绍兴地区女性人工流产生殖道感染患病率及其影响因素分析
2020-08-21罗燕子高波潘海滔张涛丁海钢
罗燕子 高波 潘海滔 张涛 丁海钢
[摘要] 目的 分析紹兴地区女性人工流产生殖道感染患病率及其影响因素。 方法 选取2017年10月~2019年10月在我院收治的200例人工流产患者,根据有无生殖道感染分为感染组99例和未感染组101例。收集所有女性年龄、文化程度、职业、婚姻状况、联系方式等一般资料。采用问诊的方式收集所有女性初次性交年龄、性伴侣个数、流产次数、是否避孕、个人卫生情况、生殖道感染病史、流产后首次性生活时间等情况。所有女性均进行妇科检查和实验室检查计算感染率。采用Logistic回归分析人工流产后生殖道感染患病率影响因素。 结果 人工流产女性生殖道感染患病率为49.50%(99/200),其中以宫颈炎、念珠菌性阴道炎、附件炎最为多见。单因素分析结果显示,初次性交年龄、性伴侣个数、是否避孕、个人卫生情况、生殖道感染病史、流产后首次性生活时间等因素差异具有统计学意义(P<0.05),年龄、文化程度、职业、婚姻状况、流产次数等因素差异无统计学意义(P>0.05)。Logistic回归分析结果显示,初次性交年龄、性伴侣个数、是否避孕、个人卫生、生殖道感染疾病史、流产后首次性生活时间均为人工流产后生殖道感染的独立危险因素(P<0.05)。 结论 人工流产后生殖道感染的发病率较高,针对影响人工流产后生殖道感染发生的因素,通过健康宣教教育工作减少生殖道感染的发生,从而更好地关爱女性健康。
[关键词] 女性;人工流产;生殖道感染;患病率;影响因素
[中图分类号] R711.6 [文献标识码] B [文章编号] 1673-9701(2020)17-0060-05
Analysis on the prevalence rate and influencing factors of female abortion-induced genital tract infection in Shaoxing area
LUO Yanzi1 GAO Bo2 PAN Haitao3 ZHANG Tao3 DING Haigang4
1.Department of Family Planning, Shaoxing Women and Children's Hospital in Zhejiang Province, Shaoxing 312000,China; 2.Department of Gynecology, Shaoxing Women and Children's Hospital in Zhejiang Province, Shaoxing 312000, China; 3.Genetics Laboratory, Shaoxing Women and Children's Hospital,Shaoxing 312000, China; 4.Department of Medical Affairs, Shaoxing Women and Children's Hospital in Zhejiang Province, Shaoxing 312000, China
[Abstract] Objective To analyze the prevalence rate and influencing factors of female abortion-induced genital tract infections in Shaoxing area. Methods 200 cases of abortion patients who were admitted to our hospital from October 2017 to October 2019 were selected. According to the presence or absence of reproductive tract infection, the patients were divided into 99 cases in the infection group and 101 cases in the non-infection group. All general data about womens age, education, occupation, marital status, and contact information were collected. The age of first sexual intercourse,the number of sexual partners, the number of miscarriages, taking contraception or not, personal hygiene, the history of reproductive tract infections, the time of first sexual life after miscarriage were collected by inquiry. All women were given gynecological examination and laboratory examination to calculate the infection rate. Logistic regression was used to analyze the influencing factors for the prevalence rate of reproductive tract infections after abortion. Results The prevalence rate of reproductive tract infections in abortion women was 49.50% (99/200), among which cervicitis, candidal vaginitis, and appendicitis were the most common. According to the results of univariate analysis,there were statistically significant differences in factors such as age at first sexual intercourse, number of sexual partners, taking contraception or not, personal hygiene, history of reproductive tract infection, time of first sexual life after miscarriage(P<0.05). There were no statistically significant differences in factors such as age, education, occupation, marital status, and number of miscarriages(P>0.05). According to the Logistic regression analysis, the age of first sexual intercourse, the number of sexual partners,taking contraception or not, personal hygiene, history of reproductive tract infections,and the time of first sexual life after abortion were all independent risk factors for reproductive tract infections after abortion(P<0.05). Conclusion The prevalence rate of reproductive tract infections after abortion is high. In view of the influencing factors for the occurrence of reproductive tract infections after abortion, the occurrence of reproductive tract infections can be reduced through health education and education work, so as to better care for women's health.
[Key words] Women; Abortion; Reproductive tract infections; Prevalence rate; Influencing factors
妊娠3个月内用人工或药物方法终止妊娠称为人工流产,是避孕失败意外妊娠的补救措施,在控制人口数量方面起到了一定的作用,已成为当前世界生殖健康方面关注的公共卫生问题之一[1-2]。人工流产手术包括负压吸引、钳刮人工流产术,术后常伴有很多并发症,其中生殖道感染是人工流产女性主要并发症之一。人工流产技术是一种侵袭性操作,手术会破坏妇女生殖道环境,若术前宫颈受到损伤或生殖道有炎症,则增加生殖道感染易感性;若吸宫不彻底,子宫口与外界相通,子宫内有残余物易引起感染[3-4];此外,人工流产次数越多,生殖道感染等问题发生率越高,给妇女的生殖健康和心理健康产生严重危害。生殖道感染通常无症状,且与不孕症、新生儿感染、宫颈癌等多种疾病发生有关,并可增加感染艾滋病的危险性[5-6]。目前降低生殖道感染的发病率已成为计划生育技术服务迫切需要解决的问题之一。因此本研究旨在分析绍兴地区女性人工流产生殖道感染患病率及其影响因素,现报道如下。
1 资料与方法
1.1 一般资料
回顾性分析2017年10月~2019年10月在我院收治的200例人工流产患者的临床资料,本研究经医院伦理委员会批准进行。入组标准:①所有患者均经超声确诊为宫内妊娠;②所有患者均符合《妇产科学》关于生殖道感染的诊断标准;③年龄18~40岁;④均自愿要求终止妊娠者;⑤临床资料完整;⑥患者及家属知情并签署同意书。排除标准:①高危妊娠者;②非宫内妊娠者;③合并全身系统性疾病者;④精神障碍无法沟通交流者。
1.2 资料收集与检测方法
1.2.1 一般资料 分别在人工流产结束后1、4、12、24周对患者进行随访,采用调查表收集所有女性年龄、文化程度、职业、婚姻状况、联系方式等一般资料。采用问诊的方式收集所有女性初次性交年龄、性伴侣个数、流产次数、是否避孕、个人卫生情况、生殖道感染病史、流产后首次性生活时间等情况。
1.2.2 妇科及实验室检测 所有女性均进行妇科检查和实验室检查,取阴道分泌物检测阴道清洁度以及患者是否存在滴虫、细菌、衣原体、念珠菌性阴道炎、宫颈炎、附件炎及盆腔炎等,计算感染率。采集静脉血检查梅毒和人体免疫缺陷病毒(Human immunodeficiency virus,HIV),采用梅毒螺旋体抗体诊断试剂盒进行梅毒血清学筛选试验,阳性者再用ELISA法检测梅毒抗体;采用HIV抗体诊断试剂盒进行HIV初筛,经半自动ELISA法进行测定,阳性者再用另一种试剂手工测定;梅毒和HIV阳性结果送往疾控,免疫印迹法疾控确诊。梅毒梅毒螺旋体抗体诊断试剂盒、HIV抗体诊断试剂盒均购于英科新创(厦门)科技有限公司。
1.3 统计学方法
本研究所有计数数据均采用[n(%)]表示,以χ2检验两组间数据的比较,P<0.05为具有统计学差异,Logistic回归分析人工流产后生殖道感染患病率影响因素。本研究数据均采用SPSS21.0软件包进行分析。
2 结果
2.1 人工流产女性生殖道感染患病率
本研究人工流产女性生殖道感染患病率为49.50%(99/200),其中以宫颈炎、念珠菌性阴道炎、附件炎最为多见。所有患者均未见梅毒及HIV阳性。见表1。
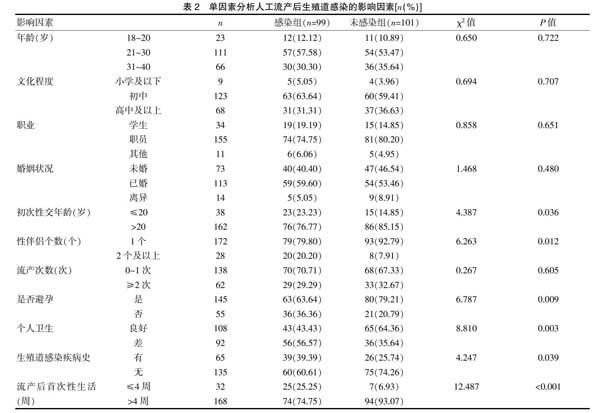
2.2 单因素分析人工流产后生殖道感染的影响因素
单因素分析结果显示,初次性交年龄、性伴侣个数、是否避孕、个人卫生情况、生殖道感染病史、流产后首次性生活时间等因素差异具有统计学意义(P<0.05),年龄、文化程度、职业、婚姻状况、流产次数等因素差异无统计学意义(P>0.05)。见表2。
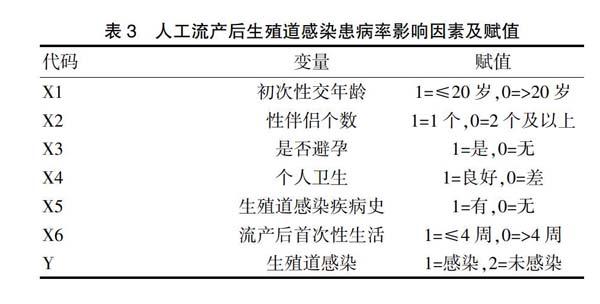
2.3 各影响因素及赋值
见表3。
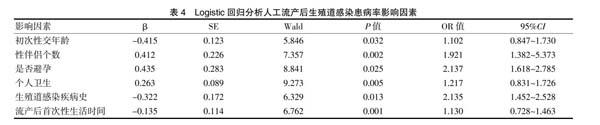
2.4 Logistic回归分析人工流产后生殖道感染患病率影响因素
Logistic回归分析结果显示,初次性交年龄、性伴侣个数、是否避孕、个人卫生、生殖道感染疾病史、流产后首次性生活时间均为人工流产后生殖道感染的独立危险因素(P<0.05)。见表4。
3 讨论
人工流产作为一种避孕失败后终止妊娠的补救措施,可严重破坏生殖道的正常防御机制,其中生殖道感染是人工流产的常见并发症,也是临床上常见的疾病之一[7-8]。生殖道感染是指多种病原微生物入侵引起的生殖道感染,其发病率较高[9],临床危害较大,给育龄妇女的生殖健康和身心健康带来严重影响。本研究结果显示,人工流产女性生殖道感染患病率为49.50%(99/200),这可能是人工流产手术可削弱甚至破坏女性生殖系统生理屏障的保护作用,引起外源性细菌感染或上行性细菌感染,严重者可引发盆腹膜炎甚至败血症。发生生殖道感染的女性者中以宫颈炎、念珠菌性阴道炎、附件炎最为多见,主要原因是人工流产可导致宫腔、阴道壁及宫颈口有大面积伤口,阴道酸性环境可使病原体繁殖增多,增加了阴道炎和宫颈炎的可能性[10-11]。
人工流产可直接造成女性健康的不良影响,本研究经Logistic回归分析结果显示,初次性交年龄、性伴侣个数、是否避孕、个人卫生、生殖道感染疾病史、流产后首次性生活时间均为人工流产后生殖道感染的独立危险因素(P<0.05)。初次性交年龄小,患者自我保护意识淡薄,多数未采取避孕措施,性伴侣个数较多且有性病等高危因素,更易发生人工流产后生殖道感染[12-13]。未采取合理的避孕方式可增加女性人工流产后生殖道感染的危险,避孕药物的使用、避孕套的不正确使用及宫内节育环的脱落等均可导致避孕失敗的发生,增加人工流产的发生率及生殖道感染的患病率[14-15]。个人卫生习惯的良好与人工流产后生殖道感染的发生密切相关,人工流产可降低患者生殖道抵抗力,若患者不注意个人卫生,清洗外阴时间间隔较长、不勤换内裤等,更易引起生殖道感染。是否有生殖道感染疾病史也是人工流产后生殖道感染发生的危险因素,大部分女性对生殖道感染的严重性认识不足,认为出现白带异常、外阴瘙痒等症状不影响日常生活,未能及时就医诊治,导致生殖道感染患病率增加[16-17]。流产后首次性生活时间过早也可增加生殖道感染的发生率,由于人工流产可损伤子宫内膜,破坏生殖道微环境,过早进行性生活可增加感染的发生率[18]。有学者通过研究发现[19],流产史、婚姻健康状况、个人或配偶健康状况等均是生殖道感染发生的影响因素。还有相关报道发现[20],配偶健康状况、避孕方式、初次性交年龄等是人工流产后发生生殖道感染的影响因素,由此可见人工流产后患者发生生殖道感染的因素较为复杂。
綜上所述,人工流产后生殖道感染的发病率较高,针对影响人工流产后生殖道感染发生的因素,通过健康宣教教育工作减少生殖道感染的发生,从而更好地关爱女性健康。
[参考文献]
[1] Karen Morgan,Meram Azzani,Si Lay Khaing,et al.Acceptability of women self-sampling versus clinician-collected samples for HPV DNA testing:A systematic review[J]. Journal of Lower Genital Tract Disease,2019,23(3):193-199.
[2] Bruce P,Blackshaw,Daniel Rodger. Ectogenesis and the case against the right to the death of the foetus[J].Bioethics,2018,33(1):76-81.
[3] Tanvi Dev,Neha Taneja,Deepak Juyal,et al. Upper genital tract infection due to Ureaplasma urealyticum:Etiological or syndromic management?[J]. Indian Journal of Dermatology Venereology & Leprology,2017,83(4):489-491.
[4] Khoudia Diop,Thi Tien Nguyen,Jérémy Delerce,et al. Corynebacterium fournierii, sp. nov.isolated from the female genital tract of a patient with bacterial vaginosis[J].Antonie Van Leeuwenhoek,2018,111(7):1165-1174.
[5] Sahar Bagheri,Rasoul Roghanian,Naser Golbang,et al. Molecular Evidence of chlamydia trachomatis infection and its relation to miscarriage[J]. International Journal of Fertility & Sterility,2018,12(2):152-156.
[6] Nirina Andersson,Isabella Preuss,Jens Boman,et al. Chlamydia infection among digital daters and nondigital daters[J].Journal of Lower Genital Tract Disease,2019, 23(3):230-234.
[7] W. Glenn,Mc,Cluggage. Recent developments in non-HPV-related adenocarcinomas of the lower female genital tract and their precursors[J]. Advances in Anatomic Pathology,2016,23(1):58-69.
[8] Pedro Vieira-Baptista,Svitrigaile Grinceviciene,Gert Bellen,et al. Genital tract infections in an isolated community:100 women of the príncipe island[J]. Infect Dis Obstet Gynecol,2017,2017(4):1-6.
[9] Merav Strauss,Raul Colodner,Dana Sagas,et al. Detection of ureaplasma species by a semi-quantitative PCR test in urine samples:Can it predict clinical significance?[J]. Israel Medical Association Journal,2018,(20):9-13.
[10] Krunal Patel,Shauna Williams,George Guirguis,et al.Genital tract GBS and rate of histologic chorioamnionitis in patients with preterm premature rupture of membrane[J].J Matern Fetal Neonatal Med,2017,31(3):1-4.
[11] Leonardo R. Sanchez,Maria L. Breser,Gloria J. Godoy,et al. Chronic infection of the prostate by chlamydia muridarum is accompanied by local inflammation and pelvic pain development:Chlamydia chronic prostatitis[J].Prostate,2017,77(5):517-529.
[12] Miller S, Krumins T, Zhou H, et al. Ertugliflozin and sitagliptin co-initiation in patients with type 2 diabetes:The VERTIS SITA randomized study[J]. 2018,9(1):253-268.
