Clinical profile of amblyopia and outcome of occlusion therapy in pediatric populations attending a referral hospital
2020-11-02RajuKaiti1PabitaDhungel2AsikPradhan3MonicaChaudhry
Raju Kaiti1, Pabita Dhungel2, Asik Pradhan3, Monica Chaudhry
Abstract
•KEYWORDS:amblyopia; occlusion therapy; visual impairment; refractive error; strabismus
INTRODUCTION
Amblyopia originates from the Greek language which means dimness or dullness of vision. Amblyopia is also called lazy eye in a laymen term. Depending upon the prevailing patho-physiological concept about its etiology, this condition has been defined in a variety of ways. Simply, amblyopia can be defined as a unilateral or bilateral reduction in visual acuity caused by abnormal binocular interaction or deprivation of pattern vision; though no cause can be found on physical examination of the eye, some cases are reversible by therapeutic measures[1]. Many research works have shown that the deficit in amblyopia extends beyond monocular visual acuity impairment. Higher-order function such as binocular vision, fixation instability, and visuomotor activities are also impaired due to abnormal interocular interactions[2-3]. Approximately, 3% of the population is affected by Amblyopia and it has been estimated to carry a projected lifetime risk of visual loss of at least 1.2%[4]. Whatever may be the etiology, the basic mechanisms in the amblyopic cases are either form deprivation in one or both eyes or abnormal binocular interaction between the eyes[4-6]. It is one of the most common causes of childhood[7-10]and adult visual impairment[11-13]. Lack of awareness among parents and poor attitude towards routine screening can prevent amblyopia and unilateral amblyopia can only be identified early during screening.
Amblyopia is the result of degradation of the quality of retinal image during a sensitive period of visual development, which has been supposed to be the first 7 years of life[14]. It is to be understood that sensitive period for amblyopia development and the sensitive period during which treatment is possible, might vary with cases. Vision deterioration secondary to amblyopia can be permanent if corrective interventions are not taken in time. Amblyopia imparts great negative effects on the social, economic, behavioral, educational, physical and psychological aspects of a community. The burden of disability due to amblyopia can be pronounced when one takes into account the duration of life with visual disability[15-16]. Therefore, timely diagnosis, proper treatment of the problem in either of the eyes and follow up measures is very important.
SUBJECTS AND METHODS
This study was a hospital-based longitudinal, conducted from April 2015 to April 2016. All children less than 15 years of age who were diagnosed with amblyopia were included in the study. The study period was divided as: 6mo of data collection, 3mo for spectacle wear after cycloplegic correction as refractive adaptation and 3mo of occlusion after full refractive correction. The assessment of children included history, presenting visual acuity (PVA), best corrected visual acuity (BCVA) after cycloplegic [Cyclopentolate (1%)] refractive correction (post mydriatic test was done after 3d) and the chief reason or concern for which the children were brought for ocular examination. It also included detail history on the age of presentation, any previous treatments and/or interventions and detail ocular examinations as required.
Visual acuity was assessed with LogMAR chart in children older than 4 years of age. Those who couldn’t co-operate on LogMAR chart were assessed with other charts like Kay picture or Sheridan Gardiner charts or preferential looking charts.
The following definitions were used to classify the refractive error[17]: 1) Hypermetropia: refractive error greater than or equal to +0.50 DS. This was further categorized as low hypermetropia (≥+0.50 D to <+3.0 D), moderate hypermetropia (≥+3.0 D to <+6.0 D) and high hypermetropia (≥+6.0 D); 2) Myopia: refractive error of greater than or equal to -0.50 DS. This was further classified as low myopia (≥-0.50 D to <-3.0 D), moderate myopia (≥-3.0 D to <-6.0 D) and high myopia (≥-6.0 D); 3) Astigmatism: any cylindrical error of greater than or equal to ±0.5 D. Astigmatism was further classified as simple myopic astigmatism, simple hyperopic astigmatism, compound astigmatism and mixed astigmatism. It was further divided as “with the rule” when myopic astigmatism at 180±30 or hypermetropic astigmatism at 90±30, and “against the rule” when myopic astigmatism at 90±30 or hypermetropic astigmatism at 180±30. Astigmatism at >30 to <60 or >120 to <150 was considered as oblique astigmatism.
Depth of amblyopia was classified according to the BCVA attained as follow[18]: 1) Shallow amblyopia: 20/15 to 20/60; 2) Moderate amblyopia:20/70 to 20/100+; 3) Deep amblyopia: 20/200 and worse.
Visual impairment was classified according to the presenting visual acuity with which the children present to the department. Visual impairment was further classified[19]as: 1) Normal vision: 20/10-20/25; 2) Mild visual impairment: 20/30-20/60; 3) Moderate visual impairment: 20/70-20/160; 4) Severe visual impairment: 20/200-20/400; 5) Profound visual impairment: 20/500-20/1000; 6) Near total visual impairment: < 20/1000; 7) Total visual impairment: no light perception.
Detail orthoptic evaluations were performed. Cover test was performed for those having phoria or tropia. Fixation Pattern was assessed by the Linkz star configuration of the standard Heine’s direct Ophthalmoscope. Binocularity was assessed using red-green glass and worth four dot test (WFD) after full correction of refractive error if any present. Cases with eccentric fixation and wandering or no fixation were excluded from the study. Anterior segment and Fundus were examined. Color vision was screened by Isihara color vision charts and if required by Farnsworth 15 D after full refractive correction. All the subjects were prescribed full correction of refractive error.
The subjects were asked to use the spectacles for 3mo as the period of refractive correction adaptation and called for follow up every 1mo to see whether they are using spectacle regularly or not. Visual acuity recorded after 3mo of spectacle wear was recorded as refractive adaptation visual acuity (RAVA). Occlusion was commenced only after 3mo of spectacle wear. Oclussion was initiated at minimum of 6h per day for deep amblyopia; 4h per day for moderate amblyopia and 2h per day for shallow amblyopia (part time direct patching in foveal fixation) in the sound eye and alternate patching for those having binocular amblyopia. Opticlude eye patches were used in this study. Active home vision therapy was advised with occlusion and improvement after occlusion was also noted. Active home vision therapy like drawing, tracings, writing, bead stringing, television viewing, video games, puzzlesetc. were advised along with occlusion therapy. Visual acuity was then recorded first after 1mo of occlusion, secondly after 2mo of occlusion and finally after 3mo of occlusion. The data were analyzed by SPSS 16.0.
The following criteria were used as diagnostic criteria for classification[16]. Amblyopia can be defined in following ways: 1) If the difference in the BCVA between the two eyes is two or more Snellen’s lines provided no organic lesion that could result in visual reduction; 2) A BCVA of less than 6/12 in each eye on the Snellen’s chart provided no organic lesion that could result in a decrease in vision[20]. Amblyopia was categorized according to following criteria[21-22].
StrabismicAmblyopiaAmblyopia that results due to the presence of a manifest deviation (heterotropia) at near or distance fixation without any anisometropia.
AnisometropicAmblyopiaAmblyopia due to the presence of anisometropia of 1.0 D or more in spherical equivalent, or a 1.5 D or greater difference in astigmatism between the eyes but without any measurable heterotropia at near or distance.
CombinedAmblyopiaAmblyopia due to a heterotropia at near or distance along with anisometropia of 1.0 D or more in spherical equivalent or a 1.5 D or greater difference in astigmatism in any meridian between the eyes.
SensoryDeprivationAmblyopiaAmblyopia that results due to deprivation of stimulus to retina (cataract, media opacities or ptosis) without any refractive errors or heterotropia that could lead to the amblyopia.
AmetropicAmblyopiaAmblyopia that results due to refractive errors of more than 1.0 D spherical equivalent in both eyes resulting in subnormal vision in one or both eyes and no associated heterotropia or any other ocular pathology.If patients have significant anisometropia (as per the criterion mentioned above) along with high refractive errors in both eyes, then they were classified as anisometropic amblyopia group. Patients having strabismus for near and distance with bilateral refractive errors more than 1 D spherical equivalent were classified as strabismic amblyopia.
MeridionalAmblyopiaPatients having regular astigmatism greater than or equal to 1.5 D of astigmatism in any of the meridian or those with irregular astigmatism in eyes, leading to decrement in vision in one or both eyes and no associated heterotropia or anisometropia were kept under meridional amblyopia. Patients having significant anisometropia (as discussed above) along with a difference of 1.5 D or more astigmatism between the two eyes were classified as Anisometropic amblyopes. Similarly, patients having heterotropia for near and distance with regular astigmatism of more than 1.5 D or irregular astigmatism were classified under strabismic amblyopia.
ConfidentialityResponses were anonymized and participants were made aware of this fact before participation in the study. The names and status of all the participants were made strictly confidential.
EthicalConsiderationWritten consent was taken from each child and parent prior enrolling in the study and ethical clearance was obtained from the Institutional Review Committee (IRC-KUSMS). The study protocol adhered to the provision of the Declaration of Helsinki for research involving human subjects.
StatisticalAnalysisData were entered and analyzed on SPSS 16. Results were analyzed using relevant statistical tools. Descriptive tabulations and Chi-square tests were used to generate descriptive information from qualitative data assuming normalcy.
RESULTS
Among the total number of 1,092 children visiting ophthalmology department, 60 (5.49%) subjects were amblyopic. Total amblyopic eyes diagnosed were 86. The average age of presentation of amblyopic children was 8.87±3.29 (range: 3-15) years. Females were more common in presentation accounting for 58.30% of total participants. 26.67% (n=16) children were of ages ranging from 3-7 years, 40% (n=24) were between age range 7-11 and 33.33% (n=20) were between age range 11-15. Common complaints reported were difficulty in viewing board (25%,n=15). and headaches (20%,n=12) and Squint (20%,n=12). 20% of the children were asymptomatic and detected on routine examination. 56.7% (n=34) of the cases were monocular and 43.3% (n=26) were binocular amblyopia.
Meridional amblyopia being the most common form of the amblyopia, astigmatism was the most common type of refractive error found among the clients. The average age of presentation of children with amblyopia was 7.16 years for isohyperopic amblyopia,the earliest of all presentation. Average presenting age of anisohyperopic amblyopia is significantly higher than that of other types of amblyopia.
Most of the cases were orthophoric (73.3% for near and 75% for distance). 13.3% of total clients had exotropia for near and distance. Esotropia was found among 10% of the total clients for both, near and distance. 70% of the clients had binocular single vision despite of amblyopia whereas remaining 30% showed suppression in amblyopic eyes for near and distance.
The result regarding previous treatment is not satisfactory as 61.7% of the total subjects didn’t receive any form of treatment for the problem. Most of these cases were new presentation in Out Patient Department. Few subjects, though had ocular examination, were not under any interventions for amblyopia.

Table 1 Age distribution with types of amblyopia
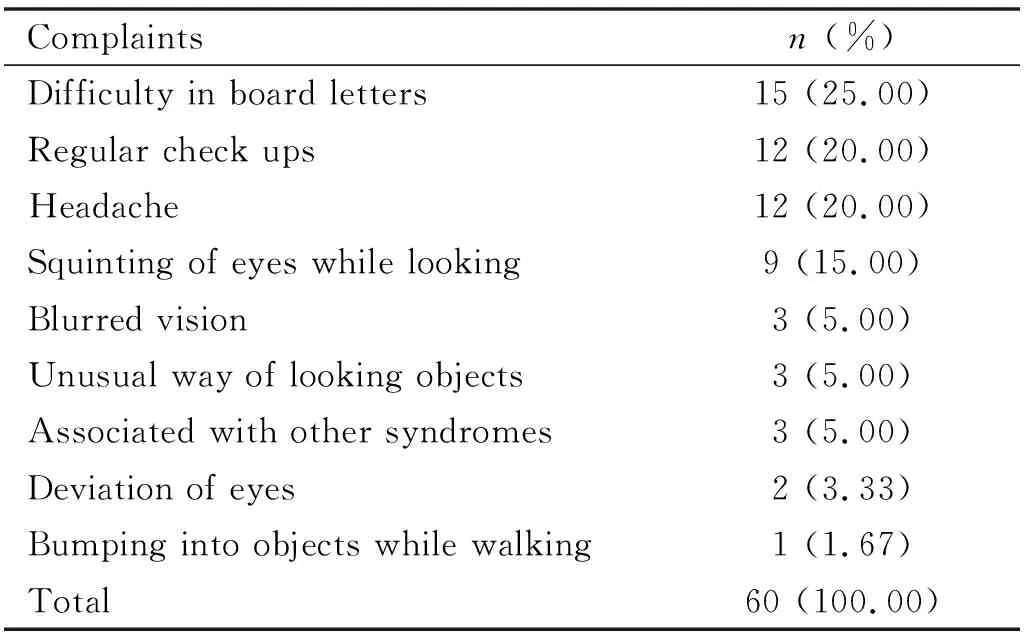
Table 2 Chief complaints

Table 3 Amblyopia distribution

Table 4 Type of amblyopia and age of presentation
26.7% of total cases were using only spectacle as interventions and only 11.7% of the total subjects were under combined spectacle, patching and active vision therapy. 58.30% of the total cases (n=35) had shallow amblyopia. Moderate amblyopia was found in 18.3% of cases (n=11) and 23.3% had deep amblyopia (n=14).

Table 5 Refractive error
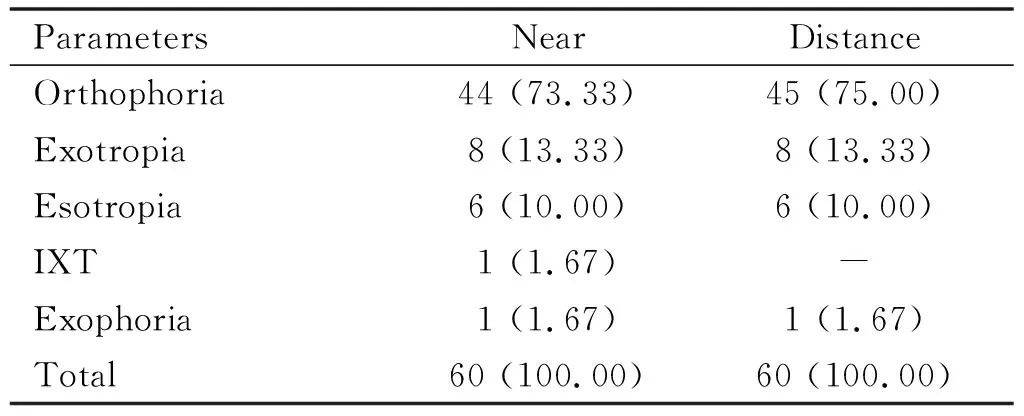
Table 6 Cover test n (%)

Table 7 Previous treatment
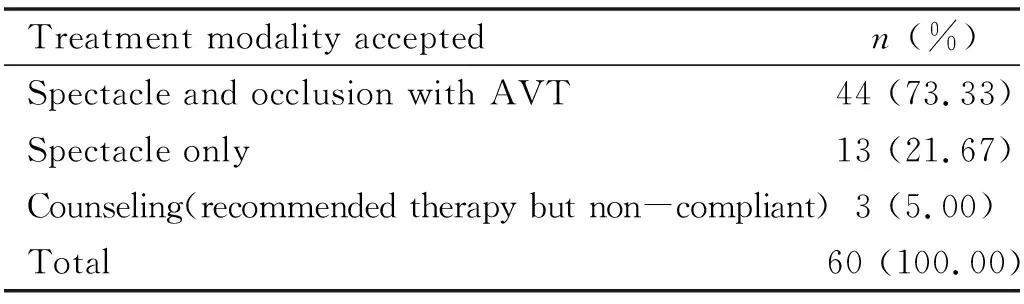
Table 8 Treatment modalities accepted
OutcomesofTreatmentThere is statistically significant improvement in visual acuity after the different treatment strategies after 3mo in amblyopic eyes, using Games Howell test of one way ANOVA for multiple comparison. Most of the subjects were provided with refractive correction and occlusion with active vision therapy (AVT) (n=44), whereas, 13 subjects used only spectacle (didn’t will to patch the eyes even after best possible counseling), 3 subjects didn’t use spectacle and occlusion (didn’t will to patch the eyes and use spectacle even after best possible counseling). Last group of subjects were only counseled. Older children were less obedient toward occlusion and also those with poor visual acuity in the amblyopic eyes were among the difficult subjects for occlusion.

Table 9 Improvement in visual acuity

Figure 1 Distribution of depth of amblyopia There were 35 shallow, 11 moderate and 14 seep amblyopic subjects.

Figure 2 Visual impairment before and after treatment.
Among the modalities for treatment of amblyopia, refractive correction combined withocclusion and AVT, showed statistically significant improvement in visual acuity. The mean among these compared using Games Howell test of one way ANOVA for multiple comparison.
Above table clearly shows the difference in final visual outcome after different treatment modalities. Final visual outcome after spectacle correction combined with occlusion and active vision therapy is significantly better compared to other children without occlusion. 30% of the cases (n=18) had moderate visual impairment, 15% (n=9) had severe visual impairment and 1.7% (n=1) had profound visual impairment when they presented to the Ophthalmology department. 30% of the cases were under normal visual acuity level.
There was significant improvement in the visual impairment severity after treatment of amblyopia. Only 5% (n=3) were left with moderate visual impairment, 36.7% (n=22) had mild visual impairment and 58.3% (n=35) improved to normal visual acuity level after treatment with spectacle and occlusion therapy. These findings show the positive effect of early detection and interventions of amblyopia. Despite late presentation of age (mean age of presentation being 8.87 years), visual acuity could be improved with appropriate refractive correction combined with occlusion and active vision therapy.
DISCUSSION
Out of 1,092 pediatric cases presented to the department of Ophthalmology, 60 cases were diagnosed to have amblyopia. This gives the prevalence of amblyopia as 5.49% which is slightly less than that 9.1% found by Woldeyesetal[20]at Menilik Hospital. With a prevalence varying between 0.2% and 12% depending on the subsets of the population studied, amblyopia is one of the most common causes of visual impairment in children[7]. The prevalence of amblyopia varies significantly and has been reported to be as high as 12% in a refractive error study done by Rakhi Dandona et al in Andhra Pradesh, India[23].
One of the important findings identified in this study is the relatively old age at presentation (8.87±3.29 years), irrespective of the subtype of amblyopia. In the similar study done at Menilik Hospital[20], Ethiopia, the average age of presentation was 6.9±3.2 years and in India the average age of the patients at presentation was 7.97±6.18 years[24]. In a study done in Pakistani children, the mean age of the 316 patients was 8.14 years[25]. This late presentation of amblyopia to hospital might be due to casual attitude of parents about vision and absence of school screening in Nepal which needs serious attention in the future. It is assumed that therapeutic measures for amblyopia are less effective after seven to eight years[6,8,26-27]. Isohyperopic amblyopes had early presentation at 7.16 years than the anisohyperopic amblyopes (10.83 years). This might be due to reduced vision in both eyes and forcing the children go for early examinations while in the case of anisohyperopic amblyopes; they have good vision in an eye and would have lesser difficulty in vision. The presentating symptoms of distance blur in class and headaches brought almost 50% of children to the hospital. Almost one fifth of the children were asymptomatic. The subjects with headache and those asymptomatic subjects contributed to over all late presentation to the hospital.
Most of these children either had monocular amblyopia or shallow form of amblyopia. Monocular amblyopes won’t have reduced vision like in binocular amblyopes and hence they won’t present particularly for ocular examination. Shallow amblyopes also won’t have problems in dailies especially with the children and hence won’t present for eye examination early. Many parents were found to be conscious about the way their children looks and these groups were among those who bring their children early for ocular examination. Squinting of eyes while looking objects (15%,n=9), unusual way of looking (5%,n=3) and deviation of eyes (3.3%,n=2) were the complaints related to strabismic and/or combined form of amblyopia. Parents are directly involved in early diagnosis and management of amblyopia. So, attitudes of parents play important role in early or late presentation of the children. Hence, parent’s awareness and knowledge on the importance of vision screening and ocular examination can be highlighted. 3 children presented with other associated symptoms; two with Down’s syndrome and one with xeroderma pigmentosa.
Etiologies of amblyopia have been shown to vary in different studies, depending on the characteristics of the study sample and how amblyopia is defined. In our study, refractive amblyopia was the major cause for amblyopia constituting 71% of the total (43.3% had meridional amblyopia, 25% had anisometropic amblyopia and 11.7% had isoametropic amblyopia). 6.7% of the cases had strabismic amblyopia, 3.3% had stimulus deprivation amblyopia and 10% had combined amblyopia. Most of other studies had shown strabismic amblyopia as a common type whereas in our study meridional amblyopia was the most common form. In the study done at Menilik Hospital in Ethiopia[20], 39.3% had strabismic, 27.3% combined, 6.0% anisometropia, ametropic and sensory deprivation amblyopia comprised 13.7% and 13.1% of the cases respectively. In a comparative study done in India[24], of a total of 733 eyes, 37.38% had strabismic amblyopia, 22.1% had anisometropic amblyopia, 18.44% had combined amblyopia, 12.88% had ametropic amblyopia, and 5.56% had meridional amblyopia, and the remaining 7.63% patients had sensory deprivation amblyopia. In a study done in Pakistan[25], the cause of amblyopia was strabismus in 120 (38%) patients, anisometropia in 136 (43%) and both strabismus and anisometropia (combined-mechanism) in 60 (19%) patients. It might be due to the higher prevalence of strabismic amblyopia; these studies had earlier age of presentation than our patients did.
In our study, 56.7% cases had monocular amblyopia and 43.3% had binocular amblyopia. This might be one of the reasons for the average age of presentation being on higher range in our study. Children won’t complain unless they have diminished vision in both eyes and this will delay the ocular examination. In the study done in Pakistan[25], 69% had amblyopia in both eyes and only 31% had monocular amblyopia.
Analyzing the severity of amblyopia, 58.3% (n=35) had shallow form of amblyopia and these higher prevalence of shallow amblyopia could be one of the reason for late presentation. 18.3% (n=11) had moderate amblyopia and 23.3% (n=14) had deep amblyopia. Astigmatism was the most common form of refractive error, 58.3% in both the eyes. It was followed by hypermetropia (22.50%) and myopia (7.5%). In the study done at Menilik Hospital[20], 113 (61.7%) patients had a hypermetropic refractive error and forty eight (26.2%) patients had no significant refractive errors. It was 51.65% of hypermetropia and 14.38% of emmetropia in the Indian study[24]. Hypermetropia was the most common refractive error in both these studies. This finding in our study correlates the higher prevalence of meridional amblyopia in contrast to strabismic type found in other studies.
Prevalence of strabismus is minimal in our study compared to the study done at Menilik Hospital[20], India[24]and Pakistan[25]. Most cases (73.3% in near and 75% in distance) had no ocular alignment problems in our study. Only fourteen cases (23.3%) had manifest deviation in our study. The study in Menilik Hospital[20]showed one hundred twenty eight (69.9%) amblyopic children with strabismus, and 62.2% strabismus in the Indian study[24]. In strabismus, the different stimuli received by the eyes prevent normal image fusion, compromising binocular vision and summation and the ability to discriminate disparity and depth of vision with altered stereoscopic visual acuity (stereopsis) and even postural stability[28]. 61.7% (n=37) of the children didn’t have undergone any forms of treatment previously. Most of the children didn’t have ocular examination before and some were prescribed some form of treatment but were not using. Many of them were prescribed spectacles and even occlusion therapy previously. 16 subjects were using spectacle as prescribed but were not under occlusion therapy. Only 7 subjects were under spectacle combined with occlusion and active vision therapy. Lack of proper counseling by practitioners, lack of adequate explanation to the parents with resultant poor involvement of the parents, long distance to eye center and improper follow-up, lack of knowledge of effective amblyopia treatment on the part of eye care personnel, lack of proper primary eye-care screening services and lack of qualified orthoptists and optometrists are the barriers for successful inclusion of the amblyopes in the treatment modality.
Visual impairment has significantly reduced after treatment modalities prescribed. Use of spectacles, occlusion therapy and active vision therapy with proper counseling and regular follow ups helped many children improved their visual acuity level. 18 subjects had moderate visual impairment, 9 had severe visual impairment and 1 had profound visual impairment when they presented to the Ophthalmology department. 32 subjects had normal to near normal visual acuity level. There was significant improvement in the visual impairment table after treatment of amblyopia. Only 3 subjects were left with moderate visual impairment, 22 subjects had mild visual impairment and 35 subjects improved to normal visual acuity level after treatment with spectacle and occlusion therapy. These findings show the positive effect of early detection and early interventions of amblyopia. Amblyopia is the easiest form of preventable blindness. Many children are forced to live with visual impairment secondary to amblyopia.
Spectacle prescription among small children in our society is not usual and it takes too much effort to make the parents understand about its importance and urgency in management. Occlusion therapy has been the backbone of amblyopia therapy. Late presentation for ocular examination combined with non-compliance for spectacle wear and occlusion therapy have been the main hurdle for amblyopia treatment. In our study compliance with spectacle wear combined with occlusion therapy and active vision therapy was 73.3% (n=44). Only 3/4thof the children actively participated in the occlusion therapy and visual acuity could be improved significantly. Similar study done in Pakistan[25]showed 80.4% (n=254) compliance rate. They found that 11 patients (10.4%,n=106) in age group between 8-14 years and 10 patients (6.7%,n=148) in age group between 3-8 years had no improvement with treatment in visual acuity of the amblyopic eye. In our study, we found that compliance to occlusion had inverse relation with increased age. 75% (15 out of 20 cases ranging between age 11-15 years) had no compliance for occlusion. Some of them started occlusion but didn’t continue long and discontinued occlusion within 1-2wk of initiation. Peer influence and criticism by friends at school was major reason for the refusal by children.
The difference between best corrected visual acuity and post occlusion visual acuity after three months was 0.243 which was significant (P=0.001). This result shows the importance of refractive correction combined with occlusion and active vision therapy. 20 subjects presented after 10 years of age and these subjects though willing to wear spectacle, were not willing to wear eye patch. In our treatment course, 13 subjects didn’t continue patching and used only spectacle. These children were of higher ages (11-15 years). Awkwardness among friends in the school and home was the major reason for not continuing occlusion as prescribed. 3 subjects neither used spectacle nor occlusion as prescribed. The management was reinforced but still failed acceptance by child or parents. One of the three had severe loss of vision in the amblyopic eye. He was not improved with refractive correction and hence occluding the sound eye totally made him handicap. Remaining two cases had high refractive error and had no improvement with best possible correction; also didn’t have compliance with occlusion.
The diagnosis of amblyopia is challenging since there is no specific test to detect it, and it depends on the child’s ability to cooperate, potentially compromising the diagnostic process[29]. Individuals with amblyopia often have restricted career options and reduced quality of life, including less social contact, cosmetic distress (if associated with strabismus), low self-esteem, visual disorientation, and fear of losing vision in the other eye[30]. Traditional amblyopia treatment options have documented improvement with spectacle correction when indicated, followed by occlusion or atropine penalisation of the non-amblyopic (fellow) eye. While the majority of children show improvement with these approaches, not all children respond to traditional therapies[31]. The management of pediatric amblyopia is often time consuming and requires a lot of understanding, patience and commitment by the child, the parents and the eye care practitioners. Ocular examination should be kept as a regular schedule in every school and also there should be a system of ocular examination of the children prior to admission in school. The American Academy of Pediatrics has recommended screening for amblyopia as a part of the regular child visit made by a pediatrician, including the use of instrument-based vision screening techniques for preverbal children[32]. Newer works have shown two major shifts in paradigm regarding amblyopia: the belief that successful treatment of amblyopia outside the critical period is possible and the concept that amblyopia is more of a binocular, rather than a monocular, disease[33]. New protocols with different and more engaging games such as action-oriented adventure games, first-person shooter games, virtual reality, and 3-dimensional gaming platforms are being analyzed for this purpose[34-37]. More detail and global study of amblyopic subjects can give justifications about the great variability of response to treatment of amblyopic subjects. This will also help to prepare a more customized treatment protocol for different types of amblyopia[38]. Though this study has selection bias, it can form the basis for future population based studies. One of the advantages with hospital based studies is that, varieties of patients from different parts with different referrals are included and hence a good clinical profile can be established.
This study concludes that prevalence of amblyopia and associated visual impairment is still a public health issue in developing countries like Nepal. Lack of awareness and lack of community or preschool vision screening for children lead to late presentation and significant visual impairment associated with the condition. The burden can easily be reduced with screening camps, timely referrals and proper interventions. Refractive amblyopia being the most common subtype highlights the importance of vision and refractive screening and early correction. Since it was a hospital based study, it had selection bias. Also, occlusion therapy was taken as a sole treatment modality; comparison could not be made as for the efficacy compared with other modalities. Follow ups after occlusion was not taken for longer duration. Efficiency of occlusion in different age groups was not assessed.
