Study and observation of ultrasound on hemorheology of continuous renal replacement therapy in ICU
2020-07-31LeiWangDaWeiWangNaYuanQinQinMaZhiFeiQiaoAiHongJiaShuXiaGao
Lei Wang, Da-Wei Wang, Na Yuan, Qin-Qin Ma, Zhi-Fei Qiao, Ai-Hong Jia, Shu-Xia Gao
1. Department of ICU, the First Affiliated Hospital of Hebei North University
2. Department of ICU, Zhangjiakou First Hospital, Zhangjiakou, Hebei 075000, China
Keywords:Acute kidney injury Continuous renal replacement therapy Tricuspid annular plane systolic excursion Kidney perfusion Renal aortic resistance index
ABSTRACT Objective: To observe the influence of bedside ultrasound on Hemodynamics of Continuous Renal Replacement Therapy,and explore the clinical value of bedside ultrasound technique in acute kidney injury (AKI) Patients with continuous renal replacement therapy (CRRT) and capacity management. Methods 311 cases of AKI patients with CRRT were divided randomly into Observe group and Control group. the observe group was used bedside ultrasound technique, by monitoring tricuspid annular plane systolic excursion (TAPSE), internal diameter of inferior vena cava (IVC), respiratory variation index of the inferior vena cava internal diameter (RVI) and left vertical Tei index changes. Meanwhile, each parameter change was mediated by ultrasound detection from before, to 30min, 6h, 12h, 36h, 48h after of CRRT to sustain liquid balance in observe group, however, central venous pressure (CVP) change was modulated in control group. The difference of kidney length in pre-CRRT were examined to exclude, and of renal aortic diameter, renal resistance index (RRI)and renal blood flow in post-48h of CRRT were compared in two groups. Results Renal length, Renal parenchyma thickness and Echo strength of renal parenchyma weren’t different statistically in pre-CRRT of two groups(P>0.05). In observe group, the RVI level was started to increase significantly and IVC internal diameter to decrease at 6h, which would tend to stable at 36h(F=27.746 and 15.446 respectively); the TAPSE level was gradual ascending and Tei index was descending at 12h with a stable tendency at 24h of CRRT(F=36.213 and 17.127 respectively), and there was difference statistical among time of obvious change in TAPSE, IVC internal diameter, RVI and Tei index(P<0.05); In control group, there was no difference statistical among each time in CVP(F=2.189, P>0.05). Compared with control group, renal aortic diameter and renal blood flow were increased significantly(t=2.356 and 2.075), RRI was decreased obviously in observe group(t=2.244), which was different in statistics (P<0.05). Conclusion the application of bedside ultrasound technique in AKI patient’s capacity management with CRRT was more effective and evaluated the kidney perfusion.
1. Introduction
Acute kidney injury(AKI) is a clinical syndrome of a rapid and persistent decreasing of the glomerular filtration rate and accumulation of metabolism, is the major causes of death in critically ill patients[1]. Continuous renal replacement therapy(CRRT) is used to treat of critically ill patients with AKI, and, the common complication of CRRT is hemodynamics instability[2, 3]. In order to reduce the volume load of patients as soon as possible, doctors often increase the intensity of ultrafiltration, which easily leads to reduction of effective circulation blood volume, resulting in serious volume imbalance, then may lead to the decrease of renal perfusion, resulting in the“second strike”of kidney injury. Nowadays, Bedside ultrasound is widely used in Intensive care unit(ICU),which not only quickly judge the effective blood volume and heart function, but also the perfusion of kidney and other important organs[4]. Our study is to detect the volume management of CRRT in ICU through bedside ultrasound, and the renal perfusion of blood flow in target organs with a good effect.
2. Information and methods
2.1 General data
311 cases of AKI III stage patients with CRRT were selected in the ICU of the first affiliated hospital of the Hebei North University and the first hospital of Zhang Jiakou City from 2015-11-01 to 2018-11-01. Admission criteria: more than 300% of the base creatinine or≥354µmol/L and ≥ 44.2µmol/L in 48h of AKI, <0.3ml/(kg.h) of urine volume is lasted for more than 24h or without urine for 12h. Exclusion criteria: patients complicated with cardiopulmonary resuscitation, mechanical ventilation, pulmonary hypertension, severe valvular disease, malignant arrhythmia and advanced malignant tumor. Observe group and Control group were randomly divided, age 34-81years, median age 58 years. The observe group is 164 cases, age 39-81 years, median age 59 years, male 88 cases and female 76 cases; acute physiology and chronic health evaluation Ⅱ score(APACHEⅡ) is (19.291±2.278);Cardiac insufficiency with acute aggravation 55 cases, acute glomerulonephritis 40 cases, severe pancreatitis 19 cases, brain injury and secondary infection 23 cases, crush syndrome 12 cases, obstetric severe patients 7 cases, drug intoxication 8 cases. The Control group 147cases, age 34-76 years, median age 57 years, man 80 cases and female 67 cases; APACHE II score is (19.168±1.883); Cardiac insufficiency with acute aggravation 46 cases, acute glomerulonephritis 30 cases, severe pancreatitis 24 cases, brain injury and secondary infection 21 cases, crush syndrome 9 cases, obstetric severe patients 10 cases, drug intoxication 7 cases. CRRT treatment was operated and ultrasound was applied to detect the Renal length, Renal parenchyma thickness and Echo strength of renal parenchyma in pre-CRRT of two groups. Our study was accorded with medical ethics standards, approved by the hospital’s ethics committee and received informed consent from the patient’s family.
2.2 Methods
A double-lumen dialysis catheter was inserted into the right femoral vein under local anesthesia to establish cardiopulmonary bypass in 311 patients. Prismaflex bedside continuous hemofiltration system and affiliated duct filters was used: Fresenius FX80 membrane type hemofiltration with a membrane area of 1.6m2. CVVH mode was applied and the modified prescription of replacement fluid was used (General hospital of Nanjing Military Area Hospital),the replacement volume was 3000-4000ml/h, the blood flow was 130-150 ml/h, the 5% sodium bicarbonate was 150-180ml/h, the potassium chloride was whether added depending upon the outcome of electrolyte and blood gas, temperature was heated to 37℃-37.5℃; ordinary heparin was applied to anticoagulate and adjusted according to the time of activating thrombin with APTT containing at 1.5-2.5 times. CRRT was operated once a day for 10h-16h for at least 3 days. Tricuspid annular plane systolic excursion (TAPSE), Internal diameter of inferior vena cava (IVC), Respiratory variation index of the inferior vena cava internal diameter (RVI) and left ventricle Tei index was observed from pre-CRRT, to 30min, 6h, 12h, 36h, 48hof post-CRRT to sustain liquid balance in observe group, central venous pressure (CVP) change was modulated in control group. The difference of renal aortic diameter, renal resistance index (RRI) and renal blood flow in post-48h of CRRT were compared in two groups.

Table 1 the difference of Renal length, Renal parenchyma thickness and Echo strength of renal parenchyma in pre-CRRT of two groups
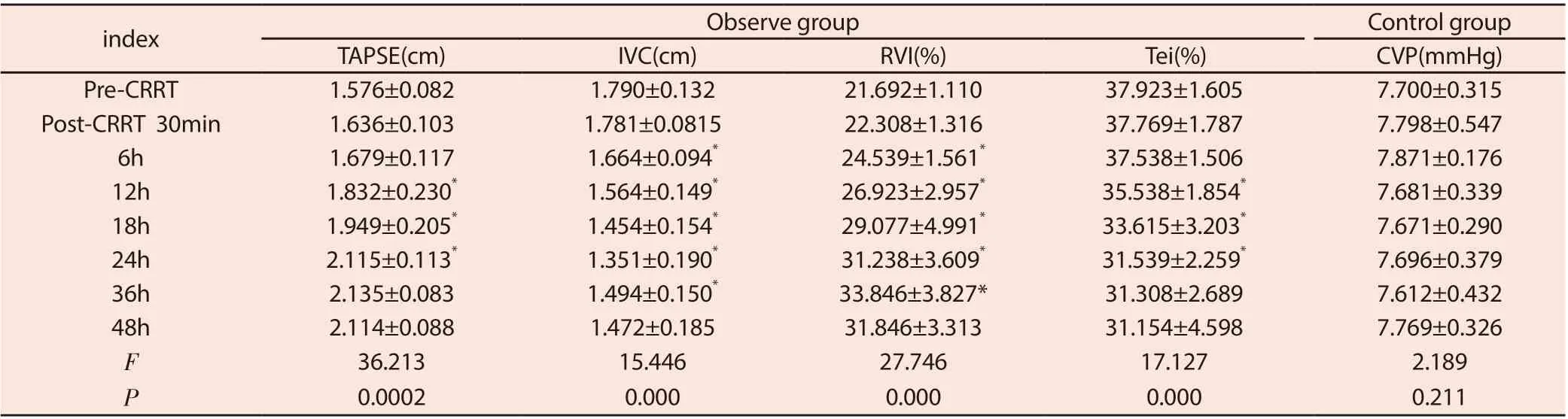
Table 2 Change of TAPSE, RVI, IVC, Tei index and CVP in each time of CRRT
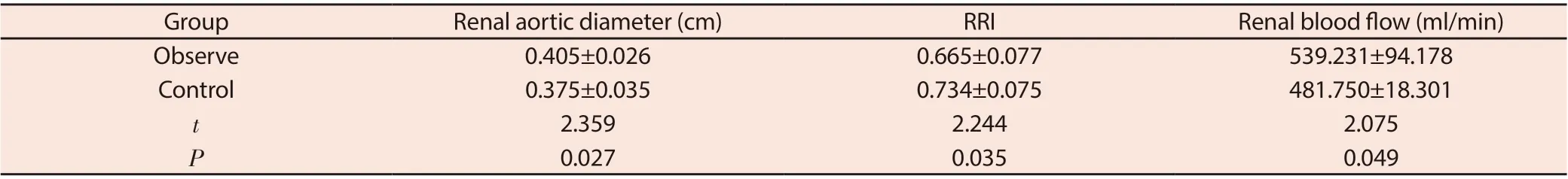
Table 3 Comparison of Renal aortic diameter, RRI and Renal blood flow in post-48 of CRRT between two groups
2.3 Monitoring index
2.3.1 CVP detection
the central catheter was placed into the internal jugular vein or subclavian vein at a depth of 12cm-15cm, and confirmed in the superior vena cava near the right atrium by bedside X ray. The median line of the forth rib was used as standard zero point when CVP is recorded where the pressure sensor should be placed and measured at the end of the gas.
2.3.2 Ultrasonic testing
the portable color Doppler ultrasound diagnostic instrument produced by American SonoSite. Having a supine position, a longitudinal section of the IVC was detected by ultrasonography in patients and the normal end of gas IVC diameter was measured at 1cm near to right atrium. At the situation of normal respiration, the maximum of IVC (IVC max) and the minimum of IVC (IVC min) was measured at the end of the exhalation and inhalation respectively, and calculated RVI, RVI= (IVC max-IVC min)/IVC max100%. The baseline was placed in free wall of right ventricular and tricuspid annulus level to measure the TAPSE. The left ventricular Tei index: isovolumic systolic time (ICT) plus isovolumic diastolic time (IRT) divided by left ventricular ejection time (ET), is that left ventricular Tei index= (ICT + IRT)/ET = (a-b) /b, a (the time between the end of the diastolic mitral flow spectrum and the beginning of the next cardiac cycle’s E peak), b(the duration of forward flow spectrum of aortic valve in systole is called ET). Kidney length and Renal parenchyma thickness in pre-CRRT were examined, and of renal aortic blood flow in post-48h of CRRT was measured, recording peak systolic velocity (PSV), end diastolic velocity (EDV), renal aortic resistance index (RRI). The formula for renal aortic blood flow Q(ml/min)=π×D2/4×Vm ean×60[D: internal diameter of renal artery]. The mean of blood speed (Vmean): adjusting the angle of sampling frame and instructing the patient to hold breath, at least three steady blood flow spectrum of Renal Aorta was examined and Vmean value was got by automatic spectrum recording function. Left and right renal aortic internal diameter: the longitudinal sections of the left and right renal arteries was measured on the short axis of the abdominal aorta, and the blood flow in the lumen was shown by CDF1, then the color flow was adjusted to fill the lumen without overflow and the image was enlarged as far as possible without distortion. the internal diameter of the renal aorta was measured at 5mm near to abdominal aorta. Echo intensity of renal parenchyma: ScnImage software was used to analyze the echo intensity of gray-scale images of patient’s kidneys. The above operation is measured three times by the same operator and the average value is the final result.
2.4 Statistical methods
SPSS19.0 software was used to completed. Measurement data and counting data were shown withx±s and % separately. Two-to-two comparisons of measurement data was performed by t-test, singlefactor repeated measures and intergroup comparison was applied by variance analysis. P<0.05 was statistically significant difference.
3. Results
3.1 The difference of Renal length, Renal parenchyma thickness and Echo strength of renal parenchyma in pre-CRRT of two groups. (table 1)
The kidney length, Renal parenchyma thickness and Echo strength of renal parenchyma in pre-CRRT of two groups weren’t different in statistics(P>0.05), indicating that two groups being coparable.
3.2 The measurement change of every times of TAPSE, RVI, IVC, Tei index and CVP in bedside ultrasound. (Table 2)
In observe group, the level of RVI was significantly increasing and IVC was gradually decreasing at 6h, and was stable at 36h of post-CRRT (F=27.746 and 15.446 respectively); otherwise, the level of TAPSE was steadily ascending and the left ventricular Tei index was descending at 12h, and was tended to stable at 24h of post-CRRT (F=36.213 and 17.127 separately), and there was difference statistical among time of obvious change in TAPSE, IVC internal diameter, RVI and Tei index(P<0.05); In control group, there was no difference statistical among each time in CVP(F=2.189, P>0.05).
3.3 Comparison of Renal aortic diameter, RRI and Renal blood flow in post-48 of CRRT between two groups. (Table 3)
The Post-CRRT of 311 patients, the level of Renal aortic diameter and Renal blood flow of observe group was more than control group (t=2.356 and 2.075), the level of RRI in observe group was less than control group (t=2.244), which has a difference in statistics (P<0.05).
4. Discussion
Most of AKI patients in ICU exist the other diseases and have a unstable in vital signs, therefore, CRRT is the first choice of treatment[5].CRRT was used to relieve water load and reduce inflammation by improving the metabolic disorder of acid and base. In the treatment of CRRT, the fluid management is the most important, excessive or insufficient dehydration could increase the mortality in AKI patients[6].
The CVP level, a measure of ventricular volume, is often used to guide fluid balance during CRRT[7]. Yet, CVP isn’t accurately reflect the real volume state of AKI patients when it is influenced by various factors such as heart, chest pressure and vasoactive drugs, only when CVP<2mmHg or >12mmHg has clinical value[8]. We found the CVP level was fluctuated between 7 mmHg-8 mmHg in CRRT treatment and an effective volume state may not be detected. Bedside ultrasound can monitor blood volume and important organ function to ensure cardiac output, blood pressure and further renal perfusion[9]. Due to the early stage of AKI with enlargement of kidney volume and renal parenchyma thickeness, the kidney length, Renal parenchyma thickness, RRI and et al were measured by ultrasound have a important reference value for assessing the degree of kidney damage and guiding the treatment [10]. In our study, The kidney length, Renal parenchyma thickness and Echo strength of renal parenchyma in pre-CRRT of two groups weren’t different in statistics, in order to exclud the various interference factors affecting chronic kidney injury.
Patients with kidney failure usually have less urine, greater water and sodium retention may increased pre-load of heart. According to Frank-starling’s law, the heart has an ability of heterometric regulation, only in the rising phase of the curve, pre-load of heart and cardiac output are increased; otherwise, in the plateau phase of the curve, pre-load of heart is increased, but the contractility of myocardium is weakened and cardiac output is reduced; however, if the ultrafiltration volume is over, pre-load of heart is insufficient, could also lead to decrease in cardiac output[11]. Cumulated studies show that bedside ultrasound is also an effective tool for monitoring vascular volume status, which can significantly reduce kidney injury of AKI patients by detecting IVC level to guide the balance of body volume, resulting in longer survival and better kidney protection[12, 13]. But the measurement of IVC is susceptible to spontaneous breathing or mechanical ventilation, which is hard to value accurately liquid volum. Based on the principle of cardiopulmonary interaction, the superiority of the volume reactivity indices reported such as RVI is used to detect the volume[14]. In our study, the change of IVC internal diameter and RVI were observed and found IVC was decreasing and RVI was increasing at 6h, continuous dynamic change to reach the steady state at 36h of post-CRRT, considering IVC and RVI may monitoring the state of capacity more sensitively, alleviating “negative balance” via increasing the amount of dehydration, and in order to make the cardiac function curve gradually transition from the plateau stage to the ascending stage, meanwhile, improving the right heart function and providing the guarantee of the volume power. It is reported that TAPSE is used to value the right ventricular contractile function and is an important parameter of reflecting the change of right ventricular myocardial fiber in longitudinal axis mechanics[15]. We showed the TAPSE<16mm in pre-CRRT and there was existing the decrease of right ventricular myocardial function, conforming to the recommendations of the American and European Society of echocardiograms[16]. During the CRRT treatment, TAPSE was gradually and in particular obviously ascending at 12h and was up to stable at 24h of post-CRRT, which suggested TAPSE was detected by ultrasound to slightly adjust the amount of dehydration and improve the right ventricular systolic function. In addition, the Tei index is elevated when ventricular systolic dysfunction, also as a indicator to assess the ventricular systolic function[17]. In the same way, we observed the change of left ventricular Tei index monitored and the Tei index could be directed the management and control of CRRT volume with a left systolic function improved. Therefore, considering the volume overload is common phenomenon and effective circulating blood volume is relatively inadequate of AKI patients. In the course of CRRT dehydration treatment, the pattern of continuous, gentle and slow adjusting is to avoid the insufficiency of vital organs and tissues. The method of adjusting CRRT dehydration was as follows: according to the changes of the above indexes in observe group, the dehydration was added by 100ml/h in each time(30min、6h、12h、18h、24h) on the basis of the original “negative balance” dehydration, if the above-mentioned factors were close to or reach the normal value at the corresponding time, the total dehydration amount would be adjusted to “zero balance” , and didn’t up to the normal value at 24h of post-CRRT, 50ml/h was added to the original dehydration at 24 h, 36h, 48 h until the above factors trended to normal and dehydration amount was adjusted to “zero balance”. In Control group, only when CVP value is more than 12mmHg did the dehydration added by 100ml/h on the basis of original “negative balance” dehydration. By means of monitoring the above indicators, our study was not only to avoid over CVP level to aggravate postload of kidney, and also pre-load of heart was improved and left and right heart function was coordinated, the heart output was added to increase the renal perfusion.
how to evaluate renal perfusion, the International Society of Nephrology’s “0by25” initiative on acute kidney injury proposes color Doppler flow imaging as an indicator of renal blood flow, RRI is an effective index to assess renal function injury, which can directly reflect the resistance of renal vessels, and has a good evaluation effect on the ability of renal blood perfusion and the prognosis of AKI patients[18, 19]. Anile showed that the normal of RRI value is less than 0.7, when RRI is more than 0.7 indicating there being a kidney dysfunction and blood flow decreased of kidney[20].
At 48h of Post-CRRT, the level of Renal aortic diameter and Renal blood flow of observe group was more than control group, the level of RRI in observe group was less than control group. RRI is less than 0.7, suggested that IVC, RVI, TAPSE and Left ventricular Tei index were detected had a guiding effect during CRRT volume arrangement,the kidney injury can be improved in a short time compared with CVP. Of course, our study has certain limitation, first of all, study is a observation study, not only a limited number of samples, in addition to there are many heart factors evaluated by ultrasound and a few factors were selected would to be further applied and studied in the clinical work.
Above all, the application of IVC, RVI, TAPSE and Left ventricular Tei index in the CRRT treatment of AKI is more accurately guide the volume management of critical patients than CVP. The study returns to the nature of volume management, improving volume load while paying attention to cardiac function to ensure normal renal perfusion.
杂志排行
Journal of Hainan Medical College的其它文章
- The potential mechanism of prevention and treatment of COVID-19 by shufeng jiedu capsule was studied based on network pharmacology
- A case of recurrent PMT caused by poor atrial pacing
- Experience of Professor Shao Mingxi in treating knee osteoarthritis based on "Bin Si Xue" acupuncture
- Meta analysis of Masquelet technology and Llizarov technology in the treatment of infectious bone defects
- Acupuncture for post-stroke dysphagia: An overview of systematic reviews
- Effect of TGIF1 expression on epithelial cadherin and Twist1 protein expression in breast cancer cells
