Value of Preoperative Neutrophil-to-Lymphocyte Ratio in Predicting Prognosis of Surgically Resectable Urinary Cancers:Systematic Review and Meta-Analysis
2020-10-03ZhanWangXuWangWendaWangGuoyangZhengHaoGuoYushiZhang
Zhan Wang,Xu Wang,Wenda Wang,Guoyang Zheng,Hao Guo,Yushi Zhang
Department of Urology,Peking Union Medical College Hospital,Chinese Academy of Medical Sciences &Peking Union Medical College,Beijing 100730,China
Key words:urinary cancers;neutrophil-to-lymphocyte ratio;inflammatory biomarkers;prognostic factors;meta-analysis
Objective Accumulated evidence has suggested that there is a close association between preoperative neutrophilto-lymphocyte ratio (NLR) and prognosis of various malignant tumors.However,the relationship between NLR and surgically resectable urinary cancers remains contradictory.Therefore,we performed this systematic review and meta-analysis to explore whether preoperative NLR could predict the prognosis of surgically resectable urinary cancers.Methods After searching the Embase,PubMed/MEDLINE and Cochrane databases and screening the articles,we finally included 25 studies involving 15950 patients.Hazard ratios (HRs) and their 95% confidence intervals(CIs) were extracted to assess the association between preoperative NLR and the overall survival (OS) and cancerspecific survival (CSS) of surgically resectable urinary cancers.Results The pooled results revealed that an elevated preoperative NLR could predict a worse OS (HR=1.40,95%CI:1.26-1.54,P<0.001) and CSS (HR=1.43,95%CI:1.27-1.59,P<0.001) in urinary cancers.In addition,our analyses also suggested that high preoperative NLR was associated with worse prognosis in renal cell carcinoma (OS:HR=2.06,95%CI:1.54-2.76,P=0.131;CSS:HR=2.46,95%CI:1.46-4.16,P=0.178),upper tract urothelial carcinoma (OS:HR=1.91,95%CI:1.50-2.42,P=0.616;CSS:HR=1.84,95%CI:1.41-2.39,P=0.001),bladder cancer (OS:HR=1.09,95%CI:1.02-1.17,P<0.001;CSS:HR=1.05,95%CI:1.01-1.09,P=0.163) and prostate cancer (OS:HR=1.69,95%CI:1.19-2.41,P=0.714).Regardless of the participants’race or the cutoff value of the preoperative NLR,the results remained valid.Conclusion Elevated preoperative NLR could predict a worse prognosis in surgically resectable urinary cancers,namely,renal cell carcinoma,bladder cancer,prostate cancer and upper tract urothelial carcinoma.
URINARY cancers are one of the most common malignancies that threaten both men and women worldwide.According to the latest survey,it is estimated that there will be 158 220 new cases and 33 420 deaths in the United States for both sexes,ranking fifth in new cases and sixth in deaths of all malignancies.[1]Although a set of new preoperative and postoperative adjuvant treatment modalities,such as immunotherapy and molecular targeted drugs,have been developed,a subset of patients still die within a short time after surgery due to the rapid progression or reoccurrence of urinary cancers.Therefore,finding better preoperative prognostic biomarkers could hopefully prolong the survival span and change the postoperative follow-up routines.
Emerging evidence has revealed that the systemic inflammatory reaction (SIR) plays a critical role in the development and progression of various cancers,including malignant tumors of the digestive,respiratory and urological systems.As a marker of SIR,the neutrophil-to-lymphocyte ratio (NLR) has displayed great potential in predicting the prognosis of urinary cancers.[2-4]However,since the results of different studies remain inconsistent or even contradictory regarding the role of NLR in surgically resectable urinary cancers,we conducted this systematic review and meta-analysis to obtain a more reliable assessment.
MATERIALS AND METHODS
Literature search
We systematically searched the PubMed/MEDLINE,Embase and Cochrane databases for all possible studies without restrictions.The search strategy combined the medical subject heading (Mesh) terms NLR (e.g.,‘‘neutrophil-to-lymphocyte ratio’’ or ‘‘neutrophil lymphocyte ratio’’) with words related to urinary cancers (e.g.,“renal cancer”,“bladder cancer”,“prostate cancer”,“urothelial cancer” or “transitional cell carcinoma”) and prognosis (e.g.,“outcome”,“prognosis”,“prognostic’’,‘‘survival”,“cancer specific survival” or “overall survival”).The last search was updated on July 18,2019.
Inclusion and exclusion criteria
Studies were eligible if they met all the following criteria:(1) Studies evaluated preoperative NLR as a prognostic factor in urothelial cancers,such as renal cell cancer (RCC),bladder cancer (Bca),prostate cancer(Pca) or upper urinary tract urothelial cancer (UTUC);(2) Studies provided survival data on overall survival(OS) and/or cancer-specific survival (CSS);and (3)Hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) orP-values of CSS or OS can be found or calculated based on information provided in the article.
The exclusion criteria were as follows:(1) review articles,editorial comments,letters,expert opinions,conference abstracts,or case reports;(2) articles containing overlapping or duplicate data;(3) patients who received neoadjuvant treatment such as preoperative chemotherapy or radiotherapy;(4) patients who did not undergo an operation;and (5) incomplete or no survival data regarding OS or CSS.
Data extraction and quality control
For each eligible study,the following items were extracted:first author’s name,year of publication,country,tumor type,number of patients,median age,gender composition,NLR cut-off value,median follow-up period,survival outcomes,variate analysis type,andHRs of OS or CSS and 95%CIs.We used theHRs of multivariate analysis if both univariate and multivariate analyses were conducted.
The Newcastle-Ottawa Scale (NOS) was applied to assess the quality of all the enrolled studies.Any included study with a total score of more than 5 was considered good quality.The search was conducted,and the titles and abstracts of all initially identified studies were assessed independently by two authors (WZ and WX).Any discrepancies were solved through group discussion or a third author (ZGY) to establish a consensus.
Statistical analysis
TheHRs with their 95%CIs from each study were used to calculate pooledHRs.Cochran’sQ-test and HigginsI2statistics were applied to assess the heterogeneity of the pooled results.I2>50% orP<0.05 was regarded as heterogeneity.The fixed effects model (Mantel-Haenszel method) was used if there was no heterogeneity;otherwise,the random effects model was applied.In addition,we performed subgroup analysis and sensitivity analysis to identify the source of heterogeneity.Egger’s linear regression test was used to evaluate publication bias,andP<0.05 was considered significant.If publication bias existed,we used the Trim and Fill method to assess the influence of publication bias on the effect estimate.All statistical analyses were performed using STATA software version 14.0(STATA Corporation,College Station,TX,USA).AllPvalues were two-sided.
RESULTS
Characteristics of the included studies
After searching the PubMed/MEDLINE,Embase and Cochrane databases and removing duplicates,we initially found 443 articles.After having read the titles and abstracts,we excluded 383 articles that were reviews,conference abstracts,editorial assessments,letters or studies in which no patients undergoing an operation.Afterward,60 full-text original articles were screened.As a result,we excluded another 35 articles since 23 provided no or incomplete survival data regarding CCS or OS;7 focused on neoadjuvant radiotherapy;3 were related to derived NLR rather than NLR;2 contained overlapping samples.In the end,25 studies[2-26]met our criteria and were included in our final meta-analysis (Figure 1).Characteristics of all the included studies are shown inTable 1.
The 25 eligible studies contained 15950 cases from 8 countries (America,Korea,Singapore,Poland,Japan,Italy,China and Austria).Among the 25 studies,10[7,9,11,13,16,18,21-23,25]explored the prognostic role of preoperative NLR in UTUC,which contained 6365 patients;8 studies[2,5,12,15,17,19,20,24]in RCC with 3568 patients;2[3,8]in Pca with 2293 patients;5[4,6,10,14,26]in Bca with 3724 patients.Regarding the survival results,17 studies[2-8,10,12,14,15,17,18,20,23,24,26]focused on the predictive role of NLR in OS,with another 17[3,5-7,9-11,13,16,18,19,21-26]on CSS.All 25 studies received scores of more than 5 according to the NOS and were deemed to have good quality.
Overall survival
As shown inFigure 2andTable 2,it’s evident that elevated preoperative NLR could predict a worse prognosis in urinary cancers concerning OS with a pooledHRof 1.40 (95%CI:1.26-1.54,Pheterogeneity<0.001).Subgroup analysis by cancer type revealed that a higher preoperative NLR was also associated with a poorer OS in RCC[2,5,12,15,17,20,24](HR=2.06,95%CI:1.54-2.76,Pheterogeneity=0.131),UTUC[7,18,23](HR=1.91,95%CI:1.50-2.42,Pheterogeneity=0.616),Bca[4,10,13,14,26](HR=1.09,95%CI:1.02-1.17,Pheterogeneity<0.001) and Pca[3,8](HR=1.69,95%CI:1.19-2.41,Pheterogeneity=0.714).
Furthermore,another subgroup analysis by ethnicity suggested that a high preoperative NLR remained a worse predictor for OS in both Asians[3-5,7,8,12,14,15,17,18,20](HR=1.89,95%CI:1.58-2.25,Pheterogeneity=0.203) and Caucasians[2,6,10,23,24,26](HR=1.09,95%CI:1.02-1.16,Pheterogeneity=0.001).
Further analysis stratified by the NLR cut-off value revealed that regardless of whether the NLR cutoff was lower or higher than 2.7,an elevated NLR could still predict a worse prognosis in urinary cancers(NLR<2.7[2-5,7,8,12,20]:HR=1.77,95%CI:1.49-2.11,Pheterogeneity=0.268;NLR≥2.7[6,10,14,15,17,18,23,24,26]:HR=1.15,95%CI:1.05-1.26,Pheterogeneity<0.001).
Cancer-specific survival
As shown inFigure 3andTable 3,a high preoperative NLR was associated with a worse CSS in urological cancers[3,5-7,9-11,13,16,18,19,21-26](HR=1.43,95%CI:1.27-1.59,Pheterogeneity<0.001).Further subgroup anal-ysis by tumor site indicated that the NLR remained a prognostic biomarker of UTUC[7,9,11,13,16,18,21-23,25](HR=1.84,95%CI:1.41-2.39,Pheterogeneity=0.001),RCC[5,19,24](HR=2.46,95%CI:1.46-4.16,Pheterogeneity=0.178),Bca[6,10,26](HR=1.05,95%CI:1.01-1.09,Pheterogeneity=0.163).Since only one paper explored the CSS of Pca,we didn’t perform the subgroup analysis of Pca.
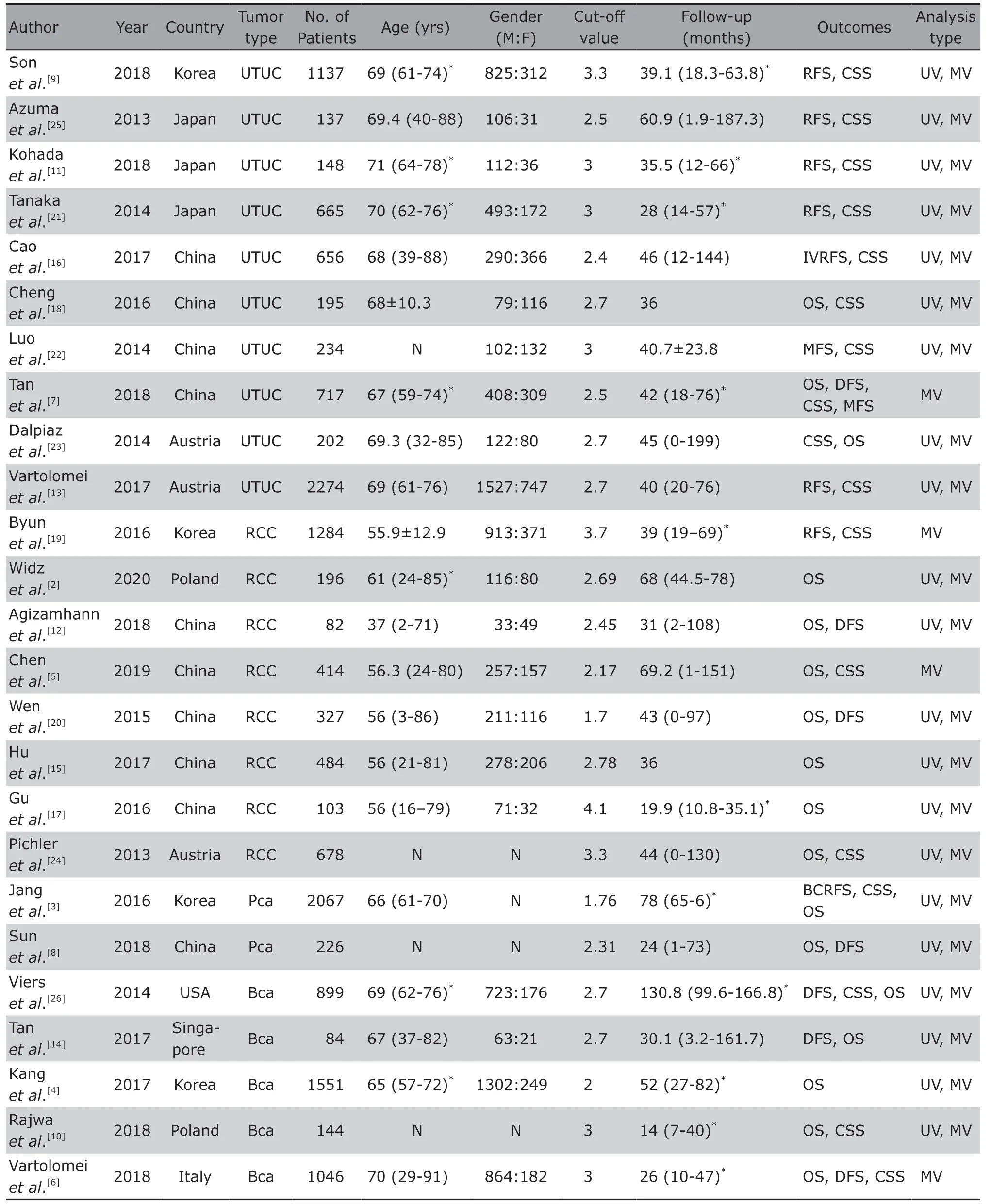
Table 1.Characteristics of all the studies included in our meta-analysis

Table 2.Subgroup analysis of all included articles regarding OS
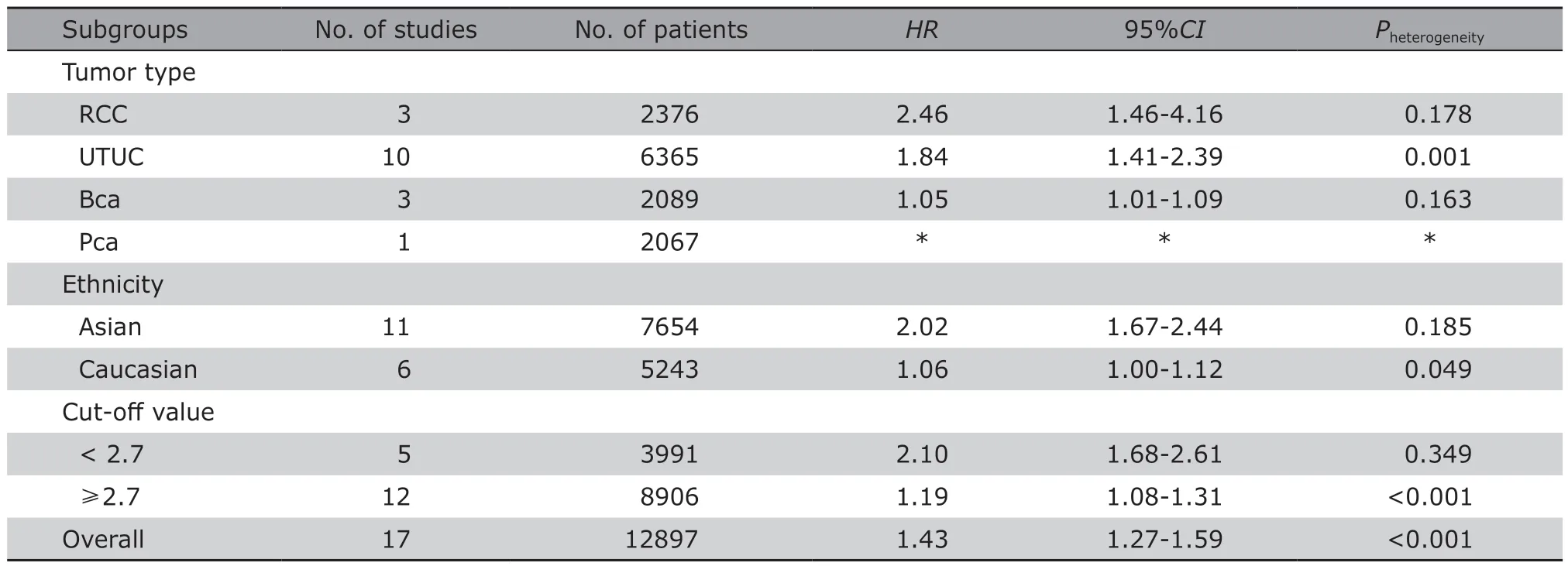
Table 3.Subgroup analysis of all included articles regarding CSS
In addition,when stratified by race,the subgroup analysis revealed that elevated NLR could still predict a worse prognosis in urinary cancers (Asian[3,5,7,9,11,16,18,19,21,22,25]:HR=2.02,95%CI:1.67-2.44,Pheterogeneity=0.185;Caucasian[6,10,13,23,24,26]:HR=1.06,95%CI:1.00-1.12,Pheterogeneity=0.049).
Another subgroup analysis by NLR cut-off demonstrated that regardless of whether the NLR cutoff was higher or lower than 2.7,preoperative NLR remained a worse prognostic marker (NLR<2.7[3,5,7,16,25]:HR=2.10,95%CI:1.68-2.61,Pheterogeneity=0.349;NLR≥2.7[6,9-11,13,18,19,21-24,26]:HR=1.19,95%CI:1.08-1.31,Pheterogeneity<0.001).
Heterogeneity
As shown inFigures 2and3,there was heterogeneity in our meta-analysis(OS:I2=82.8%,P<0.001;CSS:I2=81.8%,P<0.001).Therefore,we performed sensitivity analysis by sequentially omitting each study(Figure 4).The sensitivity analysis results showed that the article of Rajwaet al.[10]and the article of Vierset al.[26]may be the sources of heterogeneity.Therefore,we omitted the two articles and performed the meta-analysis again,and the results regarding OS(HR=1.78,95%CI:1.53-2.07,Pheterogeneity=0.135) and CSS (HR=1.91,95%CI:1.55-2.37,Pheterogeneity=0.001)remained valid.
Publication bias
Egger’s test was carried out to identify potential publication bias in our enrolled studies.The results showed that there was significant publication bias in the analysis of the pooled OS and CSS (PEgger<0.001).Therefore,we used the Trim and Fill method to assess the effect of publication bias,and the results showed that the adjusted pooledHRs for OS and CSS were also significant (OS:HR=1.209,95%CI:1.095-1.335;CSS:HR=1.142,95%CI:1.019-1.280),which was still consistent with the primary results (as presented inFigure 5).
DISCUSSION
Although many new therapies have been developed for the treatment of urinary cancers,such as chemotherapy,radiotherapy and molecular-targeted therapy,surgery remains the main therapeutic strategy and can provide a radical cure.Currently,the most widely used preoperative prognostic assessment strategy is the TNM staging system,which is still incomplete and imprecise.The identification of new prognostic factors may contribute to a more precise preoperative assessment,thus promoting survival outcomes and optimising follow-up routines.Recently,enormous evidence has suggested that NLR is closely related to the prognosis of malignant urinary tumors.However,the role of the NLR in surgically resectable urinary cancers remains unexplored,which is the reason why we performed this meta-analysis.Our studies enrolled 25 studies containing 15 950 patients,which were deemed good quality according to the criterion of the NOS scoring system.From the results of our meta-analysis,we could conclude that elevated preoperative NLR could predict a worse OS and CSS in urinary cancers,namely,RCC,UTUC,Pca and Bca.
However,the deeper underlying mechanism between the NLR and survival is still poorly understood.The most widely accepted hypothesis is the tumor micro-environment theory,which is crucial for the angiogenesis,viability,motility and invasion of tumors.[27]NLR variations illustrate an elevated neutral-based inflammatory reaction and a weakened lymphocyte-dependent immune response.Cancer cells can create different kinds of cytokines,such as IL-2,IL-6,VEGF and myeloid growth factors,which can increase the count of tumor-infiltrating neutrophils.[17]In addition,the increased neutrocytes could enhance their ability to secrete potent angiogenesis cytokines,such as vascular endothelial growth factor and reactive oxygen species,thus leading to DNA damage and genetic instability in addition to stimulating tumor proliferation and neo-vascularization in the micro-environment.[4,28,29]On the other hand,the presence of lymphopenia indicates a relative inefficiency of lymphocytes,and tumor-related lymphocytes have previously been shown to suppress tumour development in some cases.
However,there are still several limitations in our meta-analysis.First,most of the enrolled studies in our meta-analysis were retrospective observational studies.Although the quality has been assessed as good under the criterion of the NOS scoring system,the quality of evidence was still poor.Second,there was significant heterogeneity in some analyses concerning both OS and CSS.Since the tumor site may be a potential source of heterogeneity,we divided the eligible studies into several independent groups to eliminate heterogeneity.However,in the OS of the Bca group and CCS of the UTUC group,heterogeneity also existed.After applying sensitivity analysis to all the articles,we finally identified 2 articles that may affect the stability of our pooled results.Furthermore,we still cannot rule out the possibility that there may be other factors causing the heterogeneity,such as the patients’ baseline conditions,the patients’ postoperative treatments,and the follow-up period.Since there was only one study concerning the CSS of PCa,we did not perform subgroup analysis on this group,which may be another disadvantage of our meta-analysis.Third,publication bias was detected in our meta-analysis.Studies with positive results are much easier to publish than studies with negative results,which could lead to publication bias.Although we tried our best to acquire as many eligible articles as possible without any restrictions,the Egger’s test still suggested significant publication bias in our study.To avoid the effect of potentially negative outcomes,we used the Trim and Fill method to correct our results.However,we still could not completely rule out the possibility of publication bias.
In conclusion,our pooled results revealed that preoperative NLR could act as a potential prognostic marker in malignant urinary tumors.In other words,elevated preoperative NLR was associated with a worse OS and CSS in RCC,Bca,Pca and UTUC,which may help doctors stratify patients and change the postoperative follow-up routines.
Conflict of Interests Statement
The authors declare no competing interests.
杂志排行
Chinese Medical Sciences Journal的其它文章
- Enhancing Quality of Patients Care and Improving Patient Experience in China with Assistance of Artificial Intelligence
- Advance in Functional Restoration of Injured Nerve with Low Level Laser and its Utilization in the Dental and Maxillofacial Region
- Treatment of Retroperitoneal Cavernous Lymphangioma:A Case Report
- A Homozygotic Mutation in KDSR may Cause Keratinization Disorders and Thrombocytopenia:A Case Report
- Similarities and Differences of Early Pulmonary CT Features of Pneumonia Caused by SARS-CoV-2,SARS-CoV and MERS-CoV:Comparison Based on a Systemic Review
- Effect of MR Field Strength on the Texture Features of Cerebral T2-FLAIR Images:A Pilot Study