Rheumatoid arthritis and JAK2/STAT3 signaling pathway: How does the TCM works?
2020-11-16JinfengCaoHuihuiXuXiaoweiFuZhengYuMeijieLiuXiangchenLuChengXiaoYanLiJinghuaPanHongyanZhaoDahongJu
Jinfeng Cao, Huihui Xu, Xiaowei Fu, Zheng Yu, Meijie Liu, Xiangchen Lu, Cheng Xiao, Yan Li, Jinghua Pan,Hongyan Zhao*, Dahong Ju*
1 Beijing Key Laboratory of Research of Chinese Medicine on Prevention and Treatment for Major Diseases, Experimental Research Center, China Academy of Chinese Medical Science, Beijing 100700,China
2 The Second Affiliated Hospital, Shaanxi University of Chinese Medicine, Xianyang 712000, Shaanxi Province, China
3 Institute of Basic Theory of Chinese Medicine, China Academy of Chinese Medical Sciences, Beijing 100700, China
4 Institute of Clinical Medicine, China-Japan Friendship Hospital, Beijing 100029, China
Jinfeng Cao and Huihui Xu are the first authors who contributed equally to this article.
Abstract
Key words: rheumatoid arthritis; traditional Chinese medicine; JAK2/STAT3 signal; chronic synovitis;pannus formation; cartilage damage; bone destruction
Introduction
Rheumatoid arthritis (RA) is a symmetrical, chronic systemic autoimmune disease characterized by chronic synovitis, pannus formation, cartilage damage and bone destruction. It eventually leads to joint deformation and functional loss, bringing heavy economic burden to patients and society. Its pathogenesis is not clear. With the deepening research, the roles of MAPK pathway,Janus kinase (JAK)/signal transducer and activator of transcription (STAT), RANK/RANKL/OPG, PI3K/AKT,Wnt and other signal pathways in RA have attracted increasing attention. In this article, the JAK2/STAT3 signaling pathway is taken as the breakthrough point to review the mechanism of traditional Chinese medicine(TCM) in the treatment of RA.
JAK2/STAT3 Functional Structure
JAK is a non-receptor protein tyrosine kinase, which exists in the cytoplasm in a way of coupling cytokine receptors.There are four members in the family: JAK1, JAK2, Tyk2 and JAK3, among them JAK2 is widely found in tissue cellsin vivo[1]. JAK2 has 7 functional structural regions with high homology, JH1 and JH2 are located at the C-terminal,JH2 catalyzes tyrosine phosphorylation in cooperation with JH1, and JH3-JH7 are located at the N-terminal,which plays an important role in regulating the binding of JAK2 to receptors[2]. In general, different cytokines can activate the same JAK2 kinase to play a biological role,such as IL-6 and M-CSF (Figure 1).
STAT is a special protein family that combines with nuclear DNA, including 7 members: STAT1-4, STAT5a, STAT5b,STAT6, which are widely distributed in tissue cellsin vivo. STAT3 exists in the form of inactive homodimer in resting state. STAT3 phosphorylated in cytoplasm enters the nucleus during activation, and specifically binds to DNA site in nucleus for gene regulation[3]. STAT3 has 7 functional domains: Amino Terminal Domain (NH2),Coiled-Coil Domain (Coiled-Coil), DNA Binding Domain(DBD), Linker Domain (Lk), Tyrosine Activation Motif(Y), Transcriptional Activation Domain (TAD) and SH2 Domain[4-5](Figure 1). The functional structural region and the amino acid sequence of the “anchor site” of STAT in the receptor jointly determine the selection of STAT3 by cytokines, such as IL-6 specifically activates STAT3[6].
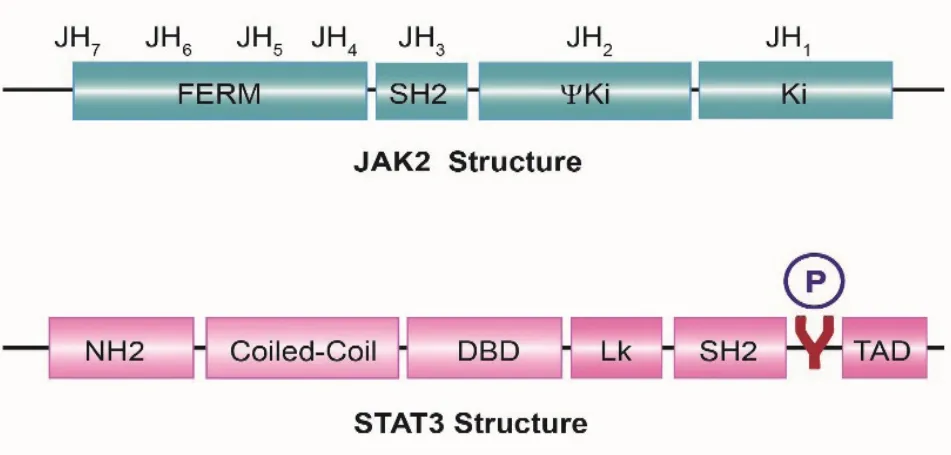
Figure 1 Structure of JAK2 and STAT3 [7]
Basic Process of JAK2/STAT3 Signal Transmission
JAK2/STAT3 signal pathway is a signal transduction pathway mediated by a variety of cytokines and widely participates in important pathophysiological processes such as cellular growth, differentiation, apoptosis,inflammation and immune regulation[8-9]. This signal pathway is mainly mediated by cytokines. Specific binding of cytokines to receptors on cell membranes causes a dimerization of intracellular receptors, making JAK2 coupled to receptors approach each other and activate through interactive tyrosine phosphorylation. Activated JAK2 phosphorylates tyrosine residues on the receptor.The phosphorylated tyrosine site and the surrounding amino acid sequence create a “docking site” for STAT3,which is recruited to the “docking site” through SH2 domain to bind to the receptor. STAT3 is phosphorylated by JAK2 and dissociated from the receptor in the form of antiparallel dimer to enter the nucleus. STAT3 specifically binds to the corresponding target sequence in the nucleus, regulates the expression of corresponding genes,and conducts extracellular signals into the cells, thus completing the whole process of signal conduction[3,10].JAK2/STAT3 signaling pathway can not only regulate embryo formation and immune response, but also affect cellular proliferation, differentiation, apoptosis and other biological processes[11].
The rapid start-up and inactivation of JAK2/STAT3 signal pathway depend on its negative feedback regulation mechanism. At present, studies have found that some protein families inhibit JAK2/STAT3 signaling pathways,such as, the suppressors of cytokine signaling (SOCS), the protein tyrosine phosphatase (PTP) and protein inhibitor of activated STAT (PIAS)[12-14]. SOCS protein can be synthesized and activated by a variety of cytokines, and at the same time it can regulate cytokines in turn. SOCS can be rapidly synthesized under the stimulation of external factors and bind with JAK2 to inhibit the activation of JAK2, or competitively bind to the “anchor site” of STAT3 on receptors, or hydrolyze JAK2 and STAT3 to negatively feedback and regulate JAK2/STAT3 pathway[13]. PTP protein family regulates JAK2/STAT3 signal conduction through negative feedback by reducing phosphorylation level on corresponding receptors. There are 4 members in the PIAS family, of which PIAS3 specifically binds to activated phosphorylated dimer STAT3, inhibits STAT3 entering the nucleus and binding to DNA specifically for transcription,thus inhibiting JAK2/STAT3 signaling[15]. Inhibitors, such as Tofacitinib, can inhibit JAK2 and further affect the phosphorylation of STAT3 for regulation[16-17]. In addition,JAK2/STAT3 signal pathway can be regulated by covalent modification negative feedback such as acetylation,glycosylation, ubiquitination of STAT3[18-20].

Figure 2 JAK2/STAT3 signal pathway
Mechanism of JAK2/STAT3 signaling pathway in RA
JAK2/STAT3 signaling pathway mainly interferes synovitis,pannus, cartilage damage and bone destruction in RA(Figure 2). Synovial membrane is a special connective tissue composed of macrophages and fibroblasts. The synovial fluid secreted by synovial membrane has the function of lubricating and nourishing joints. Macrophages in RA aggregates to form multinucleated giant cells,releasing pro-inflammatory factors such as TNF-α, IL-1β,IL-8, IL-15 and IL-17A, to cause osteoarticular synovitis[21]. IL-6, Leukemia Inhibitory Factor, Oncostatin M and IL-11, which share gp130 receptor, are also the main activation factors of JAK2/STAT3 signals[22]. IL-17 is a proin flammatory factor secreted by T helper 17 (TH-17) cells.TH-17 cells and IL-17 level are significantly increased in synovial fluid of RA patients and are closely related to the disease development of RA patients and animal models[23].After treatment with JAK2/STAT3 specific inhibitor AG490, collagen-induced arthritis (CIA) mice were relieved and IL-17A mRNA levels were significantly decreased, suggesting that JAK2/STAT3 participates in the development of synovitis by regulating IL-17A mRNA[24]. Retinoid-related orphan receptorγt (RORγt) is a key transcription factor that promotes Th17 cell differentiation to produce IL-17A, IL-17F and IL-22. Lack of RORγt will inhibit inflammation[25]. Synovial tissues of CIA mice showed that the mRNA expressions of JAK2, STAT3,IL-17A and RORγt were all increased, and the mRNA expression levels were all decreased after leflunomide and Chinese medicine treatment. It can be inferred that JAK2/STAT3 regulates the expression of IL-17A and RORγt mRNA, eventually regulates TH-17 cells that participate in inflammatory reactions[26]. Inducible nitric oxide synthase(iNOS) and cyclooxygenase-2 (COX-2) are common proinflammatory factors. In RA, iNOS and COX-2 increase the level of reactive oxygen species in synovium to promote leukocyte in filtration and aggravate inflammatory reaction[27]. JAK2/STAT3 pathway participates in oxidative stress reaction by up-regulating iNOS and COX-2 mRNA expressions in H2O2-treated cells[28]. Another TCM study shows that Prim-O-glucosylcimifugin (POG),the main component ofRadix Saposhnikoviae, can inhibit the expression levels of iNOS and COX-2 mRNA in macrophages induced by lipopolysaccharide (LPS)and inhibit JAK2/STAT3 pathway, while STAT3 overexpression reverses the inhibitory effect of POG[29].
Pannus is an inflammatory mass composed of newborn microvessels, macrophages and fibroblasts. Synovial fibroblasts (SFs) not only secrete inflammatory mediators that cause cartilage destruction, but also secrete cytokines that promote angiogenesis, such as epidermal growth factor (EGF), platelet-derived growth factor and matrix metalloproteinase (MMP) that degrade stroma and promote invasion. EGF binds to EGFR/ErbB2 receptor,activates JAK2/STAT3 signal transduction, regulates the expression of Myc mRNA, collagenase-1 mRNA,IL-8 mRNA and COX-2 mRNA, promotes macrophage proliferation, increases inflammatory factors and thus aggravates RA pannus formation[30]. Although endogenous MMP-2 and MMP-9 in RA patients both contribute to the migration and invasion of SFs, only MMP-9 degrades the basal protein so that endothelial cells enter the stromal matrix and participate in inflammation-mediated angiogenesis[31]. IL-6 and TNF-α can induce the formation of human cartilage cell line MMP-9 and can be used as activators of JAK2/STAT3 pathway[32]. Similar results were observed in corneal infection by Aspergillus fumigatus.IL-6 activates JAK2/STAT3 to up-regulate MMP-9. This evidence suggests that IL-6 and other cytokines may also regulate MMP-9 through this pathway in the development of RA[33]. In addition, NO released by iNOS is closely related to angiogenesis. JAK2/STAT3 signaling participates in LPS-induced iNOS mRNA expression[34-35]. Although the formation of pannus is related to angiogenesis factors,inflammatory factors, adhesion molecules and matrix molecules, the specific mechanism is still unclear[36].
Cartilage injury and bone destruction are another characteristic pathological changes of RA, which is related to bone metabolism imbalance. Osteoclasts absorb more bone through RANKL than osteoblastdominated bone formation, causing changes in bone density[37]. RANKL is required by osteoclasts. IL-6 can regulate RANKL by activating JAK2/STAT3 to promote bone loss in RA patients, while SOCS3 can inhibit this pathway through negative feedback[15]. Similarly, JAK1/2 inhibitor Baricitinib inhibits the up-regulation of RANKL induced by 1,25-dihydroxyvitamin D3and prostaglandin E2 in osteoblasts, thus inhibiting osteoclast formation[38].Bax and caspase-3 protein can promote apoptosis, while Bcl-2 protein can resist apoptosis. It is obvious that osteoclasts up-regulate the expression of anti-apoptosis factor or osteoblasts up-regulate the expression of proapoptosis factor on bone destruction. IL-1β can activate JAK2/STAT3 pathway in chondrocytes and enhance chondrocyte apoptosis[39]. Compared with patients with osteoarthritis, Bax protein in SFs of RA patients decreased while Bcl-2 protein increased, indicating that apoptosis factor may play a role in bone destruction by intervening inflammatory reaction[40]. SFs can also invade bones and joints, and MMP-9 decomposes the cartilage matrix in the gap under the stimulation of IL-1 and TNF-α to promote the development of RA[41]. Under the activation of IFN-γand IL-6, MMP-9 may be one of the target genes that JAK2/STAT3 regulates bone destruction[42].Further experiments prove that the expressions of TRAP,integrin-b, cathepsin K and MMP-9 mRNA in osteoclasts treated with AG490 are all decreased, indicating that the JAK2/STAT3 signal pathway is also involved in bone destruction[24].
Previous literature has pointed out that focusing on inhibiting immune cell activation or inflammatory cytokines cannot solve the chronic inflammationdependent SFs activation observed in some patients[37].In conclusion, JAK2/STAT3 signaling pathway targeting synovitis, pannus, cartilage injury and bone destruction may be the preferred strategy for RA treatment.
How Does the TCM Works?
TCM and synovitis
Chronic synovitis is a RA-based lesion, which is closely related to the increase of IL-6, IL-15, M-CSF and other cytokines. These factors can combine with JAK2 and then activate STAT3, thus promoting synovial cell proliferation and aggravating inflammatory reaction.Studies have shown that inhibiting the activity of STAT3 can reduce inflammatory reaction[43]. Extracts ofGentiana macrophylla, Clematis chinensis, Sophora flavescens,Curcumae Rhizoma, Ilex chinensis, Clematis manshuricaandPlumbagincan inhibit synovial cell proliferation and improve RA symptoms by inhibiting the expression of p-JAK and p-STAT3 in synovial fibroblasts[44-51]. TCM compounds Wangbi Tablets and Fengshi Ning Capsules have also been proved to have the similar therapeutic effects[52-53]. Experimental studies such asCurculigo orchioides, Salvia miltiorrhiza, Scutellaria baicalensis,Astragalus membranaceus, Ellipticine, Artemisininderivatives,Guizhi Shaoyao Zhimu Decoction, Jinwujiangu Granules, have shown that TCM can inhibit JAK2/STAT3 signaling pathway by inhibiting the expression of STAT3,improve joint swelling of CIA mice and rats, and provide basis for clinical treatment of RA[54-63](Table 1).
TCM and pannus
The formation of pannus marks the development of RA.Vascular endothelial growth factor (VEGF) is one of the most effective mediator for angiogenesis and plays an important role in RA pathology. Studies have shown thatGentiana macrophylla, Clematis chinensis, Clematis mandshuricaand Fengshiling Capsules can inhibit JAK2/STAT3 signaling pathway and further reduce VEGF mRNA expression, thus improving pannus formation in RA[45-46,50,53]. Gao et al intervened the CIA rats with total saponins ofDioscorea nipponica. The analysis of synovial tissue showed that total saponins ofDioscorea nipponicacould inhibit angiogenesis of RA by inhibiting the expression of STAT3 protein[64]. Another study ofDioscorea nipponicaalso showed that it can inhibit pannus formation by intervening STAT3[65].
TCM and cartilage damage and bone destruction
Cartilage injury and bone destruction are the important causes of deformity and teratogenicity in RA patients,which run through the course of RA. The IL-1 and IL-6 families regulate bone formation and bone resorption through JAK2/STAT3. Studies have shown thatsage, Salvia plebeia R.Br., Wenjing Huoluo Recipe inhibit osteoclast bone resorption activity and osteoclast differentiation activity, to prevent and treat RA-induced bone loss by inhibiting phosphorylation of JAK2 and STAT3[26,66-67].Experimental studies such as Lee and Lin showed thatcatechuandartemisininderivatives can obviously inhibit STAT3 expression, further inhibit the formation of osteoclasts, and regulate the ratio of helper T cells to TH-17 cells, thus protecting bone tissue[61,68].

Table 1 How does the TCM works on JAK2/STAT3 signaling pathway?
Conclusion
To sum up, JAK2/STAT3 signaling pathway can enhance RA inflammatory response, promote angiogenesis, activate osteoclasts and induce synovial cell apoptosis under the stimulation of cytokines. TCM can actively intervene synovitis, pannus formation, cartilage damage and bone destruction in RA pathological process through JAK2/STAT3 signal pathway. However, TCM as an alternative drug for RA treatment needs further research.
杂志排行
Global Traditional Chinese Medicine的其它文章
- Correlation between scapulohumeral periarthritis and cervical spondylotic radiculopathy
- Effects of nine saponins of Aralia echinocaulis root on the viability of bone marrow-derived macrophages
- Bushen Huoxue methods combined with amiodarone in the treatment of coronary atherosclerotic heart disease with severe frequent premature ventricular contractions: a case report
- Research status, countermeasures and recommendations of emergency management system for TCM prevention and control of major epidemics#
- Mechanism of prevention and treatment of osteoporosis with traditional Chinese medicine