中山地区70例儿童化脓性脑膜炎病原学及临床特征分析
2020-11-06黄军刘祥玉童辉纯
黄军 刘祥玉 童辉纯

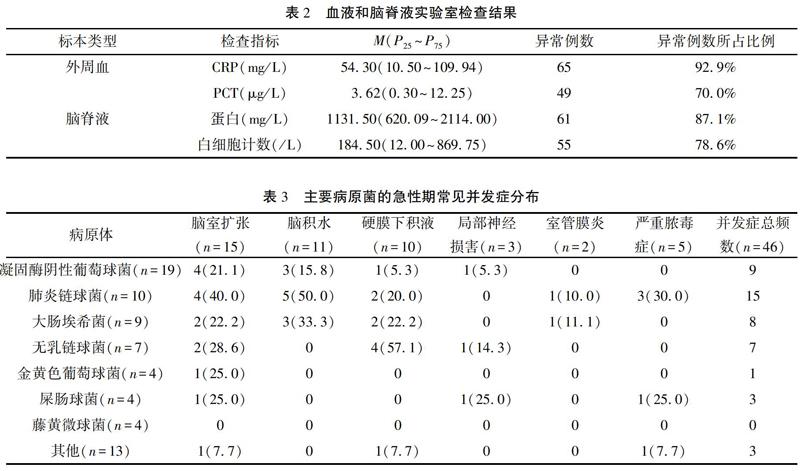
【摘要】 目的 探讨中山地区儿童脑脊液分离培养的不同病原体构成和临床特征,为临床对儿童化脓性脑膜炎(purulent meningitis,PM)的诊治提供依据。方法 选取2014年至2020年南方醫科大学附属中山市博爱医院住院的确诊为化脓性脑膜炎且脑脊液培养阳性的70例患儿为研究对象,病原体培养和鉴定按照《全国临床检验操作规程》进行,分析患儿一般资料、脑脊液和血液实验室检查结果及临床转归情况。结果 70例患儿检出70株病原菌,以革兰氏阳性球菌为主(52/70,74.3%),凝固酶阴性葡萄球菌最为多见(19/70,27.1%);革兰氏阴性杆菌18株(18/70,25.7%),主要为大肠埃希菌(9/70,12.9%)。75.7%的菌株分离均来自1岁以内的患儿。新生儿组和婴儿组分离的主要病原菌均是凝固酶阴性葡萄球菌和大肠埃希菌;儿童组分离的病原菌主要是凝固酶阴性葡萄球菌和肺炎链球菌。化脓性脑膜炎外周血CRP、PCT以及脑脊液蛋白、白细胞计数异常的比例分别为92.9%、70.0%、87.1%、78.6%。其中,肺炎链球菌脑脊液培养阳性患儿的外周血CRP水平中位数为149.59(50.69~194.26)mg/L,脑脊液蛋白水平中位数为2613.00(1420.00~3075.00)mg/L,两者均明显高于其他病原菌感染组外周血CRP水平[39.27(5.50~100.17)mg/L]和脑脊液蛋白水平[1113.00(606.50~1783.00)mg/L]。共有29例患儿出现并发症(29/70,41.4%),并发症总频数为46例次。脑室扩张(15例)最为常见,其次为脑积水(11例)和硬膜下积液(10例)。出现并发症的病例主要集中在凝固酶阴性葡萄球菌(7例)、无乳链球菌(7例)、肺炎链球菌(6例)脑脊液培养阳性患儿,最容易出现并发症的是无乳链球菌(7/7,100%)和肺炎链球菌(6/10,60%)感染。患儿积极治疗后达到治愈标准有31例,好转22例,未愈16例,死亡1例,总有效率为75.7%。结论 儿童化脓性脑膜炎主要发生在1岁以内的患儿,致病菌以凝固酶阴性葡萄球菌、肺炎链球菌和大肠埃希菌为主。各病原菌感染的实验室检查及并发症特点不同,肺炎链球菌感染的患儿外周血CRP和脑脊液蛋白较高,无乳链球菌和肺炎链球菌感染发生并发症的概率较大,应及早诊断,及时使用抗菌药物治疗,避免出现严重的并发症。
【关键词】 儿童;化脓性脑膜炎;病原学;预后
中图分类号:R683.2 文献标志码:A DOI:10.3969/j.issn.1003-1383.2020.09.009
【Abstract】 Objective To investigate the components and clinical characteristics of different pathogens and isolated and cultured from cerebrospinal fluid (CSF),so as to provide basis for clinical diagnosis and treatment of purulent meningitis (PM).Methods 70 cases of children hospitalized in Boai Hospital of Zhongshan Affiliated to Southern Medical University and diagnosed with PM,and whose CSF cultures were positive from 2014 to 2020 were selected as research objects.The pathogen culture and identification were carried out in accordance with the National Clinical Laboratory Operation Rules.And then,general information,CSF,blood laboratory results and clinical outcome were analyzed.Results 70 strains of pathogenic bacteria were detected in 70 children.Gram positive cocci (52/70,74.3%) were the main pathogens,and coagulase negative Staphylococcus was the most common (19/70,27.1%).There were 18 cases of gram-negative bacilli (18/70,25.7%),which was mainly Escherichia coli (9/70,12.9%).75.7% of the strains were isolated from children under 1 year old.The main pathogens isolated from neonatal group and infant group were coagulase negative Staphylococcus and Escherichia coli,while those from children group were mainly coagulase negative Staphylococcus and Streptococcus pneumonia.The abnormal rates of CRP,PCT,CSF protein and white blood cell count were 92.9%,70.0%,87.1% and 78.6%,respectively.The median levels of CRP in peripheral blood and cerebrospinal fluid were 149.59 (50.69-194.26) mg/L and 2613.00 (1420.00-3075.00) mg/L in CSF culture positive children with Streptococcus pneumoniae,both of which were significantly higher than those in other pathogenic bacteria infection groups [39.27 (5.50-100.17) mg/L]and cerebrospinal fluid protein levels [1113.00 (606.50-1783.00) mg/L].Complications occurred in 29 cases (29/70,41.4%),and the complication frequency was 46 times,with ventricular dilatation (15 cases) being the most common,followed by hydrocephalus (11 cases) and subdural effusion (10 cases).Complications mainly occurred in CNS (7 cases),Streptococcus agalactiae (7 cases),and Streptococcus pneumonia (6 cases),and complications were the most commonly seen in Streptococcus agalactiae (7/7,100%) and Streptococcus pneumonia (6/10,60%)infection.After active treatment,31 cases reached to cure standard,22 cases improved,16 cases did not recover,and 1 cases died,and total effective rate was 75.7%.Conclusion Purulent meningitis mainly occurs in children under 1 year old,and the pathogens are mainly CNS,Streptococcus pneumonia and Escherichia coli.Laboratory examination and complication characteristics of various pathogen infection are different.Blood CRP and CSF protein are high in children infected with Streptococcus pneumonia,and complications caused by Streptococcus agalactiae and Streptococcus pneumonia infection are more likely to occur.Therefore,early diagnosis and timely use of antibiotics for treatment should be made to avoid serious complications.
【Key words】 children;PM;etiology;prognosis
化脓性脑膜炎(purulent meningitis,PM)是由各种细菌感染引起的脑膜、蛛网膜下腔和脑血管急性炎症[1],是一种严重的感染性疾病。PM临床主要表现为发热、头痛、脑膜炎、脑性脑膜炎和大脑功能障碍,具有较高的病死率[2]。全世界每年约有120万例的新发病例,6个月以下的婴幼儿是该病的好发人群。可导致10%~20%幸存患儿出现永久性的神经系统后遗症,包括行为问题、学习困难,认知、运动、听力、视力障碍和脑积水等[3]。尽管抗菌药物和疫苗不断的发展,但其高发病率和高致死率仍威胁着儿童健康。因为不同地区、不同疾病类型或者不同年龄人群PM的发病率和病死率不同,预后也有差别[4~5]。因此了解本地区不同病原体和人群的发病特点对于疾病的治疗至关重要。儿童患者由于免疫系统发育尚未完善,血脑屏障抵御外来病原体的能力较弱,而且脑膜炎的典型症状不容易观察到,因此需要更多的研究资料为儿童PM的临床治疗提供线索。本研究通过回顾性分析中山地区2014年至2020年期間70例PM患儿中分离培养出的70株病原菌结果,探讨中山地区儿童PM不同病原体的分布、脑脊液(CSF)和血液实验室检查以及疾病预后特点,为本地区儿童PM的防治提供更多的依据和策略。
1 资料与方法
1.1 临床资料
选取2014年到2020年期间在我院住院诊断为PM且脑脊液培养病原学阳性的儿童患者70例。男39例,女31例,年龄介于1天到11岁之间。依据儿童生长发育的特点,分为0~28 d组(新生儿组)、~1岁组(婴儿组)和 >1岁组(儿童组)。其中新生儿组23例,婴儿组30例,儿童组17例。本研究有11例临床怀疑为污染菌株并剔除的病例,包括凝固酶阴性葡萄球菌7例,克氏微球菌、枯草芽孢杆菌、内氏放线菌、肺炎链球菌各1例。
1.2 病例纳入和排除标准
①年龄0~14岁;②临床表现符合儿童PM诊断标准[6],即有发热、呕吐、嗜睡及精神改变等表现;③CSF常规、生化检查符合PM改变;④CSF培养或者CSF细菌革兰染色检出病原菌。排除标准:①排除结核分枝杆菌和真菌引起的脑膜炎;②排除病原检测为阳性,但病情不符合《诸福棠实用儿科学》中PM诊断标准[6],不具有临床意义的怀疑污染的菌株。
1.3 血液和脑脊液标本微生物检查
所有入选的患儿在使用抗生素治疗前抽取0.5~1 mL脑脊液或者3~5 mL静脉血注入儿童血液培养瓶并立刻常温送检。采用美国BacT/alert3D血培养仪、VITEK32细菌鉴定仪对送检的微生物标本进行培养和鉴定。培养和鉴定流程严格按照实验室标准操作规程进行,每个标本至少培养5天才报告结果。
1.4 血液和脑脊液标本实验室检查
对送检的血清进行CRP和降钙素原(PCT)检测,脑脊液标本进行脑脊液蛋白和白细胞计数检查。血清CRP和脑脊液蛋白检测使用贝克曼AU5800全自动生化分析仪,血清PCT检测采用法国梅里埃VIDAS全自动荧光酶免疫分析仪,脑脊液白细胞数量使用牛鲍计数板进行人工计数。
1.5 疗效判定指标
用抗生素足疗程治疗且2次脑脊液检查正常,体温稳定且无阳性体征为临床治愈;经过治疗体温稳定且没有阳性体征,但是脑脊液白细胞>10×106/L为临床好转;否则为未愈。治疗总有效率=治愈率+好转率。
1.6 统计学方法
本研究中各项数据采用SPSS 20.0软件进行分析。计量资料不服从正态分布,采用中位数(四分位间距)M(P25~P75)表示,组间比较采用秩和检验,率的比较采用卡方检验,检验水准:α=0.05,双侧检验。
2 结果
2.1 不同年龄段患儿脑脊液阳性病原学分析
检出的病原菌共70株,以革兰氏阳性球菌为主,共52株(52/70,74.3%),其中凝固酶阴性葡萄球菌最为多见,19株(19/70,27.1%),其次为肺炎链球菌10株(10/70,14.3%)。革兰氏阴性杆菌18株(18/70,25.7%),最常见的为大肠埃希菌9株(9/70,12.9%),其次为脑膜炎败血黄杆菌(3/70,4.3%)。75.7%的菌株分离来自1岁以内的患儿。各年龄段中,新生儿组和婴儿组分离的主要病原菌均是凝固酶阴性葡萄球菌和大肠埃希菌,儿童组分离的病原菌主要是凝固酶阴性葡萄球菌和肺炎链球菌,肺炎链球菌和藤黄微球菌在儿童组中阳性率较其他组别高,组间差异有统计学意义(P<0.05或0.001)。大肠埃希菌和无乳链球菌主要分布在新生儿组和婴儿组。见表1。
2.2 血液和脑脊液实验室检查结果分析
PM患儿外周血CRP、PCT以及脑脊液蛋白、白细胞计数均高于正常值范围,各项目异常的例数占总数的比例分别为92.9%、70.0%、87.1%、78.6%。其中,肺炎链球菌脑脊液培养阳性患儿的外周血CRP水平中位数为149.59(50.69~194.26)mg/L,脑脊液蛋白水平中位数为2613.00(1420.00~3075.00)mg/L,两者均明显高于其他病原菌感染组外周血CRP水平[39.27(5.50~100.17)mg/L]和脑脊液蛋白水平[1113.00(606.50~1783.00)mg/L]。所有病原体的培养时长中位数为0.65(0.39~0.97)d。其中,凝固酶阴性葡萄球菌培养时长中位数为0.89(0.77~1.06)d、肺炎链球菌为0.26(0.17~0.63)d、大肠埃希菌为0.49(0.26~0.56)d、无乳链球菌为0.35(0.32~0.60)d、藤黄微球菌为2.05(0.76~3.00)d,肺炎链球菌和无乳链球菌的培养时长较短,而藤黄微球菌培养时长较长。血液和脑脊液实验室检查结果见表2。
[4]TROTMAN H,OLUGBUYI O,BARTON M,et al.Pneumococcal meningitis in Jamaican children[J].West Indian Med J,2009,58(6):585-588.
[5]OORDT-SPEETS A M,BOLIJN R,VAN HOORN R C,et al.Global etiology of bacterial meningitis:a systematic review and meta-analysis[J].PLoS One,2018,13(6):e0198772.
[6]胡亚美,江载芳.诸福棠实用儿科学[M].7版.北京:人民卫生出版社,2002:912-926.
[7]徐青青,李梅.317例儿童化脓性脑膜炎临床分析[J].中国当代儿科杂志,2015,17(7):710-714.
[8]黄涛,刘星苗,陈朝晖,等.2014—2018年天津市儿童医院化脓性脑膜炎病原菌分布及耐药性分析[J].现代药物与临床,2019,34(6):1909-1914.
[9]姜荣荣,李杨方.新生儿化脓性脑膜炎83例早期诊疗及病原学分析[J].中国基层医药,2016, 23(1):88-90.
[10]林罗娜,林立,温顺航,等.儿童细菌性脑膜炎100例病原分布及耐药分析[J].临床儿科杂志,2016,34(2):105-110.
[11]史中华,徐明,王永志,等.脑脊液检测指标对神经外科术后颅内感染的诊断价值[J].中华神经外科杂志,2018,34(6):601-605.
[12]CHEN H L,WU F,FU R,et al.Expression of MMP-2 and TIMP-1 in cerebrospinal fluid and the correlation with dynamic changes of serum PCT in neonatal purulent meningitis[J].Exp Ther Med,2018,15(2):1285-1288.
[13]周漫,彭銳,李艳.血清PCT、hs-CRP在成人脑膜炎诊断中的应用价值[J].国际检验医学杂志,2018,39(17):2102-2104.
[14]王建,雷雨涵.血PCT同CRP在儿童化脓性脑膜炎与病毒性脑膜炎中的鉴别诊断价值分析[J].临床检验杂志(电子版),2019,8(2):25-26.
[15]ALBUQUERQUE R C,MORENO A C R,SANTOS S R,et al.Multiplex-PCR for diagnosis of bacterial meningitis[J].Braz J Microbiol,2019,50(2):435-443.
[16]耿海峰,杨斌,朱雪萍.新生儿化脓性脑膜炎53例临床分析及其无乳性链球菌脑膜炎特点[J].中华临床医师杂志(电子版),2016,10(5):751-754.
[17]李清峰,吴明赴,符明凤.新生儿化脓性脑膜炎43例住院期间临床结局分析[J].中华临床医师杂志(电子版),2018,12(11):626-629.
[18]任建兵,李慈梅,邓文喻,等.无乳链球菌相关新生儿化脓性脑膜炎15例临床分析[J].国际医药卫生导报,2018,24(12):1760-1762.
[19]张娜,杨娜,曲妮燕,等.小婴儿无乳链球菌细菌性脑膜炎临床分析[J].中华实用儿科临床杂志,2017,32(20):1571-1574.
[20]JANOWSKI A B,NEWLAND J G.From the microbiome to the central nervous system,an update on the epidemiology and pathogenesis of bacterial meningitis in childhood[J].F1000Research,2017,6:86.
(收稿日期:2020-05-31 修回日期:2020-07-30)
(编辑:潘明志)