Outcome prediction value of National Early Warning Score in septic patients with community-acquired pneumonia in emergency department: A single-center retrospective cohort study
2020-10-17HaijiangZhouTianfeiLanShubinGuo
Hai-jiang Zhou, Tian-fei Lan, Shu-bin Guo
1 Emergency Medicine Clinical Research Center, Beijing Chao-yang Hospital, Capital Medical University & Beijing Key Laboratory of Cardiopulmonary Cerebral Resuscitation, Beijing, China
2 Department of Allergy, Beijing Shijitan Hospital, Capital Medical University, Beijing, China
KEYWORDS: Community-acquired pneumonia; Sepsis; National Early Warning Score (NEWS);Intensive care unit; Emergency departments
INTRODUCTION
Community-acquired pneumonia (CAP), a common presentation to emergency departments (EDs) with a high mortality rate, is the leading cause of sepsis.[1]Hospital admissions of CAP are increasing every year and have placed a substantial burden on healthcare resources.[2]Despite prompt and appropriate treatment, 5%-15% of patients hospitalized with CAP will die within 30 days of admission, while rising to 30% for those admitted to an intensive care unit (ICU).[3]Severity assessment and prognostic prediction are of vital significance because early identification of severe CAP patients can reduce mortality and improve prognosis.
Current guidelines recommend scoring systems like Pneumonia Severity Index (PSI) and CURB65(confusion, urea >7 mmol/L, respiratory rate ≥30/minute,blood pressure <90 mmHg [systolic] and/or ≤60 mmHg[diastolic], and age ≥65 years) as an aid for clinical evaluation.[1,4,5]The PSI is based on 20 variables and stratified patients into five risk categories based on 30-day mortality,[5,6]but the calculation complexity limits its widespread and routine adoption in primary care, EDs,or medical admission units.[5]Comparatively, the PSI and CURB65 score performed equally well at discriminating patients into mortality risk groups.[5]
The Sepsis-3 Task Force updated the clinical criteria for sepsis, excluding the need for systemic inf lammatory response syndrome (SIRS) criteria and highlighting the clinical implication of Sequential Organ Failure Assessment (SOFA) score and quick SOFA (qSOFA)score.[7,8]Sepsis was defined as a life-threatening organ dysfunction caused by a dysregulated host response to infection, and organ dysfunction was characterized by an increased SOFA score ≥2 from baseline.[7]Ranzani et al[8,9]reported the qSOFA score was an easilyused bedside stratification tool, and qSOFA ≥2 was independently associated with mortality in patients with sepsis. Moreover, other sepsis-related tools such as the Mortality in Emergency Department Sepsis (MEDS)score and National Early Warning Score (NEWS) were also used in risk stratif ication and prognostic prediction of patients with CAP.[10-12]Shapiro et al[10,11]reported the MEDS score is based on the assessment of age, terminal disease, nursing home resident, lower respiratory tract infection, respiratory rate, platelet count, band cell level,and mental status, while the NEWS score comprises parameters of respiratory rate, blood oxygen saturation,supplemental oxygen, temperature, systolic blood pressure, heart rate, and level of consciousness. Previous studies have found NEWS to be superior compared to other risk stratification tools in different settings.[12-14]Only a few studies have investigated the prediction value of NEWS for the adverse clinical outcome of CAP on admission to EDs.[11,12,15]
In this study, we investigated the accuracy of NEWS compared with other commonly used severity scores (CURB65, PSI, SOFA, qSOFA, and MEDS) and admission lactate levels in predicting clinical outcomes(28-day mortality, ICU admission, and mechanical ventilation use) for septic patients with CAP in ED.
METHODS
This was a retrospective, single-center cohort study carried out in Beijing Chao-yang Hospital,Capital Medical University, which is a tertiary teaching hospital with approximately 250,000 annual ED visits.The Institutional Review Board and Medical Ethics Committee have approved this study. The requirement of written informed consents was waived because of the retrospective design of this study.
Inclusion criteria
Adult patients with the diagnosis of CAP admitted between January 2017 and May 2019 were screened.Demographic information of CAP patients, including vital signs on admission, radiological and laboratory parameters on ED arrival, was collected and recorded.Patients who fulfilled the following criteria were included: (1) age >18 years; (2) onset in the community;(3) new patchy infiltrates, lobar or segmental consolidation, ground-glass opacities or interstitial changes with or without pleural effusions; (4) new onset of cough or expectoration, or aggravation of existing symptoms of respiratory diseases, with or without purulent sputum, chest pain, dyspnea or hemoptysis or signs of pulmonary consolidation and/or moist rales or peripheral white blood cells (WBC) >10×109/L or<4×109/L with or without a left shift.[4]In accordance with Sepsis-3 criteria, we only enrolled CAP patients with increased SOFA score ≥2 from baseline.
Exclusion criteria
The following patients were excluded: (1) patients with acquired immuno-deficiency syndrome (AIDS),active tuberculosis or metastatic tumor; (2) patients finally diagnosed with pulmonary tumor, non-infectious interstitial lung disease, pulmonary edema, pulmonary embolism, or pulmonary vasculitis; (3) patients with pregnancy; (4) patients transferred from other hospitals,discharged from the hospital within ten days, or diagnosed with hospital-acquired pneumonia; (5) patients with incomplete clinical, laboratory or radiographic records;(6) patients with admission increased SOFA score <2 from baseline.
Parameter collection
Demographic characteristics of all enrolled patients on ED arrival were collected and recorded by trained triage nurses on admission. The past history,comorbidities, and vital signs (temperature, blood pressure, heart rate, breath rate, blood oxygen saturation,and state of consciousness) were also recorded.Laboratory parameters on admission including full blood count, hemoglobin (HGB) level, hematocrit(HCT), platelet (PLT) level, albumin (ALB), hepatic function (aspartate aminotransferase [AST], alanine aminotransferase [ALT], total bilirubin [TBIL], direct bilirubin [DBIL]), renal function (creatinine [CREA],blood urea nitrogen [BUN]), electrolytes, and arterial blood gas including lactate level were assessed and collected. The CURB65, PSI, SOFA, qSOFA, MEDS,and NEWS scores on admission for each patient were calculated according to international criteria and analyzed using data collected on ED arrival.
Primary outcome and secondary outcome
All enrolled patients were followed up for 28 days through medical records. According to their prognosis after 28-day admission, patients were divided into the death group and the survival group. The 28-day mortality was the primary outcome, while the secondary outcome included ICU admission and mechanical ventilation use.
Statistical analysis
All analyses were performed using SPSS 22.0 statistical software package (SPSS Inc., Chicago, IL,USA). Continuous variables with normal distribution were described as mean±standard deviation and compared using Student’st-test. Data with skewed distribution were expressed as median (interquartile range) and compared using Mann-WhitneyU-test. The discrete variables were described as percentages and compared using the Chi-squared test or Fisher’s exact test. Receiver operating characteristic (ROC) curves for each predictor were plotted, and the area under the curve (AUC) was determined to assess their predictive values. Models were also established using several logistic regressions to save the predicted probabilities.ROC curve analysis was performed using the saved probabilities as a new indicator. Comparisons of each predictor were conducted using MedCalc 15.0 Software(Acacialaan, Ostend, Belgium). AZ-test was used for comparing the AUCs between different curves. For comparison of the AUCs,was used, the test values beingZ0.05=1.96 andZ0.01=2.58.Based on the cut-off values, sensitivity, specificity,positive predictive value (PPV), and negative predictive value (NPV) were also calculated. Kaplan-Meier survival curves were drawn using cut-off values of qSOFA and NEWS. A two-tailed value ofP<0.05 was considered statistically signif icant.
RESULTS
A total of 582 patients were screened at recruitment,and 242 patients were excluded from our study cohort. A total of 340 eligible patients were finally enrolled in our study group. Of the 242 excluded patients, 62 patients were transferred from other hospitals, 58 patients discharged within ten days after admission, six patients f inally diagnosed with pulmonary tuberculosis, five patients with pulmonary thromboembolism, six patients with lung cancer, four patients with human immunodeficiency virus (HIV), three patients with pregnancy, 38 patients with incomplete medical records,40 patients with admission SOFA <2 from baseline, and 20 patients lost to follow-up with unknown prognosis (Figure 1).
Baseline characteristics
Of the 340 enrolled patients, 90 patients were dead after a 28-day follow-up, 62 patients were admitted to ICU, and 84 patients underwent mechanical ventilation(Table 1). There was no significant demographic difference between survivors and non-survivors,patients admitted to ICU and not admitted to ICU, patients with mechanical ventilation use and without mechanical ventilation use, although diabetes mellitius (DM) was more frequent in non-survivors and patients admitted to ICU(Table 1). The ALB levels were significantly lower, while the CREA and BUN levels were signif icantly higher among non-survivors, patients admitted to ICU, and patients with mechanical ventilation use. Moreover, the vital signs were more unstable among non-survivors, patients admitted to ICU and patients with mechanical ventilation use. In addition, the CURB65, PSI, SOFA, qSOFA, MEDS,NEWS, and lactate levels were significantly higher among non-survivors, patients admitted to ICU, and patients with mechanical ventilation use.
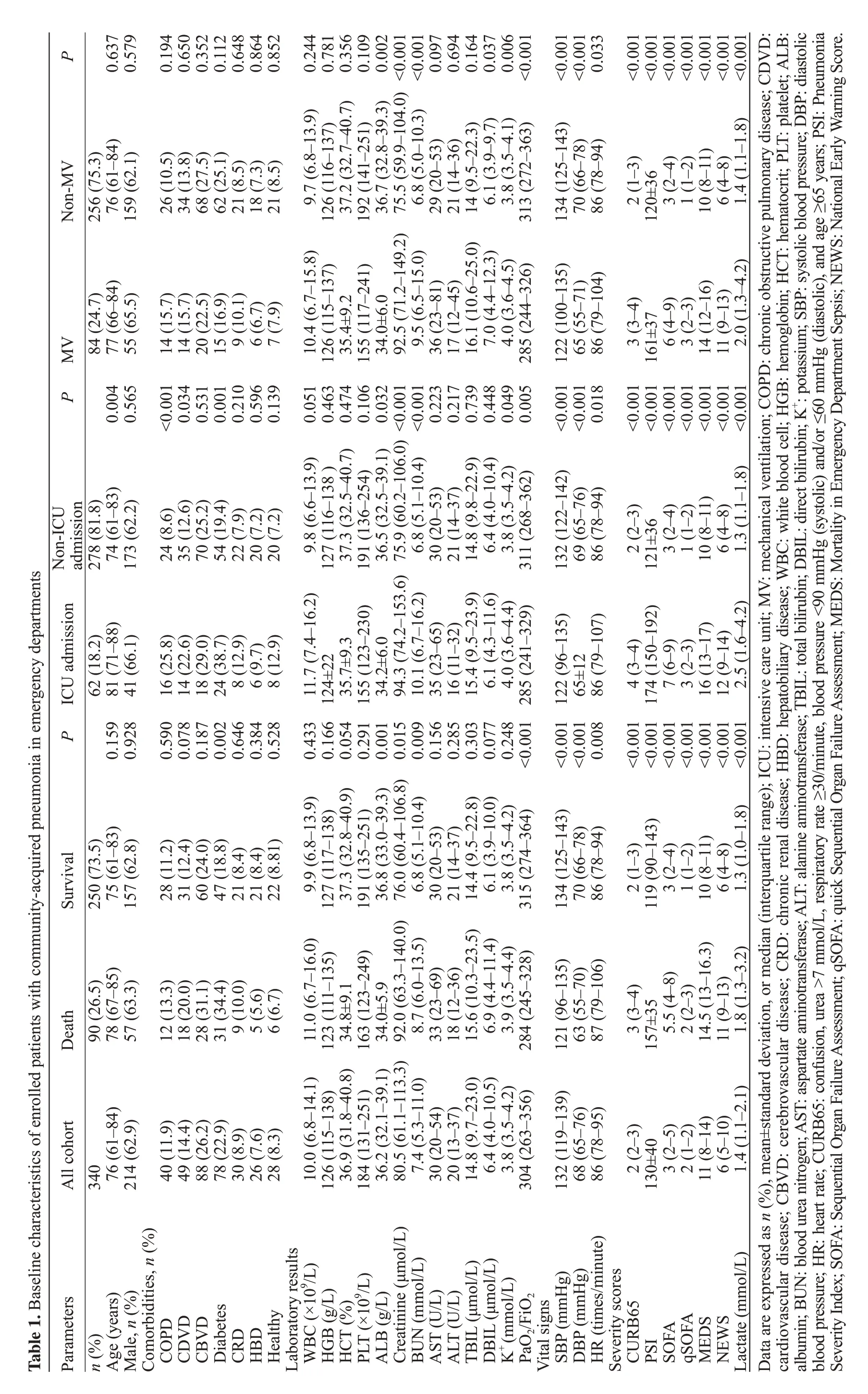
P 0.637 0.579 0.194 0.650 0.352 0.112 0.648 0.864 0.852 0.244 0.781 0.109<0.001 0.097 0.694 0.164 0.037 0.006<0.001<0.001<0.001 0.033<0.001<0.001<0.001<0.001<0.001<0.001<0.001 Non-MV 76 (61-84)256 (75.3)159 (62.1)26 (10.5)34 (13.8)68 (27.5)62 (25.1)21 (8.5)18 (7.3)21 (8.5)9.7 (6.8-13.9)37.2 (32.7-40.7) 0.356 126 (116-137)36.7 (32.8-39.3) 0.002 192 (141-251)6.8 (5.0-10.3)29 (20-53)21 (14-36)6.1 (3.9-9.7)3.8 (3.5-4.1)313 (272-363)134 (125-143)70 (66-78)86 (78-94)2 (1-3)3 (2-4)1 (1-2)10 (8-11)6 (4-8)84 (24.7)0.004 77 (66-84)MV 0.565 55 (65.5)<0.001 14 (15.7)1.4 (1.1-1.8)120±36 P 0.034 14 (15.7)0.531 20 (22.5)0.001 15 (16.9)0.210 9 (10.1)0.596 6 (6.7)0.139 7 (7.9)0.051 10.4 (6.7-15.8)0.463 126 (115-137)0.106 155 (117-241)<0.001 9.5 (6.5-15.0)0.223 36 (23-81)0.448 7.0 (4.4-12.3)0.049 4.0 (3.6-4.5)0.005 285 (244-326)<0.001 122 (100-135)0.018 86 (79-104)<0.001 65 (55-71)<0.001 3 (3-4)<0.001 161±37<0.001 6 (4-9)<0.001 3 (2-3)<0.001 11 (9-13)74 (61-83)278 (81.8)ICU admission Non-ICU admission 0.217 17 (12-45)<0.001 14 (12-16)24 (8.6)0.739 16.1 (10.6-25.0) 14 (9.5-22.3)70 (25.2)173 (62.2)35 (12.6)54 (19.4)22 (7.9)20 (7.2)20 (7.2)0.433 11.7 (7.4-16.2) 9.8 (6.6-13.9)<0.001 2.0 (1.3-4.2)127 (116-138 )37.3 (32.5-40.7) 0.474 35.4±9.2 2 (2-3)36.5 (32.5-39.1) 0.032 34.0±6.0 191 (136-254)0.009 10.1 (6.7-16.2) 6.8 (5.1-10.4)3 (2-4)30 (20-53)21 (14-37)311 (268-362)1 (1-2)132 (122-142)69 (65-76)6 (4-8)86 (78-94)121±36 Table 1. Baseline characteristics of enrolled patients with community-acquired pneumonia in emergency departments 0.077 6.1 (4.3-11.6) 6.4 (4.0-10.4)10 (8-11)3.8 (3.5-4.2)P 0.159 81 (71-88)62 (18.2)0.590 16 (25.8)0.928 41 (66.1)0.078 14 (22.6)0.187 18 (29.0)0.002 24 (38.7)0.646 8 (12.9)1.3 (1.1-1.8)0.384 6 (9.7)0.528 8 (12.9)0.166 124±22 0.291 155 (123-230)0.156 35 (23-65)37.3 (32.8-40.9) 0.054 35.7±9.3 0.248 4.0 (3.6-4.4)36.8 (33.0-39.3) 0.001 34.2±6.0<0.001 285 (241-329)0.285 16 (11-32)0.303 15.4 (9.5-23.9) 14.8 (9.8-22.9)<0.001 122 (96-135)0.008 86 (79-107)<0.001 65±12<0.001 4 (3-4)<0.001 7 (6-9)<0.001 174 (150-192)<0.001 3 (2-3)<0.001 2.5 (1.6-4.2)<0.001 16 (13-17)<0.001 12 (9-14)Survival 75 (61-83)250 (73.5)157 (62.8)28 (11.2)31 (12.4)60 (24.0)47 (18.8)21 (8.4)21 (8.4)22 (8.81)9.9 (6.8-13.9)127 (117-138)191 (135-251)6.8 (5.1-10.4)30 (20-53)21 (14-37)6.1 (3.9-10.0)3.8 (3.5-4.2)315 (274-364)134 (125-143)70 (66-78)86 (78-94)2 (1-3)3 (2-4)1 (1-2)6 (4-8)57 (63.3)10 (8-11)90 (26.5)1.3 (1.0-1.8)78 (67-85)12 (13.3)Death 18 (20.0)28 (31.1)31 (34.4)119 (90-143)9 (10.0)5 (5.6)6 (6.7)11.0 (6.7-16.0)123 (111-135)163 (123-249)36.9 (31.8-40.8) 34.8±9.1 8.7 (6.0-13.5)36.2 (32.1-39.1) 34.0±5.9 33 (23-69)6.9 (4.4-11.4)18 (12-36)3.9 (3.5-4.4)15.6 (10.3-23.5) 14.4 (9.5-22.8)284 (245-328)121 (96-135)63 (55-70)3 (3-4)87 (79-106)5.5 (4-8)2 (2-3)1.8 (1.3-3.2)157±35 11 (9-13)14.5 (13-16.3)All cohort 76 (61-84)340 214 (62.9)40 (11.9)49 (14.4)88 (26.2)78 (22.9)30 (8.9)26 (7.6)28 (8.3)10.0 (6.8-14.1)126 (115-138)184 (131-251)80.5 (61.1-113.3) 92.0 (63.3-140.0) 76.0 (60.4-106.8) 0.015 94.3 (74.2-153.6) 75.9 (60.2-106.0)<0.001 92.5 (71.2-149.2) 75.5 (59.9-104.0)<0.001 7.4 (5.3-11.0)30 (20-54)20 (13-37)14.8 (9.7-23.0)6.4 (4.0-10.5)3.8 (3.5-4.2)304 (263-356)132 (119-139)68 (65-76)86 (78-95)2 (2-3)3 (2-5)130±40 2 (1-2)6 (5-10)11 (8-14)1.4 (1.1-2.1)Parameters n (%)Age (years)Male, n (%)Comorbidities, n (%) COPD CDVD CBVD Diabetes CRD HBD Healthy Laboratory results WBC (×109/L)HGB (g/L)HCT (%)PLT (×109/L)Creatinine (μmol/L)ALB (g/L)BUN (mmol/L)AST (U/L)TBIL (μmol/L)ALT (U/L)DBIL (μmol/L)K+ (mmol/L)PaO2/FiO2 DBP (mmHg)Vital signs SBP (mmHg)HR (times/minute)Severity scores CURB65 PSI SOFA qSOFA MEDS NEWS Lactate (mmol/L)Data are expressed as n (%), mean±standard deviation, or median (interquartile range); ICU: intensive care unit; MV: mechanical ventilation; COPD: chronic obstructive pulmonary disease; CDVD:cardiovascular disease; CBVD: cerebrovascular disease; CRD: chronic renal disease; HBD: hepatobiliary disease; WBC: white blood cell; HGB: hemoglobin; HCT: hematocrit; PLT: platelet; ALB:albumin; BUN: blood urea nitrogen; AST: aspartate aminotransferase; ALT: alanine aminotransferase; TBIL: total bilirubin; DBIL: direct bilirubin; K+: potassium; SBP: systolic blood pressure; DBP: diastolic blood pressure; HR: heart rate; CURB65: confusion, urea >7 mmol/L, respiratory rate ≥30/minute, blood pressure <90 mmHg (systolic) and/or ≤60 mmHg (diastolic), and age ≥65 years; PSI: Pneumonia Severity Index; SOFA: Sequential Organ Failure Assessment; qSOFA: quick Sequential Organ Failure Assessment; MEDS: Mortality in Emergency Department Sepsis; NEWS: National Early Warning Score.
Prediction of the 28-day mortality
In predicting the 28-day mortality, NEWS showed the largest area under the receiver operating characteristic(AUROC) curve (0.861) among single predictors, followed by MEDS (0.834), SOFA (0.796), qSOFA (0.791), PSI(0.771), CURB65 (0.748), and lactate (0.683) (Figure 2A).The cut-off values for qSOFA and NEWS were 2 and 9,respectively. Among single predictors, NEWS outperformed other predictors (allP<0.05) except MEDS (Z=1.140,P=0.255).
Among the combinations of severity scores and lactate,the combination of NEWS+lactate achieved the highest AUROC (0.866), followed by MEDS+lactate (0.843),qSOFA+lactate (0.821), SOFA+lactate (0.802), PSI+lactate(0.775), and CURB65+lactate (0.773) (Figure 2B). Pairwise comparisons revealed similar predicting performance between NEWS+lactate and MEDS+lactate (Z=1.000,P=0.317), while NEWS+lactate outperformed SOFA+lactate(Z=2.478,P=0.013), qSOFA+lactate (Z=1.996,P=0.046),PSI+lactate (Z=3.601,P=0.003), and CURB65+lactate(Z=4.242,P<0.001). Lactate significantly improved the AUROC of CURB65 (0.748 vs. 0.777,P=0.022) and qSOFA(0.791 vs. 0.823,P=0.026), while lactate did not improve the AUROC of NEWS (0.861 vs. 0.866,P=0.468) (Figure 2C),MEDS (0.834 vs. 0.844,P=0.201), SOFA (0.796 vs. 0.805,P=0.267), or PSI (0.771 vs. 0.778,P=0.251).
Prediction of ICU admission
In predicting ICU admission, NEWS demonstrated the highest AUROC (0.895) among single predictors,followed by SOFA (0.892), MEDS (0.876), PSI (0.838),qSOFA (0.805), CURB65 (0.779) and lactate (0.747)(Figure 3A). The cut-off values for qSOFA and NEWS were 2 and 9, respectively. Among single predictors,NEWS outperformed qSOFA (P=0.004), PSI (P=0.043),and CURB65 (P=0.001).
Among the combinations of severity scores and lactate, the combination of NEWS+lactate achieved the largest AUROC (0.905), followed by SOFA+lactate(0.901), MEDS+lactate (0.895), qSOFA+lactate(0.860), PSI+lactate (0.843), CURB65+lactate(0.822) (Figure 3B). Pairwise comparisons revealed no significant difference between NEWS+lactate and MEDS+lactate (Z=0.555,P=0.579), NEWS+lactate and SOFA+lactate (Z=0.196,P=0.845), while significant difference was found between NEWS+lactate and qSOFA+lactate (Z=2.354,P=0.019), NEWS+lactate and PSI+lactate (Z=2.503,P=0.012), NEWS+lactate and CURB65+lactate (Z=3.632,P=0.003). Lactate signif icantly improved the AUROC of qSOFA (0.805 vs.0.860,P=0.02) and CURB65 (0.779 vs. 0.822,P=0.017),while lactate did not improve the AUROC of NEWS(0.895 vs. 0.905,P=0.152) (Figure 3C), MEDS (0.876 vs. 0.895,P=0.069), SOFA (0.892 vs. 0.901,P=0.179),or PSI (0.838 vs. 0.843,P=0.592).
Prediction of mechanical ventilation use
In terms of prediction of mechanical ventilation use,NEWS (0.873) also achieved the highest AUROC among single predictors, followed by SOFA (0.845), MEDS(0.833), qSOFA (0.821), PSI (0.782), CURB65 (0.775),and lactate (0.703) (Figure 4A). The cut-off values for qSOFA and NEWS were 2 and 9, respectively. Among single predictors, NEWS showed the similar predicting performance to MEDS (Z=1.707,P=0.088) and SOFA(Z=1.110,P=0.267), and NEWS outperformed CURB65(Z=3.932,P<0.001), PSI (Z=3.269,P=0.001), and qSOFA (Z=2.150,P=0.032).
Among the combinations of severity scores and lactate, the combination of NEWS+lactate achieved the highest AUROC (0.886), followed by qSOFA+lactate(0.859), MEDS+lactate (0.858), SOFA+lactate (0.852),CURB65+lactate (0.808), and PSI+lactate (0.799)(Figure 4B). Pairwise comparisons demonstrated no significant difference between NEWS+lactate and MEDS+lactate (Z=0.314,P=0.754), NEWS+lactate and SOFA+lactate (Z=1.909,P=0.056), NEWS+lactate and qSOFA+lactate (Z=1.631,P=0.103), NEWS+lactate and PSI+lactate (Z=1.063,P=0.288), or NEWS+lactate and CURB65+lactate (Z=0.342,P=0.732).
Prediction of primary and secondary outcomes
Our study revealed that in predicting both primary and secondary outcomes, the optimal cut-off values for qSOFA and NEWS were 2 and 9, respectively. Using these cut-off values, significant differences were found between the qSOFA ≥2 group and qSOFA <2 group,or between the NEWS ≥9 group and NEWS <9 group(Table 2). In multivariate Cox regression analysis,MEDS (adjusted hazard ratio [aHR]=1.199), NEWS(aHR=1.227), and HCT (aHR=0.974) were independent prognostic factors for survival (Table 3). Kaplan-Meier survival curves were plotted and compared using optimal cut-off values of qSOFA and NEWS (Figure 5). Results indicated that the two groups with qSOFA ≥2 and qSOFA<2 (log-rankχ2=51.404,P=0.000), or the two groups with NEWS ≥9 and NEWS <9 (log-rankχ2=130.207,P=0.000) differed significantly. Patients with admission qSOFA <2 or with NEWS <9 had a significantly prolonged survival time compared with patients with admission qSOFA ≥2 or with NEWS ≥9.
DISCUSSION
CAP is a main cause of sepsis and sepsis-related death.[1]Severe CAP, a main cause of unexpected ICU transfer within 24 hours of ward arrival from the ED, is associated with a high risk of respiratory failure or sepsisrelated organ dysfunction.[16]Patients with delayed ICU transfer usually showed poor outcomes, indicating the importance of early severity recognition and outcome prediction. Severity assessment and outcome prediction are recognized as pivotal steps in the management of CAP. The effective use of assessment tools necessitates the risk stratification of CAP patients. Multiple scoring systems have been developed to quantify disease severity in critically ill CAP patients.

Figure 2. ROC curve in predicting the 28-day mortality. A: comparisons of CURB65, PSI, SOFA, qSOFA, MEDS, NEWS, and admission lactate;B: comparisons of different combinations of CAP severity scores and admission lactate; C: comparisons of NEWS, lactate, and NEWS+lactate.

Figure 3. ROC curve in predicting ICU admission. A: comparisons of CURB65, PSI, SOFA, qSOFA, MEDS, NEWS, and admission lactate; B:comparisons of different combinations of CAP severity scores and admission lactate; C: comparisons of NEWS, lactate, and NEWS+lactate.

Figure 4. ROC curve in predicting mechanical ventilation. A: comparisons of CURB65, PSI, SOFA, qSOFA, MEDS, NEWS, and admission lactate; B: comparisons of different combinations of CAP severity scores and admission lactate; C: comparisons of NEWS, lactate, and NEWS+lactate.
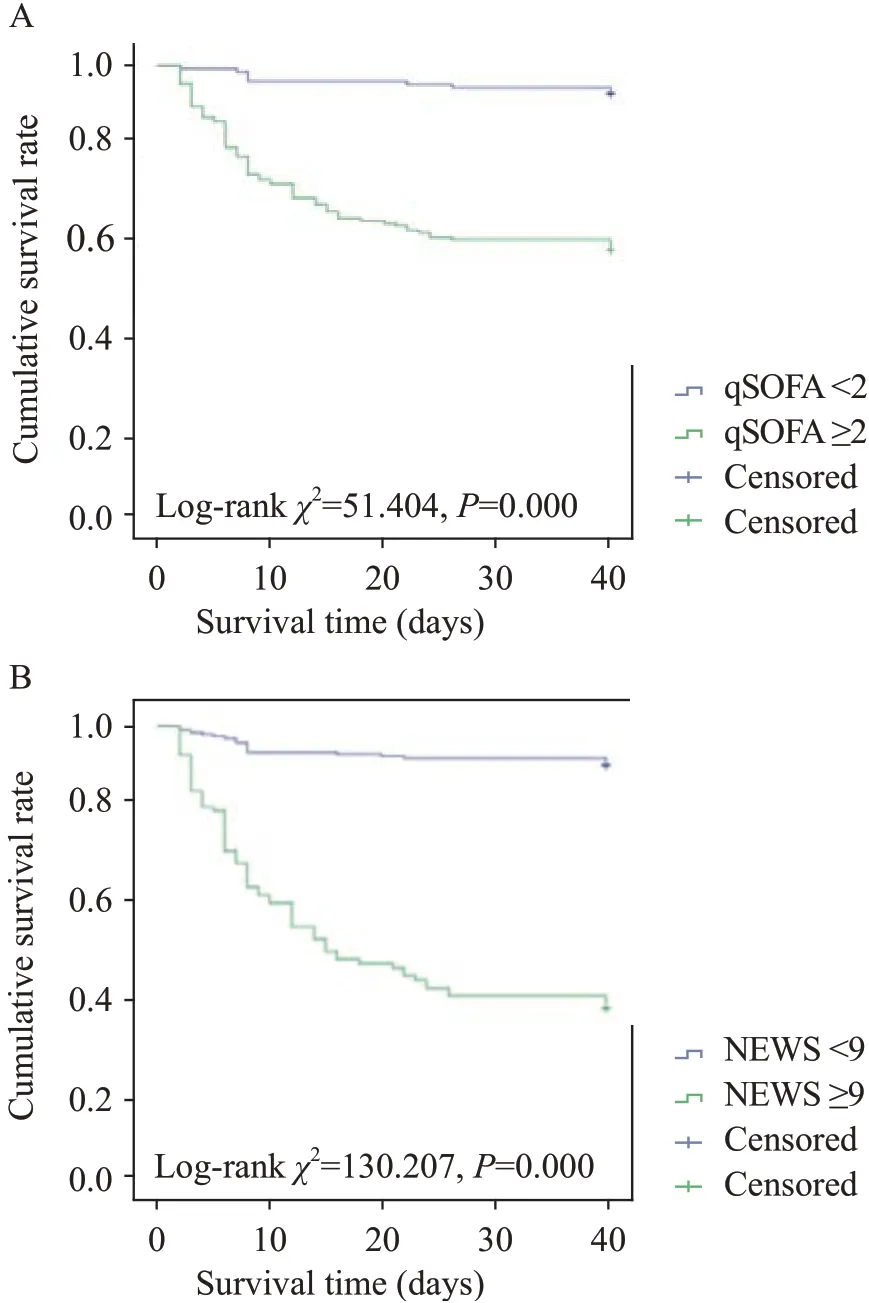
Figure 5. Kaplan-Meier survival curve. A: comparison between CAP patients with qSOFA <2 and CAP patients with qSOFA ≥2; B: comparison between CAP patients with NEWS <9 and CAP patients with NEWS ≥9.
Current guidelines recommended clinical risk assessment of CAP by validated severity scores like the CURB65 and PSI.[1,4,5]The PSI was introduced in 1997 following a study in over 50,000 patients and was proved to be a robust severity assessment tool.[6]The CURB65 score was reported in 2003, and one of its advantages is its simplicity compared with PSI which is comprised of 20 parameters.[17]CURB65 showed very good accuracy for predicting the 30-day mortality among CAP patients discharged from the ED.[18]In addition, patients with CURB65 score≤2 were often admitted to the ICU and received critical care interventions. Given this finding and the relatively low sensitivity of CURB65 for critical care intervention, clinicians should exercise caution when using CURB65 to guide disposition.[19]Comparatively, the CURB65 and PSI predicted similarly in mortality in CAP.[20]What’s more, CURB65 is more valid for the lower scores,while PSI is more valid for the higher scores.[21]Nonetheless,another research reported that PSI was more sensitive than CURB65 for mortality prediction across all age groups.[22]
In 2016, the Sepsis-3 Task Force updated the previous definition of sepsis and redefined it as a lifethreatening organ dysfunction caused by a dysregulated host response to infection.[7]Organ dysfunction was defined as an increase in the SOFA score of 2 or more. A new screening system termed as qSOFA was recommended for screening patients with high risk of mortality.[7]A qSOFA >2, despite poor sensitivity,was reported to be strongly associated with mortality in patients with pneumonia.[23]A study by Asai et al[24]reported that for the 30-day mortality, the AUROC forthe SOFA score was 0.769, while the AUROC for SOFA score with a qSOFA ≥2 was 0.829 for CAP patients. The PROGRESS study enrolled 1,532 CAP patients, and results proved that in predicting death or need for ICU admission,SOFA (AUROC 0.948) significantly outperformed CURB65, PSI, and qSOFA.[25]Another research in which 1,545 cases were enrolled demonstrated that overall accuracy assessed by ROC was more superior for CURB65 than for qSOFA, a qSOFA ≥2 at admission identif ied 40.3%of those who died within 30 days, and thus advised use of pneumonia-specific tools rather than generic sepsis or early warning scores.[15]Song et al[26]enrolled 443 CAP patients, and results indicated that qSOFA with lactate was a useful and practical tool for the early identif ication of in-hospital mortality among CAP patients in ED.

Table 2. Comparisons of severity scores and different outcomes in patients with CAP using qSOFA and NEWS

Table 3. Variables in the equation after Cox regression analysis
MEDS score was developed in 2003 and incorporated nine parameters readily available in EDs to aid clinicians in the accurate assessment of patients’severity and mortality risks at ED presentation with suspected infection.[27]The MEDS score is reported to be an excellent predictor of short-term outcomes in patients with community-onset bacteremia with higher calibration and discrimination.[28]When combined with procalcitonin, MEDS performed well in predicting mortality of ED admitted patients with inf luenza.[29]The NEWS, derived in the United Kingdom in 2012 by the NEWS Development and Implementation Group on behalf of the Royal College of Physicians, consisted of six physiological parameters classifying patients into three risk categories.[30]A study by Sbiti-Rohr et al[11]demonstrated that for the 30-day mortality, NEWS was inferior compared to PSI and CURB65 with an AUROC of 0.65, while NEWS was superior to PSI and CURB65 for prediction of ICU admission and empyema. A study by Brabrand et al[31]showed no statistical difference between CURB65 and NEWS at identifying CAP patients at risk of the 30-day mortality. When modified by serum lactate level, the National Early Warning Score-Lactate score was comparable to PSI and CURB65 for inpatient mortality prediction among adult CAP patients.[32]
The serum lactate is a well-known predictor of mortality in patients with sepsis, organ failure, and shock.[26]Hyperlactatemia upon admission is an early biomarker of organ failure and hypoperfusion. A lactate level >2 mmol/L, with a requirement for vasopressors to maintain a mean arterial blood pressure of 65 mmHg,was suggested in the new def inition of septic shock.[7,26]Obtaining blood for measuring lactate is recommended by Surviving Sepsis Campaign Bundle update, and if lactate >2 mmol/L, it should be re-measured within 2-4 hours to guide resuscitation.[33]Admission lactate levels significantly improved the prognostic value (need for mechanical ventilation, vasopressors, ICU admission,or hospital mortality) of CRB/CURB65 scores in CAP patients with an optimal cut-off value of 1.8 mmol/L.[34]The initial lactate level was independently associated with mortality in hospitalized patients with CAP.[35]
In this research, we studied the outcome prediction value of CURB65, PSI, SOFA, qSOFA, MEDS, NEWS,and admission lactate level simultaneously. Our study is among the very few studies that explore these severity scores and admission levels at the same time.We found that NEWS achieved the highest AUROC in predicting the 28-day mortality, ICU admission, and use of mechanical ventilation, while NEWS and MEDS showed similar predicting performance among single predictors. The mortality rate of CAP patients in our study was higher, and NEWS in our study achieved a higher AUROC than previous studies.[11,12]These could be explained by the fact that we only enrolled septic CAP patients in ED with SOFA score at admission ≥2 from baseline. Among the combinations of severity scores and admission lactate, NEWS+lactate had the highest AUROC, demonstrating its superiority in predicting the 28-day mortality and ICU admission,though no difference was found in multiple pairwise comparisons in predicting use of mechanical ventilation.NEWS+lactate and MEDS+lactate had similar performance in predicting both primary and secondary outcomes. Moreover, both NEWS and MEDS entered the equation after Cox regression analysis. These results highlighted the predicting performance of NEWS and MEDS. Regrettably, lactate only improved the predicting performance of CURB65 and qSOFA in predicting the 28-day mortality and ICU admission, which were similar to a previous study.[16]In addition, lactate did not improve the predicting performance of any severity scores in predicting mechanical ventilation. Our research also demonstrated that based on the cut-off values, a qSOFA≥2 and a NEWS ≥9 were strongly associated with both primary and secondary outcomes, which could remind physicians to exercise caution when treating these CAP patients. Comparatively, another research by Abbott et al[13]reported that a NEWS of 3 or more was associated with death within two days of admission. More further in-depth studies are needed to explore these differences.Components of all other scores (CURB65, PSI, SOFA,and MEDS) consist of laboratory elements, which makes them very inconvenient to use in routine clinical practice in crowded emergency rooms. Comparatively,NEWS and qSOFA include only indicators of vital signs,which could be easily obtained at ED admission. That NEWS performed better than qSOFA, should also be expected as NEWS comprised of additional parameters known to be valuable in identifying high-risk patients.[36]This highlighted the advantage of the clinical utilization of NEWS. In addition, NEWS allocates 0-3 points to each of several clinical parameters, while other severity scores consist of similar physiological variables with different weighting thresholds. We hypothesized that this may explain why NEWS outperformed other severity scores in predicting outcomes of septic CAP patients in ED. Considering that both NEWS and qSOFA are very convenient to use at ED admission without requiring laboratory components, it makes sense that physicians in ED could benef it in utilizing these two predictors.
Limitations
Several limitations of our study need to be addressed.Firstly, the relatively small sample size and the singlecenter design may limit the generalisability of our results for external validity. Baseline characteristics of CAP patients may differ by region and country, which could result in different statistical results compared with our study.Secondly, we only enrolled septic patients with CAP in the ED, their ages were older, and this could inf luence our f inal results. Our results should be verif ied by more multi-center and a large-cohort studies.
CONCLUSIONS
We explored the outcome prediction values of CURB65,PSI, SOFA, qSOFA, MEDS, NEWS, and admission lactate level for septic patients with CAP in EDs. We found that NEWS showed superiority over other severity scores and admission lactate in predicting the 28-day mortality, ICU admission, and mechanical ventilation use, while MEDS had similar predicting performance among single predictors.NEWS+lactate and MEDS+lactate had similar predicting performance, and they outperformed other combinations of severity score and admission lactate in predicting the 28-day mortality. NEWS+lactate, MEDS+lactate, and SOFA+lactate had similar predicting performance and they outperformed other combinations in predicting ICU admission. NEWS+lactate did not show superiority over other combinations in predicting mechanical ventilation use. Admission lactate did not well predict the outcomes or improve the severity scores of CAP. More multi-center studies with large sample size are warranted to validate our study results.
Funding:This study was supported by Capital Clinical Characteristic Application Research of Beijing Municipal Science& Technology Commission (Z171100001017057).
Ethical approval:This study was approved by the Institutional Review Board and Medical Ethics Committee of Beijing Chaoyang Hospital, Capital Medical University (2019-301).
Conf licts of interest:There is no conf lict of interest in this study.
Contributors:All authors have substantial contributions to the acquisition, analysis, or interpretation of data for the work. HJZ and SBG conceived and designed this research. HJZ and TFL collected data and performed the statistical analysis. HJZ drafted the manuscript. HJZ and SBG reviewed and revised the manuscript critically. All authors read and approved the final version of the submitted manuscript.
杂志排行
World journal of emergency medicine的其它文章
- Improving antibiotic prescribing in the emergency department for uncomplicated community-acquired pneumonia
- Effects of f luid balance on prognosis of acute respiratory distress syndrome patients secondary to sepsis
- Effects of sepsis on hippocampal volume and memory function
- Death and do-not-resuscitate order in the emergency department: A single-center three-year retrospective study in the Chinese mainland
- The general public’s ability to operate automated external def ibrillator: A controlled simulation study
- Aldehyde dehydrogenase 2 preserves mitochondrial morphology and attenuates hypoxia/reoxygenationinduced cardiomyocyte injury
