical practice.
CRediT authorship contribution statement
Tiantian Wang:Conceptualization,Methodology,Software,Investigation,Data curation,Writing -review & editing.Yanwei Zhao:Methodology,Investigation,Data curation,Funding acquisition.Aimin Guo:Conceptualization,Methodology,Data curation,Supervision,Writing -review &editing.
Declaration of competing interest
All authors declared that there were not any actual or potential conflict of interest including any financial,personal or other relationships with other people or organizations.
Acknowledgments
The data was collected from Peking Union Medical College Hospital.We wish to thank all those who generously agreed to be interviewed for our work.We also sincerely thank Dr.Carrie Tudor for her revision of this paper.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2020.09.005.
杂志排行
International Journal of Nursing Sciences的其它文章
- Demands of experiential training for ICU nurses in Hunan of China
- The risk factors of postpartum urinary retention after vaginal delivery:A systematic review
- Community health nursing courses in baccalaureate nursing programs in China:A descriptive study based on website information
- An exploration of the breastfeeding behaviors of women after cesarean section:A qualitative study
- Understanding autism spectrum disorder and coping mechanism by parents:An explorative study
- Theory-guided interventions for Chinese patients to adapt to heart failure:A quasi-experimental study
