Which scope is appropriate for endoscopic retrograde cholangiopancreatography after Billroth II reconstruction:An esophagogastroduodenoscope or a colonoscope?
2020-10-21MitsuruSugimotoTadayukiTakagiReiSuzukiNaokiKonnoHiroyukiAsamaYukiSatoHirokiIrieKoWatanabeJunNakamuraHitomiKikuchiMikaTakasumiMinamiHashimotoTsunetakaKatoTakutoHikichiHiromasaOhira
Mitsuru Sugimoto,Tadayuki Takagi,Rei Suzuki,Naoki Konno,Hiroyuki Asama,Yuki Sato,Hiroki Irie,Ko Watanabe,Jun Nakamura,Hitomi Kikuchi,Mika Takasumi,Minami Hashimoto,Tsunetaka Kato,Takuto Hikichi,Hiromasa Ohira
Mitsuru Sugimoto,Tadayuki Takagi,Rei Suzuki,Naoki Konno,Hiroyuki Asama,Yuki Sato,Hiroki Irie,Ko Watanabe,Jun Nakamura,Hitomi Kikuchi,Mika Takasumi,Hiromasa Ohira,Department of Gastroenterology,School of Medicine,Fukushima Medical University,Fukushima 9601247,Japan
Ko Watanabe,Jun Nakamura,Minami Hashimoto,Tsunetaka Kato,Takuto Hikichi,Department of Endoscopy,Fukushima Medical University Hospital,Fukushima 9601247,Japan
Abstract BACKGROUND Recently,with the advent of more advanced devices and endoscopic techniques,endoscopic retrograde cholangiopancreatography (ERCP) in Billroth II (B-II)patients has been increasingly performed.However,the procedures are difficult,and the techniques and strategies have not been defined.AIM To reveal the appropriate scope for ERCP in B-II patients.METHODS Sixty ERCP procedures were performed on B-II patients between June 2005 and May 2018 at Fukushima Medical University Hospital,and in 44 cases,this was the first ERCP procedure performed by esophagogastroduodenoscopy (EGDS) or colonoscopy (CS) after B-II gastrectomy.These cases were divided into two groups:17 cases of ERCP performed by EGDS (EGDS group) and 27 cases of ERCP performed by CS (CS group).The patient characteristics and ERCP procedures were compared between the EGDS and CS groups.RESULTS The procedural time was significantly shorter in the EGDS group than in the CS group [median (range):60 (20-100) vs 90 (40-128) min,P value <0.01].CS was an independent factor of a longer ERCP procedural time according to the univariate and multivariate analyses (odds ratio:3.97,95%CI:1.05-15.0,P value = 0.04).CONCLUSION Compared to CS,EGDS shortened the procedural time of ERCP in B-II patients.
Key words:Endoscopic retrograde cholangiopancreatography;Billroth II reconstruction;Esophagogastroduodenoscope;Colonoscope
INTRODUCTION
In the past,percutaneous cholangiography or biliary drainage was mainly performed in patients who underwent gastrectomy or intestinal reconstructive surgery[1].Recently,with the advent of more advanced devices and endoscopic techniques,endoscopic cholangiography and biliary drainage have been increasingly performed in these patients.Although endoscopic retrograde cholangiopancreatography (ERCP) in Billroth II (B-II) patients has been previously reported[2-19],the procedures are difficult,and the techniques and strategies have not been defined.
Initially,ERCP was performed in B-II patients using a side-viewing endoscope[2,3].However,it is difficult to insert the side-viewing endoscope into the afferent loop,and the risk of bowel perforation was reported to be greater for ERCP in B-II patients when a side-viewing endoscope was used than when a forward-viewing endoscope was used[20].Therefore,a forward-viewing endoscope has recently been used for this procedure and has been shown to be as effective as a side-viewing endoscope for ERCP in B-II patients[20-22].
Among the reports describing the use of a forward-viewing endoscope,some have described the use of esophagogastroduodenoscopy (EGDS)[9,12,15,17,19],and others have described the use of long endoscopes (e.g.,a colonoscope,single-balloon endoscope,or double-balloon endoscope)[7,8,16,19].Therefore,this study aimed to reveal which scope(an esophagogastroduodenoscope or a colonoscope) is appropriate for ERCP in B-II patients.
MATERIALS AND METHODS
Study design and ethics
This study was a retrospective study to investigate the appropriate scope for ERCP in B-II patients.This study was approved by the Institutional Review Board of Fukushima Medical University.
Patients
Sixty ERCP procedures were performed in B-II patients between June 2005 and May 2018 at Fukushima Medical University Hospital (Figure 1).Among these cases,44 involved ERCP by EGDS or colonoscopy (CS) after B-II gastrectomy.Sixteen cases were excluded from this study because in these cases,this was not the first ERCP performed by EGDS or CS.Five cases involved ERCP by both EGDS and CS.The 44 patients were divided into two groups:17 cases of ERCP by EGDS (EGDS group) and 27 cases of ERCP by CS (CS group).Patients were not required to provide informed consent for this study because this investigation used anonymous clinical data obtained after each patient had agreed to examination or treatment by written consent.For full disclosure,see the details of this study published on the home page of Fukushima Medical University.
Endoscopic retrograde cholangiopancreatography procedure
Before ERCP was started,patients were intravenously administered 300 mg of gabexate mesylate.After the patients were sedated with midazolam under blood pressure and oxygen saturation monitoring,an endoscope with a cap attached to the tip was inserted.The endoscope used was randomly chosen by each endoscopist.After the entrance of both the afferent loop and the efferent loop was observed,the endoscope was advanced to the afferent loop,reaching the papilla of Vater.Insertion into the afferent loop was performed with confirmation of the running direction by Xray images.In the EGDS group,cannulation was initiated after the papilla was turned to the 9 to 11 o’clock position (Figure 2A).In the CS group,cannulation was initiated after the papilla was turned to the 6 o’clock position (Figure 3A and B).In patients with biliary or pancreatic ductal strictures,a biliary stent was inserted after endoscopic sphincterotomy (EST).
In patients with biliary ductal stones,EST and endoscopic papillary balloon dilation(EPBD) or endoscopic papillary large balloon dilation (EPLBD) were performed,as appropriate (Figures 2 and 3).EPBD was performed if the transverse diameter of the largest stone was >8 mm and bile duct stones were difficult to remove by EST alone or if a peripapillary diverticulum was present.EPLBD was performed if the transverse diameter of the largest stone was >12 mm,if many bile duct stones were difficult to remove by EST alone or if sufficient EST was difficult because of a peripapillary diverticulum.Stones that were too large to be ejected after EPBD or EPLBD were destroyed by catheter fragmentation.If complete stone clearance was difficult,then a biliary stent was inserted.
A GIF-Q240X,GIF-Q260,or GIF-Q260J (Olympus,Tokyo,Japan) scope was used in the EGDS group.A PCF-Q260AI,PCF-Q260AL,PCF-PQ260L,or SIF-Q260 (Olympus)scope was used in the CS group.PCF-PQ260L and SIF-Q260 scopes were used in one patient each.A D-201-11304 (Olympus) was used as the cap attached to the tip of the GIF-Q240 scope.A D-201-10704 (Olympus) was used as the cap attached to the tip of the GIF-Q260 scope.A D-201-12704 (Olympus) was used as the cap attached to the tip of the PCF-Q260AI and PCF-Q260AL scopes.A D-201-10704 (Olympus) was used as the cap attached to the tip of the PCF-PQ260L and SIF-Q260 scopes.A Tandem XL(Boston Scientific Japan,Tokyo,Japan),MTW ERCP tapered catheter (MTW Endoskopie,Wesel,Germany) or a Swing Tip PR-233Q (Olympus) was used as the ERCP catheter.EST was performed using an RX needle knife XL (Boston Scientific) or Billroth II sphincterotome (Cook Japan,Tokyo,Japan).A Hurricane RX biliary balloon dilatation catheter (Boston Scientific) was used for EPBD.A CRE biliary balloon dilatation catheter (Boston Scientific) or a Giga or Giga II balloon (Century Medical,Tokyo,Japan) was used for EPLBD.A Trapezoid RX basket catheter (Boston Scientific)or an FG-V425PR basket catheter (Olympus) was used to crush and remove stones.A Flexima biliary stent (Boston Scientific) or a Zimmon biliary stent (Cook Japan,Tokyo,Japan) was used as the biliary stent.All of these devices can be used with both the GIFQ260J and PCF-Q260AI colonoscopes.The Swing Tip PR-233Q,Hurricane RX biliary balloon dilatation catheter,Giga balloon,Trapezoid RX basket catheter,and Flexima biliary stent cannot be used with both the GIF-Q240X and the GIF-Q260 scopes.The Swing Tip PR-233Q,Hurricane RX biliary balloon dilatation catheter,and Trapezoid RX basket catheter cannot be used with the PCF-Q260AL scope.In the two patients in whom the PCF-PQ260AL or SIF-Q260 scope was used,the papilla of Vater could not be observed,and ERCP devices were not used with the scope.
Examination items

Figure 1 Target of this study.
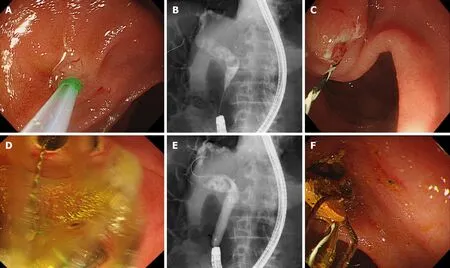
Figure 2 A case from the esophagogastroduodenoscopy group.
The characteristics of the patients (age,sex,period after B-II reconstruction,diseases treated with B-II reconstruction,untreated papilla of Vater,antithrombotic drug use,periampullary diverticulum,diseases,transverse diameter of the largest stone,and number of stones) and ERCP procedure details [EST,EPBD or EPLBD,procedural time,papilla of Vater access,stone clearance,stone destruction,procedural success,and post-ERCP pancreatitis (PEP)] were compared between the EGDS and CS groups.Additionally,the relationship between the duodenal and catheter directions (cross or parallel) and the observation of papilla of Vater in the front were compared as factors of scope usability between the EGDS and CS groups (Figure 4).The duodenal and catheter directions were determined from the X-ray images of the biliary cannulation.An untreated papilla of Vater was defined as one that had not undergone incision or dilation.If all biliary stones were removed,the intended procedures (for example,biliary duct or pancreatic duct investigation or stenting) were performed using the first endoscope,and this was defined as stone clearance or procedural success.The diagnosis of PEP was performed according to Cotton’s criteria[23].If patients were observed to have an elevated serum amylase level more than three times the normal upper limit with abdominal pain at more than 24 h after ERCP,they were diagnosed with PEP.Furthermore,peripancreatic inflammation was confirmed in all PEP cases by contrast-enhanced CT.
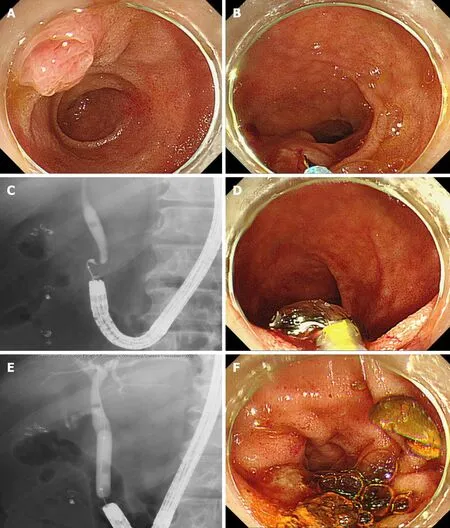
Figure 3 A case from the colonoscopy group.
Statistical analysis
Age,period after B-II reconstruction,and transverse diameter of the largest stone were compared by Student’sttest.The procedural time and number of stones were compared using the Mann-WhitneyUtest.Nominal variables were compared by Fisher’s exact test.Factors influencing the ERCP procedural time were investigated by logistic regression analysis.APvalue <0.05 was defined as statistically significant.All statistical analyses were performed using the EZR platform (Saitama Medical Center,Jichi Medical University,Saitama,Japan),which is a graphical user interface for R (The R Foundation for Statistical Computing,Vienna,Austria).EZR is a modified version of the R commander,which was designed to perform functions that are frequently used in biostatistics[24].

Figure 4 The duodenal and catheter directions in esophagogastroduodenoscopy and colonoscopy groups.
RESULTS
The patient characteristics were not significantly different between the two groups(Table 1).The ERCP procedural time was significantly shorter in the EGDS group than in the CS group [median (range):60 (20-100)vs90 (40-128) min,Pvalue <0.01](Table 2).
The procedural success rate was not significantly different between the EGDS group and the CS group (82.4%vs63.0%,Pvalue = 0.20).Procedural success was difficult to achieve in three patients in the EGDS group.Among them,one patient underwent surgery;in another patient,procedural success by ERCP was not achieved using an SIF-H290-S (Olympus) single-balloon scope,and the patient finally underwent conservative treatment;in the last patient,procedural success was not achieved by ERCP using an SIF-H290-S scope but was finally achieved by ERCP using a PCFQ260AL scope.Procedural success was not achieved in ten patients in the CS group.Among them,procedural success was achieved in four patients by ERCP using a Q260J scope and in one patient by a second ERCP procedure using a PCF-Q260AI scope.Percutaneous transhepatic biliary drainage was performed in four patients(procedural success was achieved in two patients by ERCP with the rendezvous technique).One patient subsequently underwent conservative treatment.
CS was an independent factor of a longer ERCP procedural time,as determined by univariate and multivariate analyses (Table 3).
Regarding the factors influencing scope usability,crossing of the duodenal and catheter directions was observed more often in the EGDS group than in the CS group(cross/parallel:11/3vs8/15,Pvalue = 0.02) (Table 4).Observation of the papilla of Vater in the front was achieved more often in the EGDS group than in the CS group.
DISCUSSION
In this study,EGDS was compared with CS for performing ERCP in B-II patients.The results showed that compared to CS,EGDS shortened the ERCP procedural time.
An increasing number of ERCP procedures after gastrectomy have been performed in patients who have undergone B-II reconstruction,and several scopes have been used.As mentioned in the introduction,the side-viewing endoscope was initially used for ERCP in B-II patients[2,3].However,recently,forward-viewing endoscopes have been used.Byunet al[9],Parket al[12],Kiet al[17],and Janget al[15]used an esophagogastroduodenoscope.However,Abdelhafezet al[19]used a colonoscope,and Itoiet al[7]and Kawamuraet al[16]used a single-balloon enteroscope.Linet al[8]used a double-balloon endoscope.Although it is unknown which scope is most efficient,the esophagogastroduodenoscope was reported to shorten the procedural time.In most reports,the procedural time was not described.However,a study reported that the average EGDS procedural time was 36.3 min[15],which is a short time.EGDS was superior to procedures with a longer scope because the papilla of Vater can be observed in the front (Figures 2A,3A,3B,4A,4B,4E,5A,and 5B) because the esophagogastroduodenoscope can be curved up to 210 degrees,while a colonoscope can be curved up to 180 degrees.The duodenal direction and the catheter direction could easily be crossed in ERCP using EGDS (Figure 4 and Table 4).However,these two directions tended to run parallel in ERCP using CS.In fact,in three cases,it was difficult to cannulate the bile duct by CS,whereas bile duct cannulation was successful by EGDS (Figure 5).
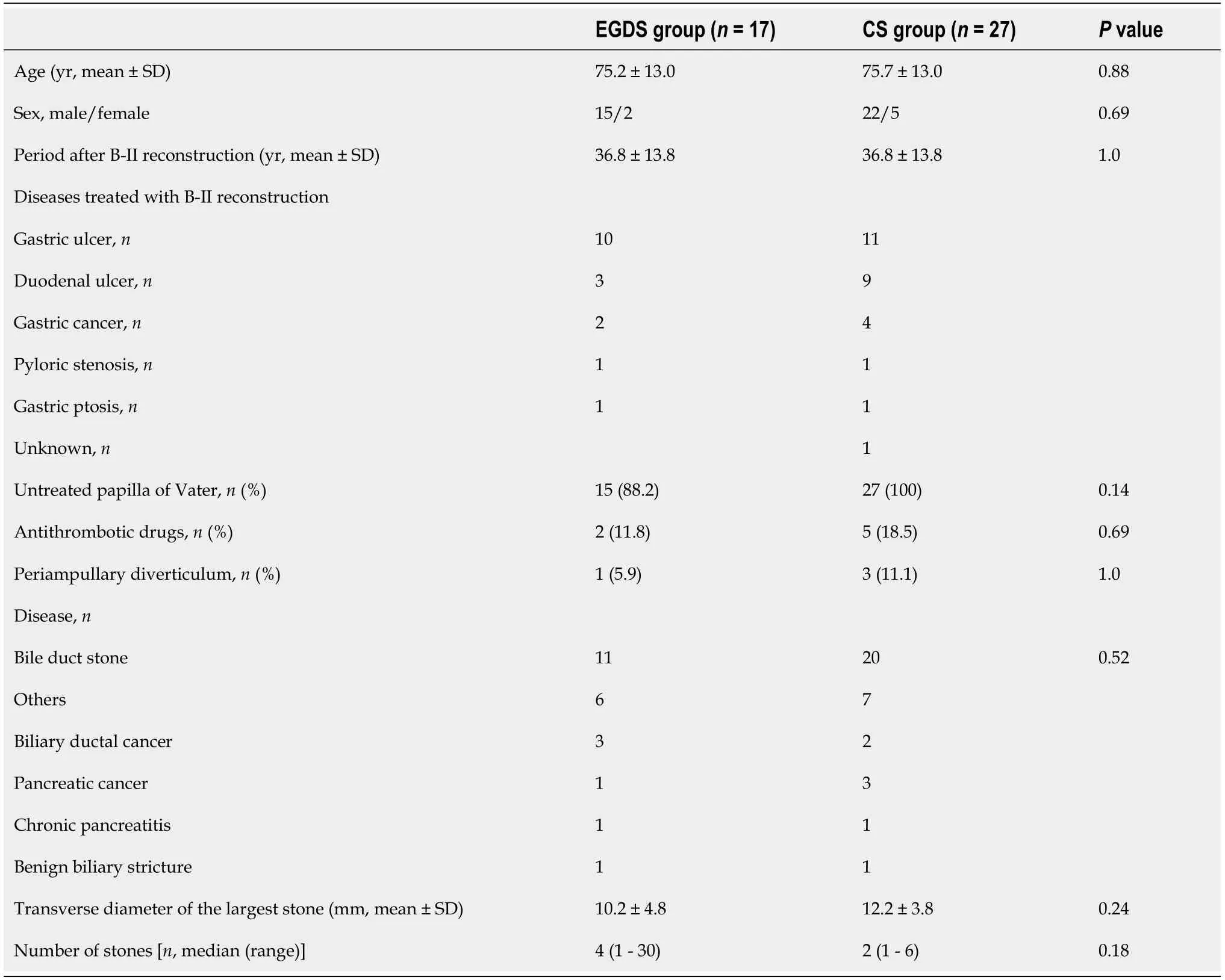
Table 1 Comparison of patient characteristics between the esophagogastroduodenoscopy and colonoscopy groups
Interestingly,although the procedural success rate was not significantly different between the two groups,the procedural time was shorter in the EGDS group.For patients who have undergone B-II reconstruction,the radiation exposure dose is decreased with EGDS.The exposure dose is also lower for the medical staff,who can thus perform more ERCP procedures.As such,EGDS is the first choice for ERCP in patients who have undergone B-II reconstruction.

Table 2 Comparison of endoscopic retrograde cholangiopancreatography procedural characteristics between the esophagogastroduodenoscopy and colonoscopy groups
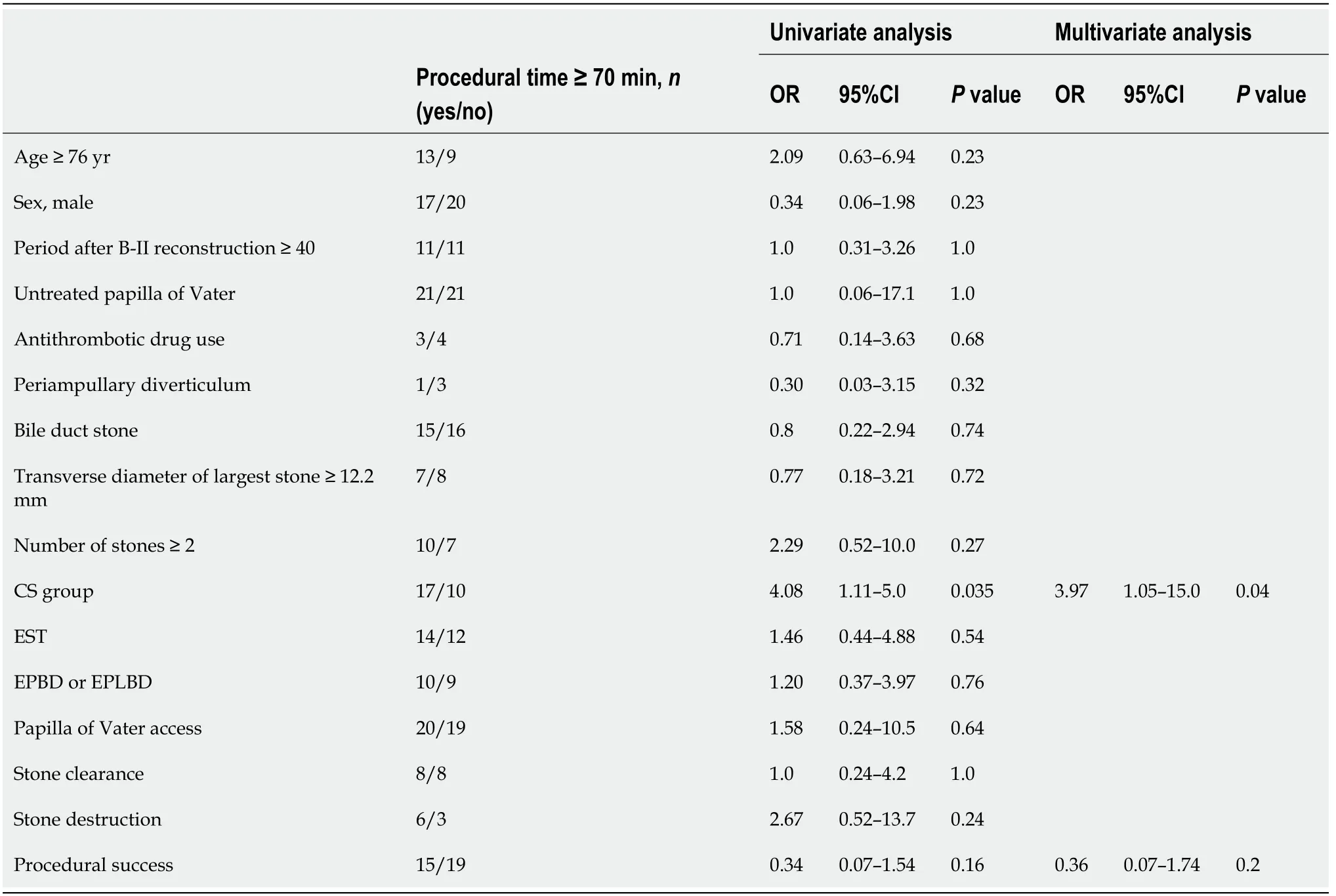
Table 3 Factors influencing the endoscopic retrograde cholangiopancreatography procedural time
There are several limitations to this study.First,this study was a retrospective and small study,and it was performed at a single institute.In the future,prospective and multicenter studies are needed.Second,due to the retrospective nature of this study,ERCP procedures were not performed by specified endoscopists.However,ERCP was performed by pancreaticobiliary specialists who had experience performing at least 2000 ERCP procedures or by trainees under the guidance of these specialists.Therefore,the quality of the ERCP procedure was constant.Third,the exact cannulation time was not recorded.However,as described above,the scope was chosen randomly.Additionally,the patient characteristics,diameter or number of stones,and factors related to ERCP were not significantly different between the two groups.Therefore,if EGDS is used for ERCP in B-II patients,the duration of the whole procedure,including insertion and cannulation,could be shortened.
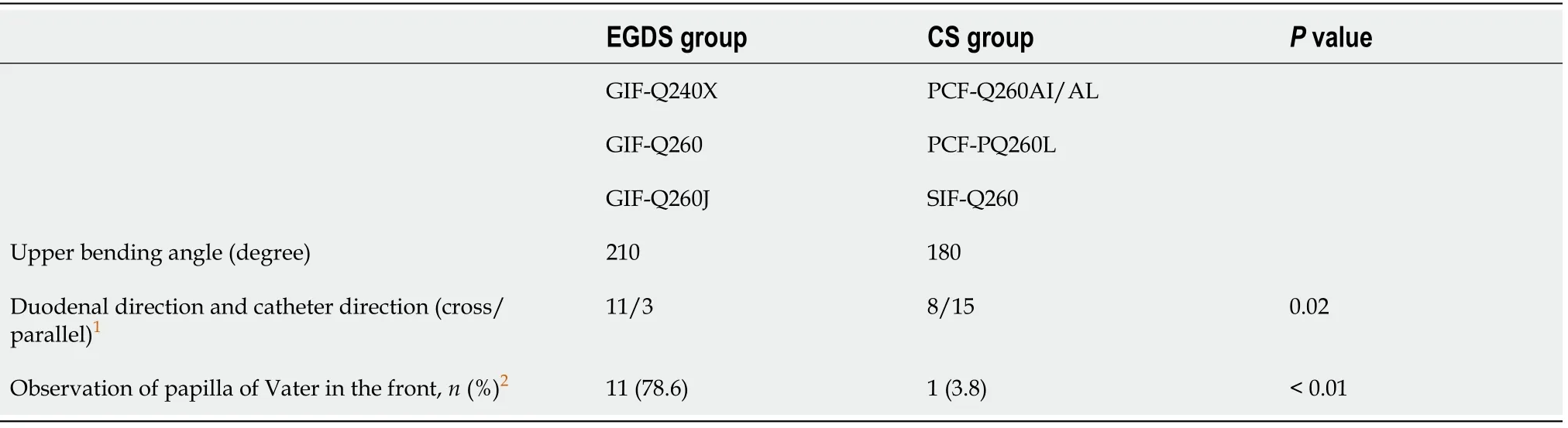
Table 4 The upper bending angle of esophagogastroduodenoscopy was greater than that of colonoscopy

Figure 5 A case of treatment that was not successful by colonoscopy was successful by esophagogastroduodenoscopy.
Research conclusions
Compared to a longer scope,the esophagogastroduodenoscope shortened the procedural time of ERCP for patients who had undergone B-II reconstruction.
ARTICLE HIGHLIGHTS
Research background
Recently,with the advent of more advanced devices and endoscopic techniques,endoscopic retrograde cholangiopancreatography (ERCP) in Billroth II (B-II) patients has been increasingly performed.However,the procedures are difficult,and the techniques and strategies have not been defined.
Research motivation
The forward-viewing endoscope has been used for ERCP in B-II patients.By using the forward-viewing endoscope,ERCP in B-II patients was performed safely and as effectively as ERCP using a side-viewing endoscope.As forward-viewing endoscopes,esophagogastroduodenoscopy (EGDS) or colonoscopy (CS) is used for ERCP in B-II patients.However,which scope (EGDS or CS) should be used remains unknown.
Research objectives
To reveal the appropriate scope for ERCP in B-II patients.
Research methods
For the 44 included cases,this was the first ERCP procedure performed by EGDS or CS after B-II gastrectomy.These cases were divided into two groups:17 cases of ERCP by EGDS (EGDS group) and 27 cases of ERCP by CS (CS group).The patient characteristics and ERCP procedures were compared between the EGDS and CS groups.
Research results
The procedural time was significantly shorter in the EGDS group than in the CS group.CS was an independent factor of a longer ERCP procedural time.
Research conclusions
Compared with CS,EGDS shortened the procedural time of ERCP for patients who had undergone B-II reconstruction.
Research perspectives
The results in this study could contribute to choosing an ERCP scope for patients who have undergone B-II reconstruction.
ACKNOWLEDGEMENTS
We thank all of the staff at the Department of Gastroenterology of Fukushima Medical University,the Department of Endoscopy of Fukushima Medical University Hospital,and the gastroenterology ward of Fukushima Medical University Hospital.We also thank American Journal Experts for providing English language editing.
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Propofol vs midazolam sedation for elective endoscopy in patients with cirrhosis:A systematic review and meta-analysis of randomized controlled trials
- Endoscopic ultrasound-guided fiducial marker placement in pancreatic cancer:A systematic review and meta-analysis
- Improved diagnostic yield of endoscopic ultrasound-fine needle biopsy with histology specimen processing
