Analysis of ocular surface dysfunction in patients with type 2 diabetes mellitus
2020-11-02
Abstract
•KEYWORDS: dry eye;ocular surface dysfunction;diabetes mellitus; related factors
INTRODUCTION
In recent decades,the prevalence of type 2 diabetes has increased notably[1]. At present diabetes mellitus is the leading cause of blindness in the adults worldwide.Ocular disorders are widespread in diabetic, such as corneal epithelial erosions, cataract,retinopathy, secondary glaucoma,and dry eye disease. Corneal diseases seem to be more common in diabetic patients affecting up to 70%[2]. The workshop (DEWS II) manifested that diabetes may be a risk factor of dry eye[3]and compared to the non-diabetic people the symptoms are worse in resent report in dry eye[4].
The recent definition of dry eye is an ocular surface disease caused by various elements. The main feature of dry eye is the instability of tear film, which is combined with multiple ocular symptoms. Tear film instability, increased osmotic pressure, ocular surface inflammatory damage and sensory nerve abnormalities play a significant role in the pathogenesis of dry eyes. In recent years, some academicians have verified the relationship between type 2 diabetes and tear film dysfunction[5]or meibomian gland dysfunction[6]. However, few studies have been made to evaluate tear meniscus height changes in diabetics, which are deemed very sensitive for dry eye assessment. In this study, we examine ear meniscus height changes in diabetics and compare it with Schirmer tests (SⅠt), tear film break-up time(TBUT), and corneal fluorescein staining which assess basic tear secretion and ocular surface function.
SUBJECTS AND METHODS
This study protocol obeyed the accordance of the Declaration of Helsinki and was authorized by the Institutional Review Board and the Ethics Committee. All the participants offered an informed consent.All participants had to provide their own blood glucose levels and hemoglobin; the normal glycemic limit for all subjects was 110 mg/dL. More than 6.4% of hemoglobin is thought to be associated with autonomic neuropathy[6-8]. The participants were aged from 42-70 (mean: 55.34±8.1) years for the diabetics and 45-76 (mean 56.89±8.5) years for the control group. One eye of each participants was selected. The exclusion criteria were as follows: patients who had diabetic neuropathy,autoimmune diseases, and those who had other comorbid ocular diseases, such as previous ocular surgery,DES,ocular allergies, and ocular injury.
The two groups should adopt a unified examination standard and time. In this study, it was stipulated that the examination should be conducted from 9:00 a.m. to 12:00 a.m. every day. In order to avoid the maladjustment of patients, the room temperature was strictly controlled at 20-25℃, the humidity was 30%-50%, and the indoor lighting was mainly soft. Every participant should complete an ocular surface disease index (OSDI) questionnaire in order to assess the symptoms of ocular surface. If the score was ≥3.5, subjects were considered symptomatic[9]. All participants proceeded a sequence of measurements of ocular surface in the following order: TBUT, tear meniscus height (TMH), corneal fluorescein staining (CFS), tear secretion (SⅠt). There should be a 30-minute interval between each test. All the participants were examined by the same physicians.
After placing the placid pattern of polaris last complete blink, TBUT was counted in seconds. The value lower than 10s was considered abnormal[10-11]. TMH measurements were executed by a commercial AS OCT (SS-1000; Tomey Corp, Nagoya, Japan). In every subject,across the central cornea, cross sectional photos of the lower TMH were taken vertically. The line space from the fluid surface of the meniscus junction to the lower eyeli-meniscus junction defined TMH. The TMH values were measured by the cross-sectional AS OCT photos. The value higher than 200 μm was considered abnormal[12]. The area of exposed ocular surface was classified by the Van Bijsterveld scheme with fluorescein staining (FL). The ocular surface was divided into nasal, temporal and middle regions, and according to the number of staining points observed, each region was scored 0-3 points[13]. Add up the scores for each area to get the final score.The analysis of the results was based in the value higher than 3.5, considered abnormal, and total score was maximum 9. Tear secretion test (SⅠt), driped in the conjunctival sac 1 of 4 g/L oxybuprocaine hydrochloride (towering in the pharmaceutical co., LTD.), 1min after put the tear secretion test into palpebral conjunctiva sac temporal lateral 1/3 place both at home and abroad, calculation the paper wet long after 5min, The normal values considered was >5 mm/min[14].

Table 1 Clinical characteristics in diabetic and non-diabetic patients
Statistical analysis wasexecuted using the SPSS version 19.0 (SPSS, Inc., Chicago, IL.USA). Mean values for the two groups were contrasted with the independent-samplest-test.The correlations between the glycemia, Hb1Ac, duration of diabetes,and tear film variables were researched by Pearson’s correlation coefficient in the diabetic group. The Mann-Whitney test was used to contrast the results when the value was not normally distributed. APvalue less than 0.05 was identified statistically significant.
RESULTS
In this study,we analyzed 60 eyes of 60 diabetics and 60 eyes of 60 no-diabetics. Demographic data of the subjects are revealed in Table 1. Diabetes mean age 63.6±10.9 years and control group mean age 63.4±10.4 years,there is no significant difference in age distribution between this two groups. No gender predilection was showed in ocular surface parameters(Table 1).
In diabetes group,the incidence rate of dry eye disease was higher compared to the control group, with a significant difference.The OSDI was significantly higher in diabetes group (6.4±1.7;P<0.01) than the control group, while the TBUT was significantly lower (6.1±1.7;P<0.01) compared to the control group. The tear secretion (SⅠt) and TMH were both significantly lower in the diabetic group (5.7±1.6, 176±19.6,P<0.01). In diabetic group,the corneal fluorescein staining present minimum staining points were higher(6.3±1.6),compared to the control group, with significant differences (P<0.01). All participants proceeded clinical examination are presented in Table 2.
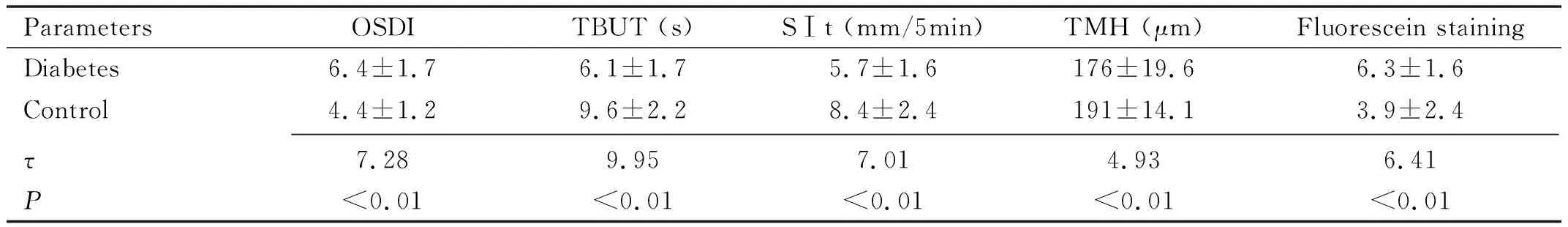
Table 2 Dry eye parameters in diabetes group and control group
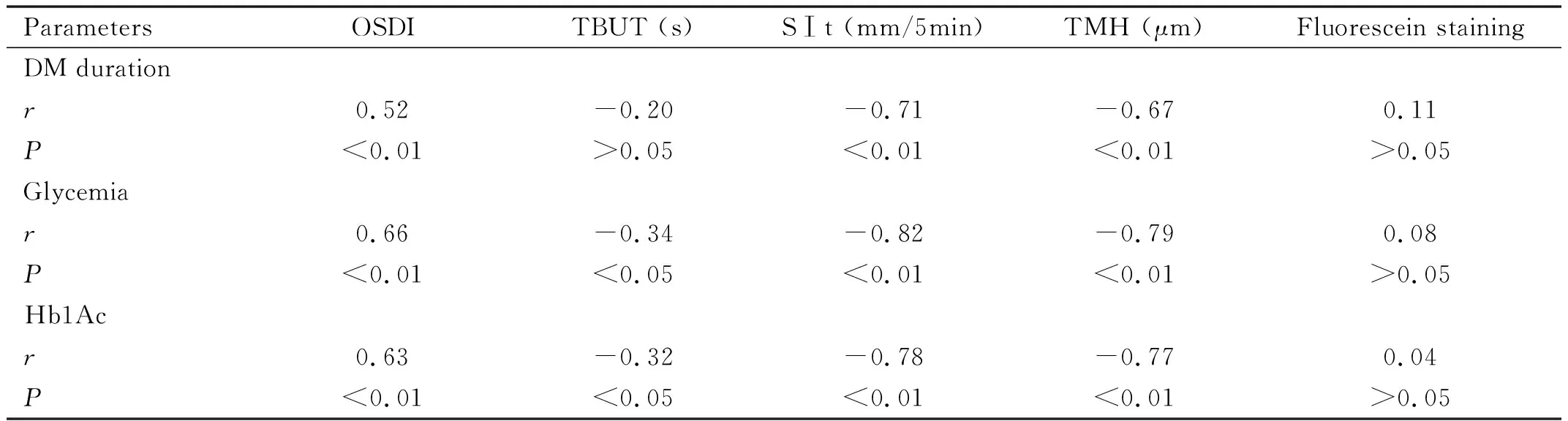
Table 3 Correlations in diabetes group
A positive correlations was found between OSDI and the DM duration, glycemia and Hb1Ac (r=0.52,r=0.66,r=0.63),with statistical significance (P<0.01). TBUT showed negative correlation with glycemia and Hb1Ac in diabetics participants (r=-0.34,P=0.012;r=-0.32,P=0.013), however it showed a negative correlation with the duration of diabetes (r=-0.20,P=0.034), although it was no statistical significance. The tear secretion (SⅠt) showed a negative correlation with the DM duration (r=-0.71,P=0.002), glycemia (r=-0.82,P=0.001) and Hb1Ac (r= -0.78,P=0.003),with significant statistical difference. The TMH showed a negative correlation with the duration of diabetes (r=-0.67,P=0.004), glycemia (r=-0.79,P=0.003) and Hb1Ac (r= -0.77,P=0.003). The correlation between the fluorescein staining and the DM duration, glycemia and Hb1Ac was of no statistical significance (P>0.05). The correlation between the different studied parameters in diabetes group is summarized in Table 3.
DISCUSSION
Diabetes is a chronic and metabolic disease that affects 422 million people worldwide (WHO, 2016). Diabetes mellitus is a systemic disease that influences the ocular surface balance through different mechanisms and affects mainly the microcirculation[15]. However the neuropathic damage and angiopathic, not only influences the retina of the eye, but also it is related to dry eye, persistent corneal defects,inflammation of the ocular surface, and changes in the lacrimal glands; these transformations are related to the oxidative stress and hypoxia by glucose alterations. Abnormalities in innervation lead to impaired tear production, as well as reduced vegetative stimulus and parasympathetic motor[16]creating inflammatory courses at the ocular surface[7-8].
Tear film plays an important role in ocular surface immune protection and corneal health. And the tear film is mainly created by the lacrimal gland that presents signs of hyperglycemia-related inflammation,oxidative stress, and accumulates AGEs in diabetes[17]. Consequently, tear secretion is often significantly lower in diabetics than normal, and the incidence of dry eye disease in diabetic patients increases[18-19]. In diabetics, decreased stability of tear film is associated with the course of diabetes, and poor glucose control and neuropathy[20]. Decreased corneal sensitivity has been shown to be common in diabetic patients and animals.The degree is related to the severity of the disease[21-22].
In this study, we tried to observe the influence of diabetes on the tear secretion and tear film quantity and quality. We also tried to discover an association between the tear film parameters, tear secretion and blood glucose, Hba1c in diabetics. According with the report of Kanetal[23]the incidence of dry eye is closely related to the level of blood glucose and Hba1c. The higher the level of blood glucose and Hba1c, the higher the mobidity of dry eye. Yau reported that the course of DM is closely related to the incidence of dry eye. Our results are in accordance with the results of Kan and Yau that we found a statistically significant decreases in tear film stability (TBUT values) and TMH, SⅠt, and increase in ocular symptoms (OSDI scores), which were significantly correlated with the DM duration, blood glucose and HbA1c in the diabetics.
The results of this study showed that the level of tear secretion, TBUT and tear river was lower than that in the control group,the OSDI and the corneal fluorescein staining in the diabetic group was higher, with statistically significant differences. A recent study presented that the lower TBUT and Schirmer test scores in diabetes were not different from controls significantly[24]. Garzónetal[6]showed that the corneal fluorescein staining has no significant differences in diabetes from controls.
Akincietal[25]and Manaviatetal[26]both used TBUT and Schirmer tests to suggest a relationship between diabetes duration and dry eye, which was confirmed in this study. The results of our research showed that the course of disease was significantly correlated with dry eye score, tear secretion, lacrimal river height, indicating that with the extension of the course of diabetes, the tear secretion would be less, and the symptoms of dry eye discomfort would be more serious. Anterior studies have confirmed a significant association between the presence/duration of DM and TBUT and Schirmer test scores[5,25-26]. As we see, our research does confirm the previous studies’ results. Corneal fluorescein staining showed no significant correlation with glycemia and Hb1Ac and the duration of diabetes, which was not consistent with previous research[13,16].
TBUT, tear secretion and TMH showed significant and inverse correlation with glycemia and Hb1Ac in diabetic patients; while OSDI presented significant and positive correlation with glycemia and Hb1Ac,indicating that the higher fasting glucose, the worse control resulted the worse ocular surface and the higher incidence of diabetic dry eyes. In a recent study, Moduloetal[24]presented a positive correlation between TBUT and Hb1Ac and blood glucose. However, Garzónetal[6]did not find an association between glycemia and Hb1Ac levels and TMH.
Several limitations in this study, such as small sample size, lack of age and gender grouping, and further studies are still warranted to verified our discoveries. With the increasing number of diabetic patients, eye surface diseases of diabetic patients are gradually paid attention to improve the symptoms of dry eyes and delay the course of disease, so as to help improve the quality of life of diabetic patients become very significant. Recent studies have suggested that the main causes of diabetic ocular surface disease may be changes in the quality and quantity of tears,corneal nerve damage,and the destruction of corneal epithelial structure and function[5,18]. Numerous clinical studies have presented that patients with diabetes are prone to abnormal ocular surface[7,16,27-28].
Although the mechanism of dry eye is multifactorial in diabetes, where the diagnosis should be based on the measurement of numerous tear parameters instead of a single one. Therefore, for patients with diabetes, especially those with a long-term course of disease and poor blood glucose control, regular routine examinations related to dry eyes should be carried out, and timely treatment such as protecting eye surface and improving dry eyes should be given.
