Experimental model standardizing polyvinyl alcohol hydrogel to simulate endoscopic ultrasound and endoscopic ultrasound-elastography
2020-10-09ElymirGalvisGarciaSergioSobrinoCossioArturoRedingBernalYesicaContrerasMarinKarinaSolorzanoAcevedoPatriciaGonzalezZavalaRosaQuispeSiccha
Elymir S Galvis-Garcia, Sergio Sobrino-Cossio, Arturo Reding-Bernal, Yesica Contreras-Marin, Karina Solorzano-Acevedo, Patricia Gonzalez -Zavala, Rosa M Quispe-Siccha
Abstract
Key Words: Endoscopic ultrasound simulators in endoscopy; Polyvinyl alcohol; Endoscopic ultrasound; Endoscopic ultrasound elastography; Strain; Elasticity
INTRODUCTION
According to the American Society for Gastrointestinal Endoscopy, before trainees can be certified in advanced endoscopic techniques, they must perform a minimum number of procedures to achieve competence[1]. Simulators may reduce the learning curve[1]; however, current models do not recreate reality, require considerable investment in terms of time and resources, and do not necessarily reproduce the haptic[2,3]. Biomaterials, compatible with human tissues make it possible to simulate lesions[4]. Natural (collagen, chitosan, fibrin,etc.) or synthetic hydrogels [polyethylene oxide, polyacrylic acid, polyvinyl pyrrolidone and polyvinyl alcohol (PVA)], absorb liquid without dissolving, due to their permeability and low friction coefficient[5,6]. Manipulation of the molecular weight (MW) and concentration of the PVA hydrogel results in contrasting densities (viscoelasticity), in order to simulate models more realistically[7-9]. These phantoms are compatible with magnetic resonance imaging and ultrasonography; which can produce acoustic, optical and elastographic images[10]. Elastography measures the degree of tissue stiffness illustrated in digital color distribution by means of the deformation histogram (DH) and strain ratio (SR). The classification system for EUS-elastography (EUS-E) is based on color patterns that measure the degree of tissue stiffness. EUS-E refers to the region of interest: A which comprises the tumor area and B the soft surface quotient; B/A strain ratio (SR) represents the elastographic measurement of interest[11-13]. Leeet al[14]reported the DH effectiveness for diagnosing solid masses is 97.7%. The sensitivity (SR > 6.04 or elasticity < 0.05%) and specificity (SR > 15.41 or elasticity < 0.03%) of the SR is close to 100%. However, these results were not confirmed with the same high figures in subsequent studies[15-17].
Although results are not consistent, knowledge of elasticity coefficient of digestive organs and lesions (cystic, semi-solid and solid) makes it possible to create more realistic models, due to the viscoelastic properties of PVA hydrogels. It is thus important to assess the modulus of elasticity or Young's modulus (E = stress/strain; KPa) of phantoms in order to construct them and compare them with tissues[18]. This work was designed to standardize the mechanical properties of PVA phantoms, employing endoscopic ultrasound images for the simulation of organs and digestive lesions and elastography to evaluate the degree of tissue stiffness.
MATERIALS AND METHODS
This experimental study was performed in the Unidad de Investigación y Desarrollo Tecnológico (its acronym in Spanish is Unidad de Investigación y Desarrollo Tecnológico) of Hospital General de México “Dr. Eduardo Liceaga”, Mexico City. PVA hydrogels (phantoms) with different densities (by changing molecular weight and concentration) were prepared. The study was exempt from approval by the Ethics Committee as there are no live specimens involved (human or animal tissue). Two molecular weights were used: MW1= 85000-124000 and MW2= 146000-186000 and a range of PVA concentrations: 3%, 5%, 7%, 9%, 12%, 15% and 20% (Sigma-Aldrich) with a 99.9% degree of hydrolysis.
Preparation of PVA phantoms
We used the following equation to obtain the desired concentrations of PVA phantoms (3%, 5%, 7%, 9%, 12%, 15% and 20%) for the two molecular weights, and to calculate the weight of PVA powder in 100 mL of Milli-Q ultrapure H2O (Merck). The PVA powder crystals were dissolved after heating the mixture to 90°C, while stirring continuously (magnetic bar) until a more homogeneous hydrogel was obtained. The hydrogel was cooled for 25 min at room temperature (25°C) and stored in stainless steel boxes (containers) to avoid contamination and ensure accuracy in terms of dimensions, as presented in Figure 1. The containers were subjected to four freezing cycles (-80°C/1.5 h; Freezer-Kaltis) and defrosting (25°C/4 h), until the phantoms showed stable mechanical properties. They were then submerged in ultrapure water for preservation (where they can last for years).
Density and Young’s modulus
The density (g/cm3) and Young's modulus (elasticity module, KPa) for each phantom (E = stress/strain) were calculated after trimming the films (1 cm × 1 cm × 0.2 cm) from the PVA phantoms.
Endoscopic ultrasound images
Images were obtained (Olympus GF-UM160 and Pentax Medical EUS 360º EG-3670URK), after submerging the phantom (Milli-Q ultrapure water at 25°C) and pressing one of its walls with a latex balloon, placed on the tip of the echoendoscope, as presented in Figure 2.
The frequency used was 7.5 MHz. Images were contrasted to those of healthy organs (pancreas and liver) and pancreatic lesions (cysts and solid masses).
Endoscopic ultrasound elastography images
We evaluated phantoms in terms of stiffness/elasticity (Pentax EUS-Hitachi EUB900, Real-Time Tissue Elastography) with 2-panel images inBmode of conventional grayscale (right) and elastographic image (left). The frequency used was 7.5 MHz (5.0 to 10.0 MHz)[11]. The point of interest (A or B) was measured to determine the degree of normal deformity (SR) < 6.04 and the degree of normal elasticity (B/A ratio) > 0.05%. The “A” area comprises the largest area of the tumor and the “B” area the soft surface (red). The B/A ratio (strain ratio) was considered to represent an elastographic evaluation[12].

Figure 1 Stainless steel mold used to obtain polyvinyl alcohol phantoms.

Figure 2 Endoscopic ultrasound images with the echoendoscope placed inside the polyvinyl alcohol phantom.
Observers
Observer 1 had > 12 years of experience in EUS diagnosis, with formal training in Denmark and Venezuela, and was in charge of the area in the HGM; Observer 2 had > 8 years of experience in EUS diagnosis, with formal training in Mexico and the United States.
Statistical analysis
We calculated the inter-observer agreement (kappa index, intra-class correlation coefficient, and extent of agreement) between the two EUS experts. To compare their congruence, we conducted an independent and blind test of simulated/real images. Kappa values and degree of concordance were as follows: < 0.2 = Poor, 0.21-0.40 = Weak, 0.41-0.60 = Moderate, 0.61-0.80 = Good, and 0.81-1.00 = Very good.
A satisfaction survey was applied, consisting of nine questions regarding the simulated image (Likert-4 points: 0 = Not satisfied, 1 = Little satisfied, 2 = Quite satisfied and 3 = Very satisfied): (1) Normal pancreas; (2) Normal liver; (3) Homogeneous lesions; (4) Heterogeneous lesions; (5) Solid lesions; (6) Cystic lesions; (7) Semi-solid lesions; (8) Elastographic image contrast; and (9) Feasibility of measuring the degree of elasticity. For the analysis, the measurement was binary (22 table): Yes = Very satisfied/satisfiedvsNo = Moderately satisfied/not satisfied, and 20 images were evaluated. The correlation between density and degree of elasticity of tissues was calculated.
RESULTS
The density and Young’s modulus (M.Y.) of each PVA-phantom are summarized in Table 1. The stiffness of the phantom was correlated with higher MW and concentration (correlationr= 0.8,P= 0.01) and with the increase in density and M.Y. This depended on cross-linking the monomers by freeze/thaw cycles. Simulated lesions were visible using EUS. As shown in Figure 3, endoscopic ultrasound revealed differences between phantoms: C1vsC5(MW1= 85000-124000).
Density was higher in homogeneous lesions (MW2= 146000–186000: C9= 15% and C10= 20%), (Figure 4) than in heterogeneous lesions (MW1= 85000–124000: C1= 7% and C2= 9%) (Figure 5). Concordance was 0.8 with a high degree of satisfaction.
Cystic lesions were created with higher density phantoms: C6and C10(MW2= 146000–186000) (Figure 6). These cystic lesions were measured by EUS (E-EUS was never used for this). Concordance was 0.8 (kappa), with a high degree of satisfaction (Likert scale 4-points). Solid lesions were contrasted with soft areas (Figure 7). The color contrasts, RI: A and B, and SR: B/A of elastographic images are presented in Figure 8. We observed lower elasticity (dark blue area), in the case of a simulated solid lesion that contrasted with green areas (normal). SR values of > 6.04 or elasticity of < 0.05% corresponded to areas with less elasticity (rigid). The differences between the B/A ratios (65.6vs7.13) and point A (0.02vs0.07%) translated into greater tissue stiffness. Figure 9 and Table 2 show the relationship between points of interest and strain ratios with different PVA phantom densities.
DISCUSSION
Simulation by EUS/EUS-E of visible organs and lesions is feasible using PVA phantoms. The model had high inter-observer concordance and satisfaction. This simulation facilitates practice, while curtailing risk. The increase in the number of repetitions amplifies skills and reduces the learning curve[2,3]. However, the models lack the realism necessary to achieve competence[2]. The focus of our experiment was to build lesions and organs visible by EUS and EUS-E, but we did not evaluate whether the technique was the most appropriate tool for differentiating malignant lesions from normal tissue. We were able to create realistic ultrasonic images using PVA phantoms. However, knowledge of the elastographic parameters of different tissues allowed us to create simulated lesions due to the viscoelastic properties of the PVA hydrogel and to contrast these with normal structures. EUS-E enables a comparison between the target and normal tissue but a stiff lesion can be either benign or malignant; therefore, the elastic properties of a tumor area may be different to those in another area[15]. Currently, the effectiveness of the DH for diagnosing solid masses is a matter of debate and outcomes are controversial. However, the rationale for using EUS–E in chronic pancreatitis relates to the possibility of detecting the increased degree of fibrosis in diseased pancreas, compared to normal pancreas[19]. Despite the controversy, we selected the B/A ratio (strain ratio) to measure tissue stiffness[12]as well as the region of interest. A and B were marked in different colors (on a scale of 0-255)[19]. It is difficult to place the region of interest of the target at the same level; this is associated with low specificity and reproducibility, and great variability in cutoff for inflammatory pancreatic masses and pancreatic cancer[15]. In contrast, if the lesion appears soft, EUSE can rule out malignancy with a high level of certainty. However two negative fine needle aspirations (FNAs), using EUS, in the case of a soft and enhancing lesion can rule out the diagnosis of pancreatic adenocarcinoma in 95% of patients[15]. The accuracy of strain ratio to distinguish between normal pancreas and pancreatitis is greater, but depends on the cutoff (97.7%-ROC 0.98[19]and 91%[18]). However, one of the largest single-center studies reported a modest diagnostic utility by quantitative analysis (4.65 for SR and 0.27% for mass elasticity) for discriminating pancreatic masses[17]. One analysis of the qualitative pattern for diagnosing malignancy reported 94% accuracy (ROC curve 0.854,P< 0.0001)[20]with high interobserver coincidence (0.77 and 0.84,respectively)[20,21]. By using quantitative analysis, bias in selecting the target was diminished (accuracy 89.7%)[17].

Table 1 Relationship between Young's Modulus and different densities of polyvinyl alcohol phantoms

Table 2 Strain ratios (B/A) and regions of interest: A and B
Figure 3 Comparison of endoscopic ultrasound images: A: Phantom concentration 1; B: Phantom concentration 5.
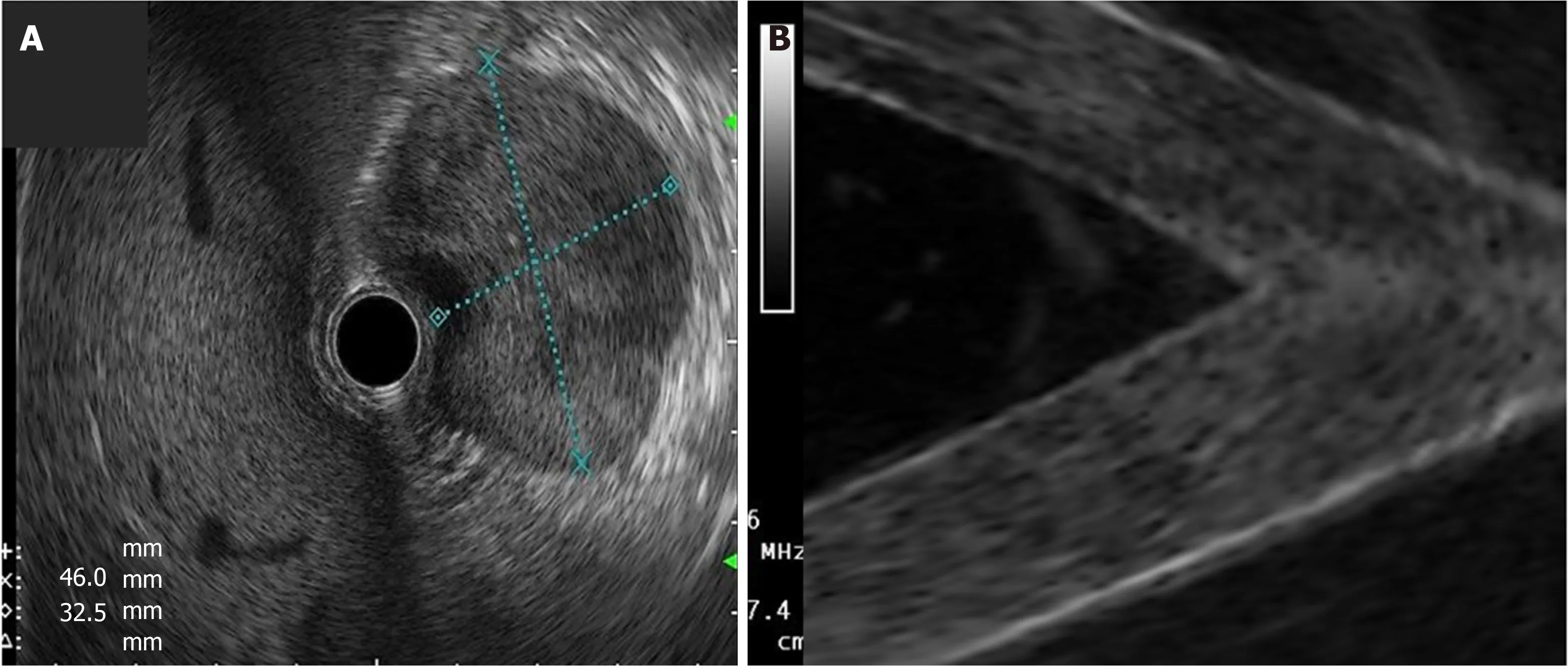
Figure 4 Type of lesions: A: Real homogeneous; B: Simulated homogeneous that refers to the liquid component inside the polyvinyl alcohol (PVA) phantom (blue arrow), surrounded by 15% PVA (concentration 9) and 20% PVA (concentration 10).
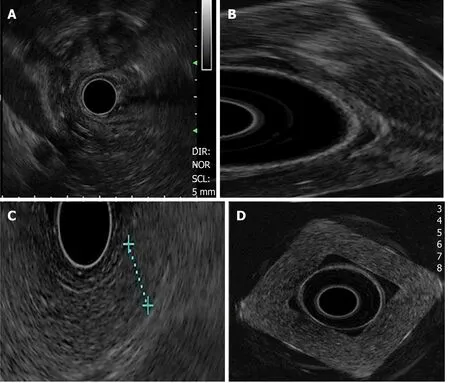
Figure 5 Type of lesions: A: Real heterogeneous lesion; B: Simulated heterogeneous lesion of hypoechoic predominance (concentration 1); C: Normal pancreatic tissue; and D: Simulated homogeneous image: phantom with 20% polyvinyl alcohol (concentration 10).
Furthermore, multilayer perceptron neural networks can be trained to classify focal lesions as either benign or malignant (accuracy 95%)[21]. Our phantom was designed to distinguish lesions, increase the n (repetitions), and evaluate skills for selecting a target, while improving spatio-temporal and haptic skills. A great advantage of practice with our phantom is that there is no need to practice EUS/EUS-E exclusively on animals. Qualitative pattern analysis yielded a high accuracy of 92.9% (ROC: 0.95) for the differential diagnosis between benign and malignant lymph nodes (LNs)[22]. The accuracy for discriminating between these is of great importance for prognosis and selection of appropriate therapy[23]. Due to the characteristics of LNs, these can also be simulated using our phantom. Another study reported lower yield of EUS-E (strain ratio) in detecting LNs but prevalence was greater (61%) in 34 patients, and it showed great heterogeneity (large width of the 95% confidence intervals)[24]. Learning in clinical scenarios in order to acquire skills has ethical and legal implications. The low prevalence of cases is a severe limit to training, in addition to the fact that in most centers, it is the expert who performs the interventions[1]. Regarding biomaterials, these have been used to obtain acoustic, optical and elastographic images[8,11,12,18]. In order to have greater realism in our simulated lesions, we needed to assess the mechanical properties (elasticity/stiffness) of tissue. In our experiment, biomaterial concentration was inversely proportional to the degree of tissue elasticity. The retention of liquid within the fibers produces echogenic differences. If we increase the density of the biomaterial, it will tend to be more homogeneous and hyperechoic. Density disperses sound and modifies impedance[16].

Figure 6 Cystic lesion: A: A hypoechoic image surrounded by a hyperechoic wall is visible, which produces a posterior reinforcement compatible with a pseudocyst of the pancreas (real image); and B: Endoscopic ultrasound contrast of the interior and exterior of the polyvinyl alcohol phantom (concentration 10): A hypoechoic image (inside) surrounded by a hyperechoic image (wall).

Figure 7 Solid lesion: A: Real; and B: Simulated (concentration 10).
In our study, density manipulation made it possible for us to build more realistic models. The presence of bubbles within the material increased the degree of realism. The degree of water retention within the phantoms enables the simulation of different injuries. The 20% concentrations (C5and C10) contain less water (solid lesions), in contrast to those at 7% (C1and C6), which contain a greater quantity (semi-solid). PVA characteristics are dynamic and differ when densities are compared. The area of least elasticity (> M.Y) is the point of greatest strength and cross-linking. The zone of least tension is the place where the transducer exerts pressure (deformity). The advantages of using PVA phantoms are as follows: (1) They do not require different equipment to that commonly used for patients, however, for the animal model they do; (2) Organs and lesions, whether hard or soft, can be simulated by modifying the molecular weight, concentration and freeze/thaw cycles of PVA; and (3) The simulators are inexpensive, this will vary depending on the size and sophistication of the phantom, for example depending on the completeness of an organ. In this work, as it only consisted of phantom characterization, each phantom costs approximately $15 to $20; 4) phantoms can be reused many times, provided they are kept immersed in water at room temperature (25-27°C) after use. Limitations in this study include: (1) It is necessary to submerge the PVA phantom in the water container; and (2) The main problem with EUS-E refers to difficulties in controlling tissue compression by the EUS transducer that may increase errors in measurement. Knowledge of the elasticity coefficient made it possible to create solid and semi-solid organs; both homo and heterogeneous, as well as more realistic cystic and solid lesions, due to the advantages of the viscoelastic properties of the phantom.

Figure 8 Elastographic images. A: Diagram showing color distribution; B: Color scale (elastography) of phantom concentration (C) 6; and C: Contrast between phantom C6 (green hue) molecular weight 2 = 146000– 186000 vs phantom C5 (dark blue hue) with molecular weight 1 = 85000 – 124000.
CONCLUSION
In conclusion, the use of PVA phantoms with different densities allowed adequate and consistent simulation of organs and digestive lesions, visible by EUS-E.
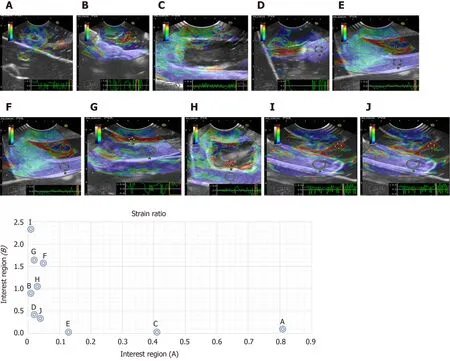
Figure 9 Relationship between the region of interest A and B and the (B/A) strain ratio.
ARTICLE HIGHLIGHTS


Research results
The density of PVA phantoms depended on MW and C. The stiffness of these phantoms was correlated with higher MW and C (correlationr= 0.8,P= 0.01) as well as with increasing density and M.Y. All simulated lesions were visible using EUS. We calculated elasticity and deformation parameters of solid (blue) areas, contrasting with the norm (Kappa = 0.8; high degree of satisfaction)
Research conclusions
The use of PVA phantoms with different densities allowed adequate and consistent simulation of organs and digestive lesions, visible by EUS/EUS-E. Knowledge of the elasticity coefficient made it possible to create different lesions.
Research perspectives
Training in a clinical setting has medical and legal implications. Skill and abilities depend on shortening the learning curve. However, in order to achieve this, a model must be realistic. PVA phantoms were demonstrated to be feasible, economical and realistic models for EUS/EUS-E training.
ACKNOWLEDGEMENTS
To Dr. Jorge Cerecedo-Rodríguez (Hospital Ángeles Acoxpa) for his contribution to the interpretation of the endosonographic images. Thanks to the engineers Yair Pacheco, Javier Márquez Cortez (Medical Scope) and Lilia Vázquez Romero (Endomédica, S.A. de C. V) for informing us about the technical aspects of obtaining EUS/elastography images.
杂志排行
World Journal of Gastroenterology的其它文章
- Role of succinate dehydrogenase deficiency and oncometabolites in gastrointestinal stromal tumors
- Acupuncture improved lipid metabolism by regulating intestinal absorption in mice
- Efficacy of pancreatoscopy for pancreatic duct stones: A systematic review and meta-analysis
- Construction of a convolutional neural network classifier developed by computed tomography images for pancreatic cancer diagnosis
- Mixed epithelial endocrine neoplasms of the colon and rectum – An evolution over time: A systematic review
- Transjugular intrahepatic portosystemic shunt for Budd-Chiari syndrome: A comprehensive review
