Improved diagnostic yield of endoscopic ultrasound-fine needle biopsy with histology specimen processing
2020-10-21LawrenceKuMohammadShahshahanLindaHouViktorEysseleinSofiyaReicher
Lawrence Ku,Mohammad A Shahshahan,Linda A Hou,Viktor E Eysselein,Sofiya Reicher
Lawrence Ku,Mohammad A Shahshahan,Linda A Hou,Viktor E Eysselein,Sofiya Reicher,Department of Medicine,Division of Gastroenterology and Hepatology,Harbor-UCLA Medical Center,Torrance,CA 90509,United States
Abstract BACKGROUND Endoscopic ultrasound-guided fine needle biopsy (EUS-FNB) has emerged as a safe,efficacious alternative to fine needle aspiration (FNA) for tissue acquisition.EUS-FNB is reported to have higher diagnostic yield while preserving specimen tissue architecture.However,data on the optimal method of EUS-FNB specimen processing is limited.AIM To evaluate EUS-FNB with specimen processing as histology vs EUS-FNA cytology with regards to diagnostic yield and specimen adequacy.METHODS All EUS-FNA and EUS-FNB performed at our institution from July 1,2016,to January 31,2018,were retrospectively analyzed.We collected data on demographics,EUS findings,pathology,clinical outcomes,and procedural complications in two periods,July 2016 through March 2017,and April 2017 through January 2018,with predominant use of FNB in the second data collection time period.FNA specimens were processed as cytology with cell block technique and reviewed by a cytopathologist;FNB specimens were fixed in formalin,processed for histopathologic analysis and immunohistochemical staining,and reviewed by an anatomic pathologist.Final diagnosis was based on surgical pathology when available,repeat biopsy or imaging,and length of clinical follow up.RESULTS One hundred six EUS-FNA and EUS-FNB procedures were performed.FNA alone was performed in 17 patients;in 56 patients,FNB alone was done;and in 33 patients,both FNA and FNB were performed.For all indications,diagnostic yield was 47.1% (8/17) in FNA alone cases,85.7% (48/56) in FNB alone cases,and 84.8% (28/33) in cases where both FNA and FNB were performed (P = 0.0039).Specimens were adequate for pathologic evaluation in 52.9% (9/17) of FNA alone cases,in 89.3% (50/56) of FNB alone cases,and 84.8% (28/33) in cases where FNA with FNB were performed (P = 0.0049).Tissue could not be aspirated for cytology in 10.0% (5/50) of cases where FNA was done,while in 3.4% (3/89) of FNB cases,tissue could not be obtained for histology.In patients who underwent FNA with FNB,there was a statistically significant difference in both specimen adequacy (P= 0.0455) and diagnostic yield (P = 0.0455) between the FNA and FNB specimens(processed correspondingly as cytology or histology).CONCLUSION EUS-FNB has a higher diagnostic yield and specimen adequacy than EUS-FNA.In our experience,specimen processing as histology may have contributed to the overall increased diagnostic yield of EUS-FNB.
Key words:Fine needle biopsy;Endoscopic ultrasound;Fine needle aspiration;Pancreatic cancer;Histology;Cytopathology
INTRODUCTION
Endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) is a well-established modality for tissue acquisition of a variety of lesions in the gastrointestinal tract and surrounding structures.It has low complication rates and high diagnostic yield[1,2].
However,several factors can limit the sensitivity of EUS-FNA.EUS-FNA samples are typically processed as cytology,which does not allow for preservation of tissue architecture necessary for diagnosis of diseases such as gastrointestinal stromal tumor(GIST)[3],lymphoma[4],autoimmune pancreatitis[5],and pancreatic lesions with nonhypovascular contrast-enhancement pattern on EUS[6].The diagnostic yield of EUSFNA may be further compromised by the limited availability of on-site cytopathologists[7-11].
EUS-guided fine needle biopsy (EUS-FNB) has emerged as an alternative to EUSFNA for tissue acquisition,with a reported similar rate of complications[12,13].Initial studies have demonstrated its non-inferiority and possible superiority,depending on the indication[14-19].FNB needle tip design enables the procurement of an intact core tissue,and the preserved architecture allows for histological and immunohistochemical evaluation.Studies differ in their approach to FNB sample processing as histologyvscytology.There is limited data on which approach is preferable.
We evaluate the performance of EUS-FNB with specimen processing as histologyvsEUS-FNA cytology with regards to diagnostic yield and specimen adequacy.
MATERIALS AND METHODS
Data was retrospectively collected on all patients who underwent EUS-FNA or EUSFNB from July 1,2016,to January 31,2018,at our institution,a large tertiary safety-net hospital.Data was collected in two periods:July 2016 through March 2017,and April 2017 through January 2018.
Procedures were performed by three experienced endosonographers who each have performed over 1000 EUS procedures.FNA specimens were collected for cytology in Plasma-Lyte A injection solution pH 7.4 (Baxter Healthcare Corporation,Deerfield,IL,United States),processed as a cell block with the Collodion bag technique[20,21],and subsequently evaluated by a cytopathologist.FNB specimens were collected,immediately fixed in formalin,and sent to pathology,where they were processed for histopathologic analysis and immunohistochemical staining in accordance with a previously reported standardized protocol[22],and subsequently evaluated by an anatomic pathologist.Rapid on-site evaluation is not available at our institution.
Echoendoscopes used were GF-UE160-AL5,GF-UC140-AL5,GF-UC140P-AL5,and GF-UCT180 (Olympus America,Center Valley,PA,United States).EUS-FNA and FNB needles were from a variety of manufacturers:Expect FNA and Acquire FNB needles(Boston Scientific,Marlborough,MA,United States),SharkCore FNB needles(Medtronic,Sunnyvale,CA,United States),and EchoTip ProCore FNB needles (Cook Medical,Bloomington,IN,United States).
Data collected from hospital Electronic Health Records and EUS databases included patient demographics,clinical outcomes,and pathology.Procedure-related data included indications,technical aspects,and complications.
Standardized definitions of specimen adequacy and diagnostic yield were used[23].Specimen adequacy was defined as the percentage of lesions sampled in which the specimens were from the intended site and sufficient for diagnosis by a pathologist.Acellular or hypocellular samples were considered inadequate.Diagnostic yield was defined as the percentage of lesions sampled in which a tissue diagnosis was obtained.Final diagnosis was based on surgical pathology when available,repeat biopsy or imaging,and length of clinical follow up.
The study was approved by the Institutional Review Board (#31297-01).
Statistical analysis
Statistical analysis was performed using Fisher’s exact test,Kruskal-Wallis test,and McNemar’s test,withPvalue <0.05 as statistically significant.The Bonferroni correction was applied to all sub-group analyses.All analyses were performed with R,version 3.6.0 (R Core Team,Vienna,Austria),and reviewed by a biostatistician,Youngju Pak,Ph.D.,from the UCLA Clinical and Translational Science Institute at Harbor-UCLA Medical Center.
RESULTS
Demographics
From July 2016 through January 2018,EUS-FNA or EUS-FNB was performed in 106 procedures in 97 patients.The mean patient age was 55.5 years (23-84),and 41.5%were males (Table 1).
The most common indications were pancreatic mass 31.1% (33/106),gastric mass 17.9% (19/106),liver biopsy 14.2% (15/106),and pancreatic cyst 13.2% (14/106).Other conditions evaluated included lymph nodes,biliary abnormalities,extraluminal lesions,pancreatitis,rectal masses,small bowel lesions,mediastinal lesions,and esophageal lesions (Table 2).
FNA alone was performed in 17 cases (16.0%);in 56 cases (52.8%),FNB alone was done;and in 33 cases (31.2%),FNA with FNB was performed.There was an overall mean of 3.3 (1-8) passes per needle;the mean was 3.4 (1-5) passes per needle in FNA alone cases,3.4 (1-8) in FNB alone cases,and 2.8 (1-8) in cases where both FNA and FNB were performed (Table 1).The most commonly used needle size was 22-Gauge;a 22-Gauge FNA needle was used in 60.0% (30/50) of FNA needle cases,and a 22-Gauge FNB needle was used in 82.0% (73/89) of FNB cases.
Diagnostic yield
For all indications,diagnostic yield was 47.1% (8/17) in FNA alone cases,and 85.7%(48/56) in FNB alone cases (Table 3).
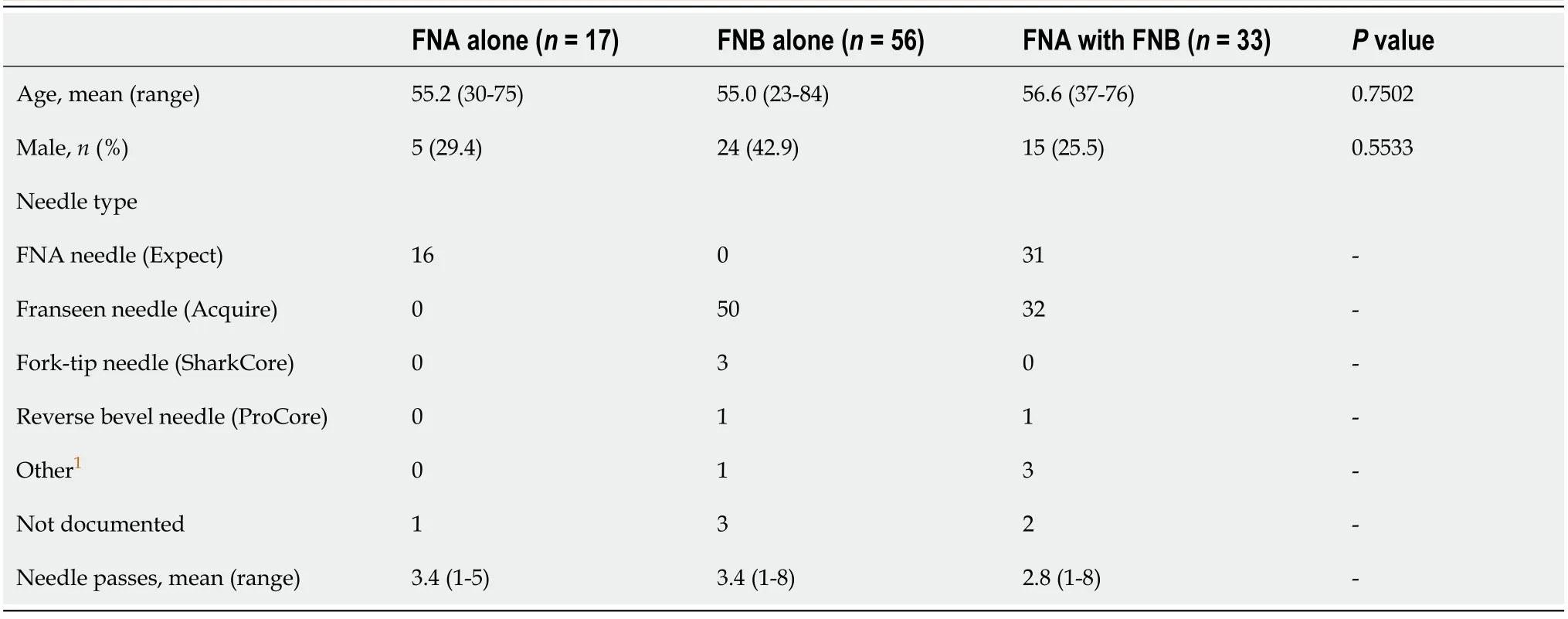
Table 1 Baseline patient and procedural characteristics
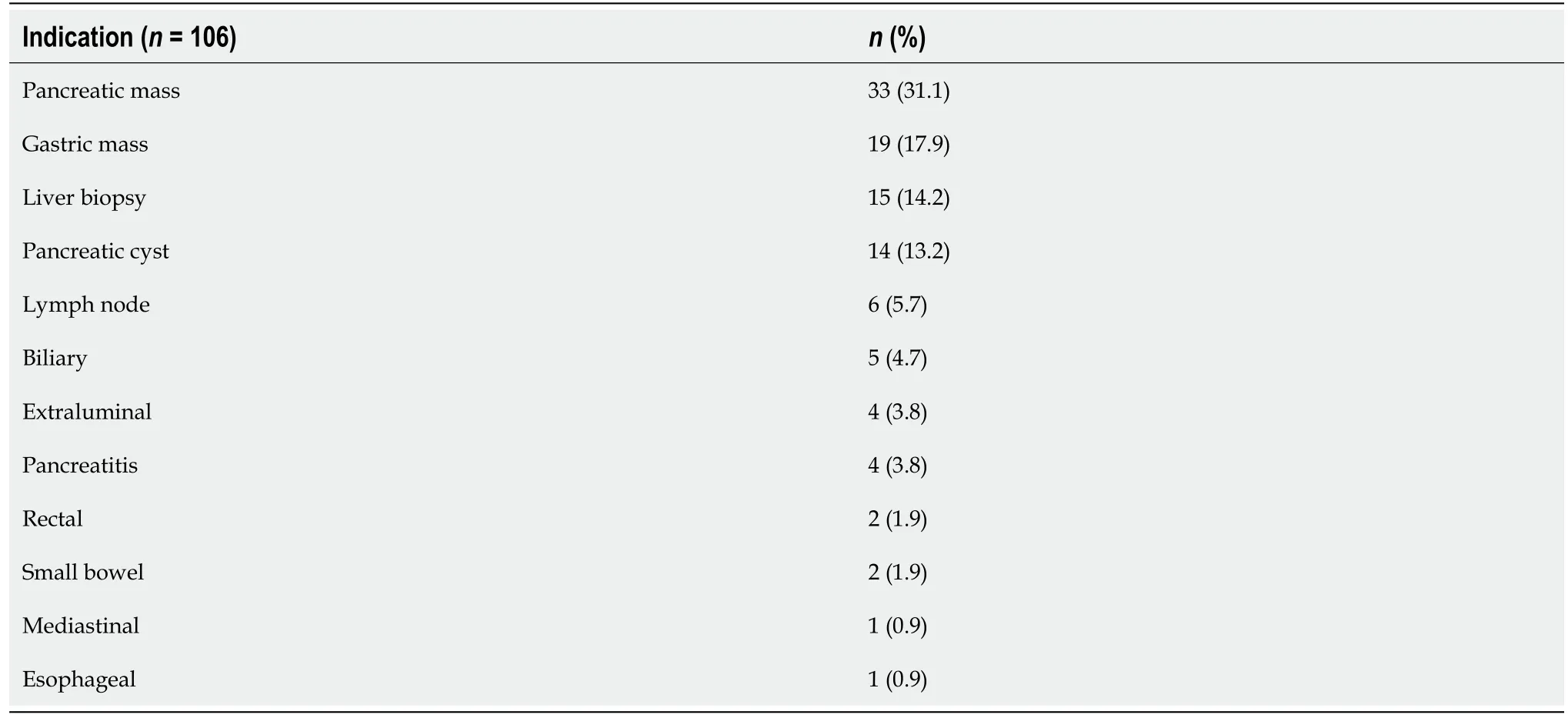
Table 2 Indications for endoscopic ultrasound-guided fine needle aspiration and endoscopic ultrasound-guided fine needle biopsy
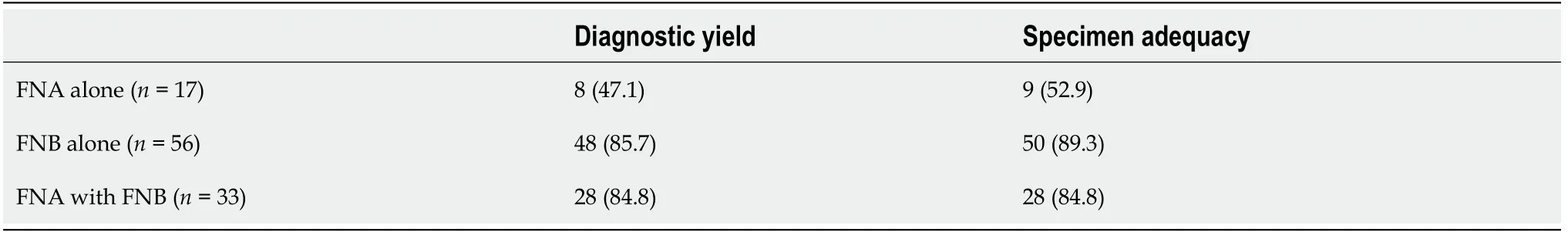
Table 3 Diagnostic yield and specimen adequacy,n (%)
There was a significant difference in diagnostic yield between the three groups(Fisher’s exact test,P= 0.0039).In sub-group analysis,there was a significant difference between the FNA alone and FNB alone groups,(Fisher’s exact test,Bonferroni adjusted,P= 0.0067) and between the FNA alone and FNA with FNB groups (Fisher’s exact test,Bonferroni adjusted,P= 0.0238),but not between the FNB alone and FNA with FNB groups (Fisher’s exact test,Bonferroni adjusted,P= 1).
In cases where both FNA and FNB were performed in the same procedure,the overall diagnostic yield was 84.8% (28/33);60.6% (20/33) in samples from FNA needles and 81.8% (27/33) in samples from FNB needles.There was a statistically significant difference in diagnostic yield (McNemar’s test,P= 0.0455) between the FNA and FNB specimen subgroups.
Specimen adequacy
Specimens were adequate in 52.9% (9/17) of FNA alone cases and adequate in 89.3%(50/56) of FNB alone cases (Table 3).
There was a significant difference in sample adequacy between the three groups(Fisher’s exact test,P= 0.0049).In sub-group analysis,there was a significant difference between the FNA alone and FNB alone groups,(Fisher’s exact test,Bonferroni adjusted,P= 0.0072),but not between the FNA alone and FNA with FNB groups (Fisher’s exact test,Bonferroni adjusted,P= 0.063),or between the FNB alone and FNA with FNB groups (Fisher’s exact test,Bonferroni adjusted,P= 1).
In cases where both FNA and FNB were performed,overall specimen adequacy was 84.8% (28/33);samples from FNA needles were adequate in 60.6% (20/33),while samples from FNB needles were adequate in 81.8% (27/33).There was a statistically significant difference in specimen adequacy (McNemar’s test,P= 0.0455) between the FNA and FNB specimen subgroups.
In 10.0% (5/50) of FNA cases,tissue could not be aspirated for cytology,while in 3.4% (3/89) of FNB cases,core tissue could not be obtained for histology.In 2 cases of pancreatic cystic lesions,when samples from FNB needles were grossly inadequate for histology,material was sent for cytology instead.
EUS-FNA/FNB of pancreatic masses
EUS-FNA or EUS-FNB performed for pancreatic masses produced adequate samples for pathologic analysis in 30/33 (90.9%).There was a trend towards improved sample adequacy from the first to second data collection time period with the predominant use of FNB (Fisher’s exact test,P= 0.0524).26 patients had pancreatic malignancy on final diagnosis.Sensitivity for pancreatic malignancy was 96.2% (25/26);one case of benign EUS-FNB was confirmed malignant operatively.There were no cases of false positive EUS-FNA or EUS-FNB.Yield for malignancy for all pancreatic masses sampled via FNA or FNB was 75.8% (25/33).Importantly,there was a significant increase in the diagnostic yield from 46.2% (6/13) in the first collection period to 95.0%(19/20) in the second data collection time period (Fisher’s exact test,P= 0.0026).Mean follow up was 29.1 months (21.7-32.4).
Complications
Two patients (1.9%) had minor post-procedural bleeding after EUS-FNB;one was selflimiting,and one required the use of a hemoclip.There were no infectious complications due to FNA or FNB in our cohort;all patients (14/14) undergoing EUSFNA of cystic lesions received prophylactic antibiotics.
DISCUSSION
The preferred approach to specimen preparation and processing of EUS-FNB samples is not well defined.In a recent trial evaluating the clinical performance of a fork-tip FNB needle (SharkCore,Medtronic,Sunnyvale,CA,United States),all FNB specimens were processed for histology[12].However,in a trial examining the clinical performance of a Franseen needle (Acquire,Boston Scientific,Marlborough,MA,United States),42.5% of FNB specimens were only sent for cytology,even though 90.3% of specimens had an adequate tissue core[13].Diagnostic concordance in cytology specimen analysis varies significantly[24,25].Inter-study heterogeneity has prevented identification of independent factors that contribute to the higher diagnostic yield of EUS-FNB noted in many studies.Recent studies have suggested alternate methods to increase diagnostic yield.In particular,contrast-enhanced EUS could be of significant benefit in characterizing pancreatic lesions[6],and touch-imprint cytology allows for processing of a single specimen for both cytology and histology[26].
Our institution has transitioned from the predominate use of EUS-FNA to EUSFNB,and thus,to processing tissue core for histology rather than cytology.In our experience,utilization of EUS-FNB led to significant improvements in both diagnostic yield and specimen adequacy,as suggested by statistically significant differences in both parameters between FNA and FNB subgroups in patients who underwent FNA and FNB for the same lesion.Our results are comparable to recently published studies demonstrating specimen adequacies of 90.3% for a Franseen needle,67% to 84.6% for a fork-tip needle,and 92.6% for a reverse bevel FNB needle (ProCore,Cook Medical,Bloomington,IN,United States)[12,13,27,28].
Limitations of our study include its retrospective nature,being a single-center experience,the use of multiple FNB needle types,and the heterogeneity of lesion types sampled.
In conclusion,EUS-FNB with subsequent processing of tissue core for histology improves diagnostic yield and specimen adequacy compared to EUS-FNA cytology.Specimen processing as histology may have contributed to the overall increased diagnostic yield of EUS-FNB.
ARTICLE HIGHLIGHTS
Research background
Endoscopic ultrasound-guided fine needle biopsy (EUS-FNB) has emerged as a safe,efficacious alternative to EUS-guided fine needle aspiration (EUS-FNA) for tissue acquisition.EUS-FNB is reported to have higher diagnostic yield while preserving specimen tissue architecture.
Research motivation
Data on the optimal method of EUS-FNB specimen processing is limited.
Research objectives
We evaluate EUS-FNB with specimen processing as histology vs EUS-FNA cytology with regards to diagnostic yield and specimen adequacy.
Research methods
A retrospective observational study of all EUS-FNA and EUS-FNB procedures performed at our institution from July 1,2016,to January 31,2018,was performed.The primary outcomes were diagnostic yield and specimen adequacy.
Research results
106 EUS-FNA and EUS-FNB procedures were analyzed.For all indications,diagnostic yield was 47.1% (8/17) in FNA alone cases,85.7% (48/56) in FNB alone cases,and 84.8% (28/33) in cases where both FNA and FNB were performed (P = 0.0039).Specimens were adequate for pathologic evaluation in 52.9% (9/17) of FNA alone cases,in 89.3% (50/56) of FNB alone cases,and 84.8% (28/33) in cases where FNA with FNB were performed (P = 0.0049).In patients who underwent FNA with FNB,there was a statistically significant difference in both specimen adequacy (P = 0.0455) and diagnostic yield (P = 0.0455) between the FNA and FNB specimens.
Research conclusions
The study suggests that EUS-FNB with processing of tissue core for histology improves diagnostic yield and specimen adequacy compared to EUS-FNA cytology.Specimen processing as histology may have contributed to the overall increased diagnostic yield of EUS-FNB.
Research perspectives
Prospective research is needed to clarify optimal specimen processing of EUS-FNB in clinical settings with varied resources.
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Propofol vs midazolam sedation for elective endoscopy in patients with cirrhosis:A systematic review and meta-analysis of randomized controlled trials
- Endoscopic ultrasound-guided fiducial marker placement in pancreatic cancer:A systematic review and meta-analysis
- Which scope is appropriate for endoscopic retrograde cholangiopancreatography after Billroth II reconstruction:An esophagogastroduodenoscope or a colonoscope?
