Modified pararectus approach for treatment of atypical acetabular anterior wall fracture:A case report
2020-09-15
Jun-Jie Wang,Jiang-Dong Ni,De-Ye Song,Mu-Liang Ding,Jun Huang,Guang-Xu He,Wen-Zhao Li,Department of Orthopedics,The Second Xiangya Hospital of Central South University,Changsha 410011,Hunan Province,China
Abstract
Key words:Acetabulum;Fracture;Modified;Pararectus approach;Case report
INTRODUCTION
Before Judetet al[1]and Letournelet al[2]proposed and developed the classification and management of acetabular fracture in the late 20thcentury,acetabular fractures were treated inappropriately.According to the Judet-Letournel classification,the anterior wall fracture is a separation of the anterior wall of the articular surface,together with the corresponding segment of the iliopectineal line[2].However,lesions of the anterior wall with preservation of the pelvic brim were not included in the Judet-Letournel classification,but have been described by others[3,4].The morphology of the isolated anterior wall fracture is similar to that of the posterior wall fracture.But the anterior wall fracture without involvement of the pelvic brim is rare,so it is named atypical anterior wall fracture in some literature[4].In this type of acetabular fracture,there is always an extraarticular component of different sizes accompanying with the articular component,including the anterior inferior iliac spine (AIIS) and the interspinous region,and even the anterior superior iliac spine (ASIS) or iliac wing[3,4].
Indications for surgical treatment of acetabular fracture are incongruent or unstable fractures with verified dislocation greater than 5 mm[5].The modified Smith-Peterson approach described by Judetet al[1]is used for the treatment of anterior wall fracture[3,4,5].Several modifications of the Smith-Peterson approach have been introduced,with different osteotomies or muscle striping for atypical anterior wall fracture[4,6,7].
This report describes a rare acetabular anterior wall fracture with preservation of the pelvic brim,but consisting of the AIIS and iliac wing.A modified pararectus approach was used for therapeutic management and was successful in achieving a good outcome.The advantages accruing from this approach include minimal tissue damage and sufficient exposure of the osseous lesions.
CASE PRESENTATION
Chief complaints
A 48-year-old Chinese woman presented with difficulty moving her right hip from abduction and external rotation after falling from 3 m that occurred 3 d ago.
History of present illness
Due to right hip pain,the patient underwent an X-ray examination in the outpatient department and was diagnosed with “right acetabular fracture,” after which she was admitted to the hospital.
Physical examination
The patient exhibited pain and external rotation of the right hip.Tenderness was present near the hip joint and movements were painful and limited.The neurovascular status was normal.
Imaging examination
Standard radiographs at admission revealed fractures of the right acetabular anterior wall in association with fractures of the AIIS and the iliac wing,with preservation of the pelvic brim (Figure1).Computed tomography showed fractures of the acetabular anterior wall,the AIIS,and the iliac wing with retained integrity of the pelvic brim(Figure1).
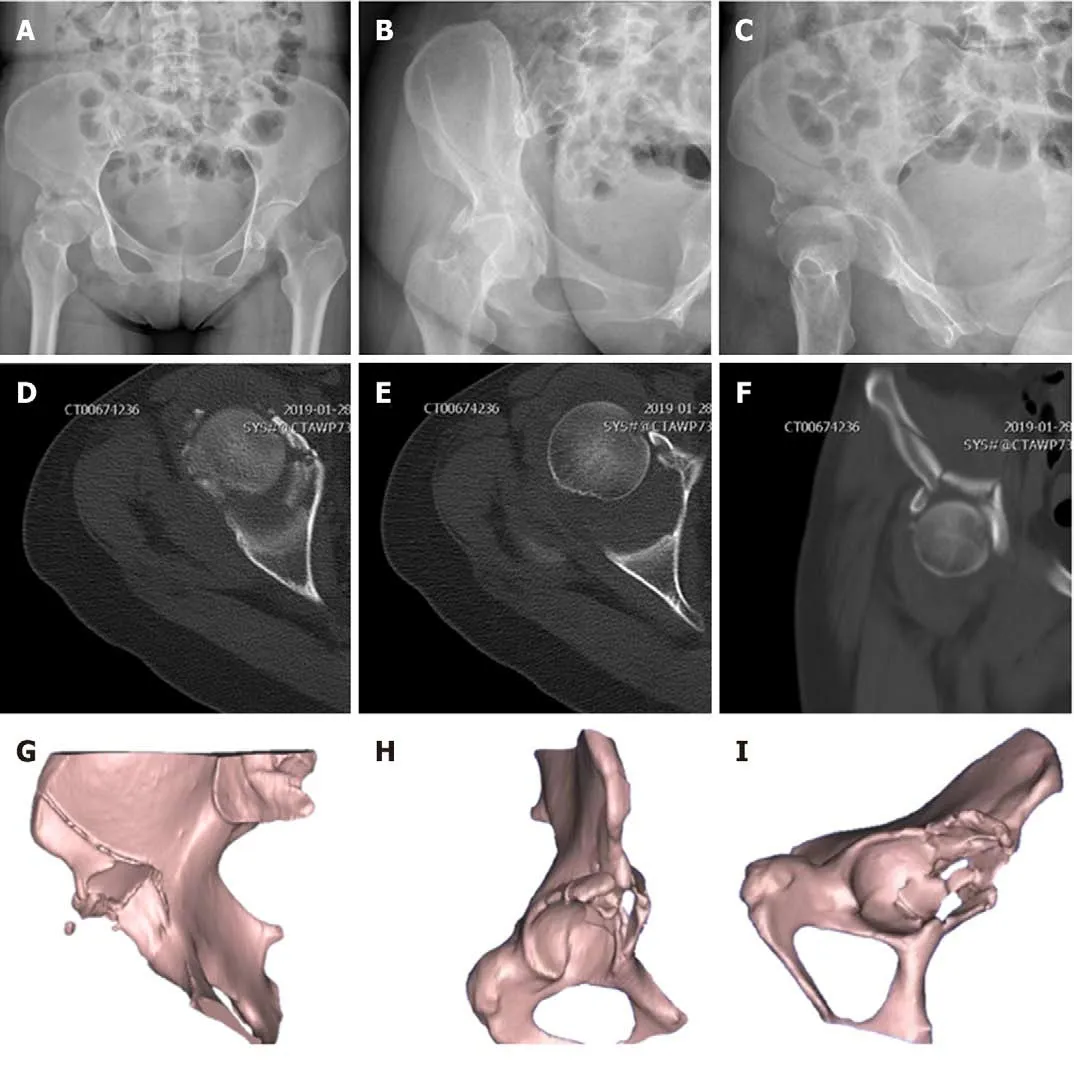
Figure1 Preoperative plain radiographs and computed tomography scans.A:Anteroposterior view radiography;B:Obturator oblique view radiography;C:Iliac oblique view radiography;D and E:Axial computed tomography (CT) images;F:Coronal CT image;G-I:Three-dimensional reconstructed CT images.
Preoperative closed reduction and skin traction
The patient underwent interim management by closed reduction of the hip dislocation and skin traction for 6 d.
Preoperative diagnosis and treatment plan
For the treatment of right atypical acetabular anterior wall fracture and iliac fracture,open reduction and rigid internal fixation were performedviaa modified pararectus approach under general anesthesia.
Surgical procedures
The surgery was performed on the 7thday following the traumatic injury.Under general anesthesia,the patient was placed supine on a radiolucent operating table and the ipsilateral leg was prepared and draped freely,facilitating reduction maneuvers.To reduce the tension of the iliopsoas muscle and protect the femoral nerve,hip joints were slightly flexed by putting a bump underneath both knees.In order to monitor potential iatrogenic bladder injury during surgery,a Foley catheter was placed in the bladder before surgery.
A modified pararectus approach was used,in which the skin incision was started from the junction of the medial and middle thirds of the line connecting the ASIS with the umbilicus to the junction of the middle and lateral thirds of the line connecting the symphysis with the ASIS,and extended distally-laterally to the AIIS (Figure2A).
To facilitate exposure of the anterior layer of rectus sheath,the subcutaneous fatty tissue,fascia of Camper,fascia of Scarpa,and external oblique muscle aponeurosis were dissected.The incision of the anterior fascial layer of rectus sheath and the transversalis fascia was made to expose the extraperitoneal space in the true pelvis,with care taken to identify the round ligament and the inferior epigastric vessels.The expanded first window of pararectus approach[8]was developed between the iliac crest and iliopsoas muscle by dissecting the iliacus muscle along the inner surface of the iliac crest and dragging it medially.By retracting the iliopsoas muscle laterally and the external iliac vessels medially,the second window[8]was created.Through the expanded first and second windows,both the anterior wall and anterior column could be seen (Figure2B).
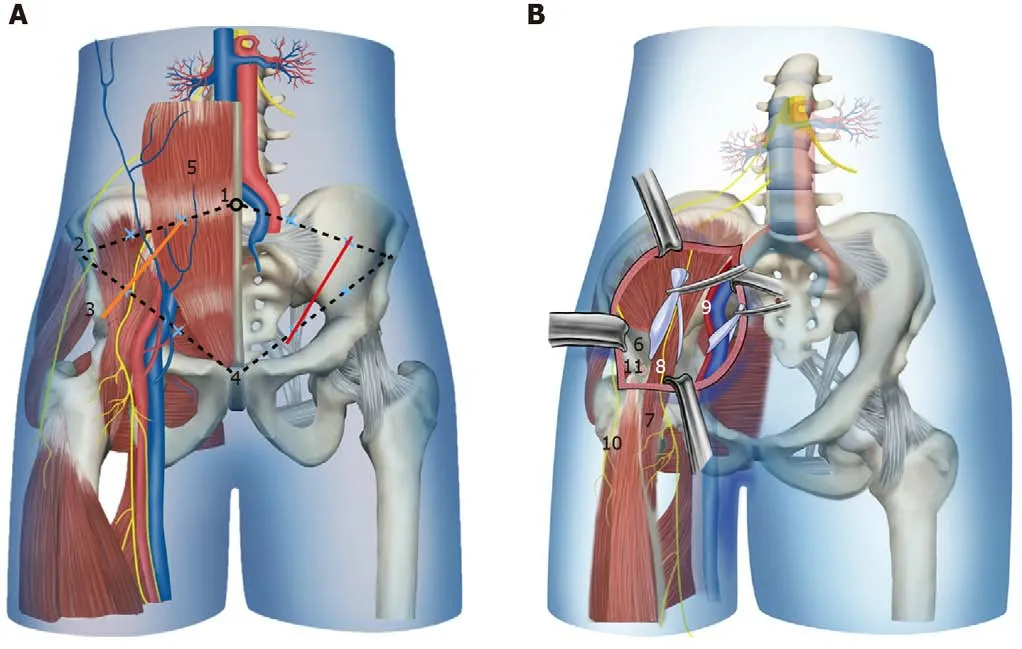
Figure2 Schematic drawing demonstrating the skin incision and anatomic structures in the modified pararectus approach.A:Skin incision;B:Anatomic structures.Orange line:Modified pararectus approach;Red line:Pararectus approach;1:Umbilicus;2:Anterior superior iliac spine;3:Anterior inferior iliac spine;4:Symphysis;5:Rectus abdominis;6:Iliac fossa;7:Iliopsoas muscle;8:Femoral nerve;9:External iliac vessels;10:Lateral femoral cutaneous nerve;11:Avulsion fracture of anterior inferior iliac spine.
Once the approach was complete,the fracture fragments were identified,namely,two main fragments of the anterior wall with superior extension of fracture above the iliopectineal line into iliac wing,and a fragment of AIIS that was attached by the direct head of the rectus femoris tendon.The reflected head of the rectus femoris tendon was released to allow mobilization of the fragment.Manual distraction was performed by placing a subtrochanteric Schanz screw parallel to the femoral neck,which was then used to visualize the joint after incision through the hip capsule,and the articular impaction was addressed.
The fracture fragments were anatomically reduced under direct visualization,and the cancellous bone void left beneath the elevated impacted fragments was filled with allograft.Interfragmentary lag screws were used to fix the AIIS and iliac wing.The fixation of anterior wall was achieved by using a nonlocking,precontoured,lowprofile reconstruction plate and a nonlocking T-shape plate.The T-shape plate was situated near the border of the acetabulum,and was slightly under-bent to enable compressing and buttressing of the fragments.Intraoperative fluoroscopy was used to evaluate the reduction and position of the implants.The hip capsule and rectus release were repaired,and the anterior layer of rectus sheath,subcutaneous tissue,and skin were sutured sequentially.A suction drain was placed for 24 h.
Prophylactic intravenous antibiotic was used from 30 min before surgery to 24 h postoperatively.Rivaroxaban was employed for 5 wk as prophylaxis against deep venous thromboembolism.The patient was started on muscle strengthening as soon as medically possible but with restricted mobilization to toe-touch weight-bearing for the first 3 mo.The postoperative X-rays and computed tomography scans revealed good reduction of the fracture (Figure3).
FINAL DIAGNOSIS
Right acetabular anterior wall fracture with preservation of the pelvic brim,associated with fracture of the AIIS and the iliac wing.
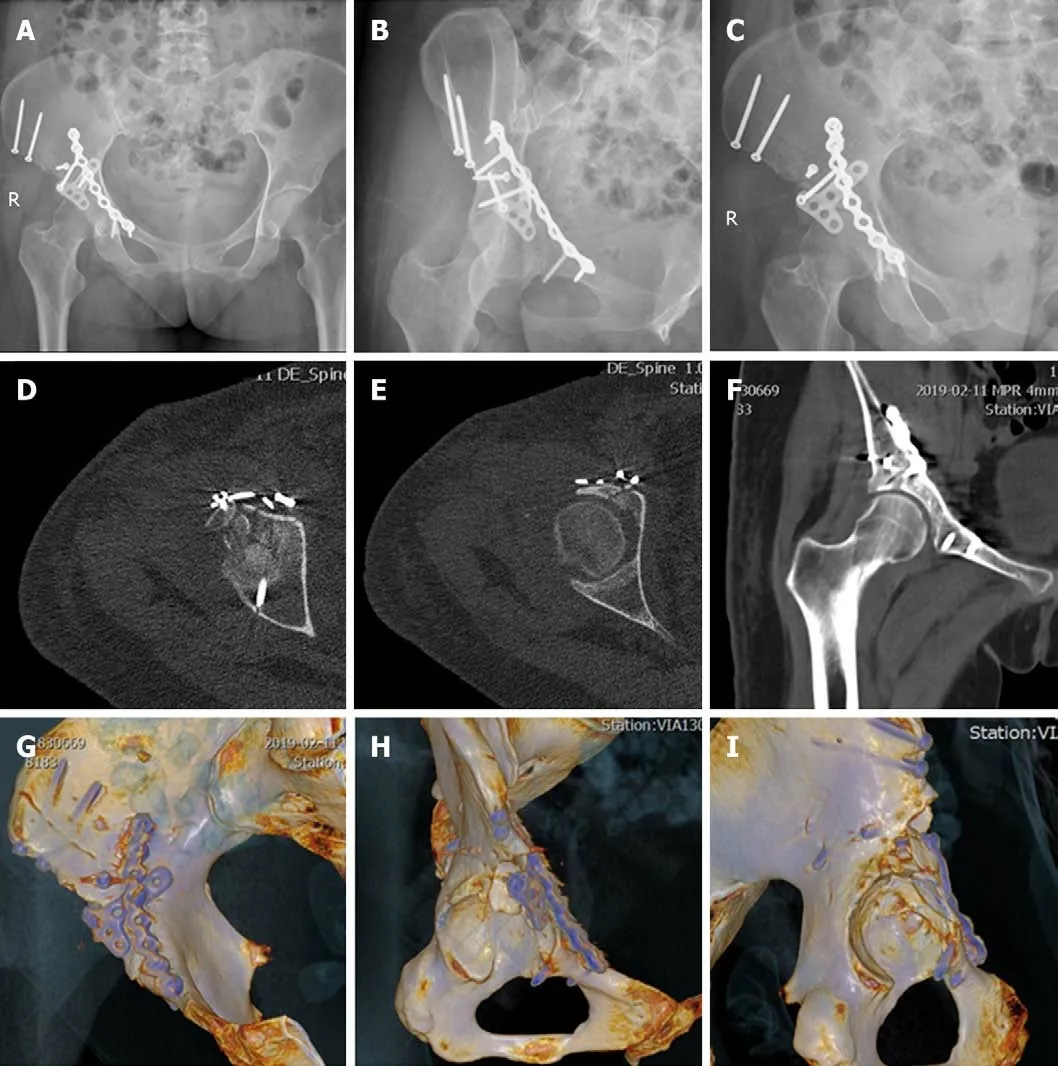
Figure3 Postoperative plain radiographs and computed tomography scans.A:Anteroposterior view radiography;B:Obturator oblique view radiography;C:Iliac oblique view radiography;D and E:Axial computed tomography (CT) images;F:Coronal CT image;G-I:Three-dimensional reconstructed CT images.
TREATMENT
The patient was treated by open reduction and internal fixation with interfragmentary lag screws,reconstruction plate and T-shape plateviaa modified pararectus approach.
OUTCOME AND FOLLOW-UP
The patient was followed monthly.At 9 mo postoperatively,an X-ray showed that the fracture lines were blurred.The patient was satisfied with the function of the injured hip (Figure4).
DISCUSSION
Acetabular anterior wall fractures with preservation of the pelvic brim are very uncommon.As far as we know,there are only ten cases reported previously in the literature[3,4,9].Mirovskyet al[9]reported an acetabular anterior wall fracture with anterior hip dislocation treated by hip arthroplasty in a 67-year-old woman.Badelonet al[10]and Piriouet al[3]reported three similar cases,but they were treated by open reduction and internal fixation.Lenarzet al[4]reported a series of anterior acetabula fracture without involvement of the pelvic brim,and defined the special form of acetabular anterior wall fracture as atypical anterior wall fracture of the acetabulum.
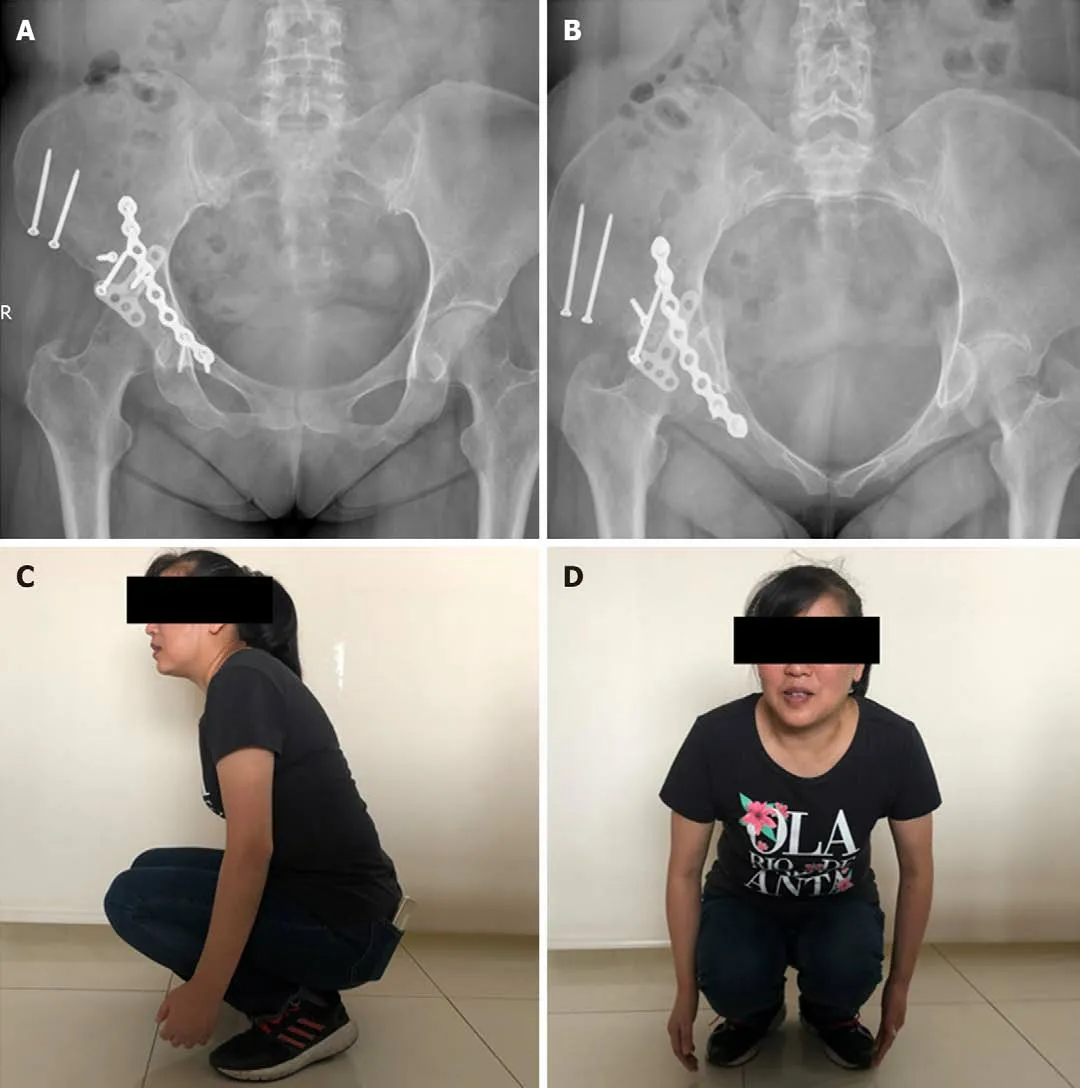
Figure4 Postoperative X-rays and hip mobility at 9 mo.A:Anteroposterior view radiography;B:Inlet view radiography;C and D:Flexion of the hip with a full load.
Previously reported cases and the present case have common features.The lesions,in all cases,included the anterior wall of the acetabulum with preservation of the pelvic brim,unlike the anterior wall fracture described in the Judet-Letournel classification.The anteriorsuperior part of the acetabulum,rather than the entire roof,was fractured,differing from the anterior wall fracture described in the Judet-Letournel classification[2].Furthermore,the fractures extended to the AIIS in all cases and even the interspinous region in some cases.The indications for surgical treatment of acetabular fracture are incongruent or unstable fractures with a dislocation verified to be greater than 5 mm[5],so that no alternative treatment to surgery was considered in our case.
The operative approach should provide access to the anterior column,anterior wall,AIIS,and hip joint for direct reduction and osteosynthesis.According to Tannast’s study about survivorship of the hip in 810 patients with operatively treated acetabular fractures,anterior wall fractures had the worst survivorship,which might be related to marginal impaction and nonanatomical articular reduction associated with limited exposure[11].Because the Smith-Petersen approach could provide exposure of the anterior column and wall extending from the inner table to the outer table,and a complete intra-articular view to judge reduction and address articular impaction[6],it was employed for open reduction and rigid internal fixation in all of the nine cases previously reported.The ilioinguinal approach,which is often used as a recommended treatment for anterior lesions,is absolutely incapable of treating such fractures because of limited potential for intraarticular manipulation through fracture line.Despite the excellent exposure of the Smith-Petersen approach for anterior acetabular fractures,it requires detachment of iliacus muscle,release of rectus femoris muscle,and even release of the attachment of the gluteus medius muscle or osteotomy of the ASIS for more extensile exposure.
The modified pararectus approach described here combines advantages of the pararectus approach and Smith-Petersen approach.It provides access to the anterior column and wall as with the pararectus approach but with less invasive tissue dissection[8].Furthermore,by changing the orientation of the skin incision towards the AIIS,the anterior impacted articular lesion could be manipulated under direct vision,after retracting fractured AIIS.Although the modified pararectus approach provides a less exposed area of intra-articular surface and outer table of iliac wing than the Smith-Petersen approach,it offered adequate view and operation space in our case and prevented further damage to the iliac wing from osteotomy.
The major advantage of the modified pararectus approach compared with the original pararectus approach is the enlarged first and second windows,so that fractures of the low anterior column with marginal impaction can be well operated.On the other hand,more dissection of subcutaneous tissue is needed,and a smaller range of the superior ramus of the pubis is exposed.
CONCLUSION
We report a rare acetabular anterior wall fracture with preservation of the pelvic brim,but consisting of the AIIS and iliac wing in a 48-year-old woman.This atypical acetabular anterior wall fracture is different from the Judet-Letournel classification in terms of morphology and surgical procedure.A modified pararectus approach was used in our case,which could facilitate exposure,reduction,and osteosynthesis for atypical acetabular fracture with less invasiveness.
杂志排行
World Journal of Clinical Cases的其它文章
- Assessment of diaphragmatic function by ultrasonography:Current approach and perspectives
- Computer navigation-assisted minimally invasive percutaneous screw placement for pelvic fractures
- Research on diagnosis-related group grouping of inpatient medical expenditure in colorectal cancer patients based on a decision tree model
- Evaluation of internal and shell stiffness in the differential diagnosis of breast non-mass lesions by shear wave elastography
- Real-time three-dimensional echocardiography predicts cardiotoxicity induced by postoperative chemotherapy in breast cancer patients
- Lenvatinib for large hepatocellular carcinomas with portal trunk invasion:Two case reports
