Target-based approach for osteoarthritis treatment
2020-07-23
Antonio M Tieppo,Cyro S de Almeida Jr,Department of Physiatrics,Faculdade de Ciências Médicas da Santa Casa de São Paulo,São Paulo,SP 01221-020,Brazil
Gustavo C de Campos,Department of Orthopedics and Traumatology,Hospital de Clínicas da Universidade Estadual de Campinas,Campinas,SP 13083-887,Brazil
Paulo C Hamdan,Departamento de Medicina Esportiva,Universidade Federal do Rio de Janeiro,Rio de Janeiro,RJ 21941-901,Brazil
Wilson M Alves,Ortopedia,Pontifícia Universidade Católica de Campinas,Campinas,SP 13087-571,Brazil
Márcia U de Rezende,Instituto de Ortopedia e Traumatologia da Faculdade de Medicina da Universidade de São Paulo,São Paulo,SP 05403-010,Brazil
Abstract
Key words: Osteoarthritis; Knee osteoarthritis; Cartilage; Treatment; Target; Pain
INTRODUCTION
Knee osteoarthritis (KOA) is a heterogeneous disease at the clinical,physiologic,anatomic,and molecular levels[1]with progressive and degenerative synovial impairment that evolves from an asymptomatic phase (molecular and cellular damage level) to symptomatic phase (multitissue lesions) with joint pain,stiffness,and functional disability[2].KOA affects not only the cartilage but the entire joint[1].There is imbalance in joint tissues anabolism/catabolism with articular cartilage breakdown,subchondral bone remodeling,and synovial and periarticular soft tissue inflammation with joint capsule hypertrophy[3].
It is a heavy burden for society because it leads to a great loss of function and quality of life in affected individuals and generates enormous costs[4].The latest update from the Global Burden of Disease study estimates that 242 million people worldwide live with symptoms and limitations related to OA of the knees or hips[4].
Despite the vast number of research studies,there is still no definitive treatment for OA.There are currently several guidelines with recommendations on the various treatment modalities for OA based on the medical literature[5,6].Most of them recommend a combination of treatment modalities including non-pharmacological and pharmacological therapies,such as information/education,weight loss,exercise programs,analgesics,nonsteroidal anti-inflammatory drugs,and symptomatic slowacting drugs[5,6].
We are,however,far from a consensus on the best form of treatment or on an effective treatment recommendation for individual patients.There are reasons for the current equivocal treatment recommendations in the face of this very serious health problem.The greatest of these,undoubtedly,is the great complexity of the factors involved in the development and progression of KOA[7]and the complex pathophysiology including mechanical,inflammatory,metabolic,post-traumatic,molecular,genetic,and psychological changes[7].Similarly,there is a large variation among individuals in relation to disease trajectory with some patients evolving rapidly,while others remain stable for long periods of time[8].This has led to attempts to group patients with common disease characteristics or similar treatment responses into subgroups called OA phenotypes[8].
Several studies have proposed different OA phenotypes based on clinical,laboratory,or imaging findings[8].Correlation of different phenotypes to different patterns of response to treatment creates the possibility of developing specific treatments for certain groups of patients,theoretically allowing better treatment efficacy[8].However,in practice we still find totally different responses and evolutions in individuals belonging to the same phenotype.This is because despite grouping patients with similar characteristics,the great variety and propensity of factors involved in the pathophysiology of each individual makes it difficult to achieve success with the same treatment for different individuals[9].Additionally,the same individual may have characteristics common to several phenotypes,such as an obese elder who has had a meniscectomy in the past.Thus,classification by phenotypes,despite being an advance,is not sufficient.We must go further addressing specific features of these phenotypes,i.e.targets.The purpose of this publication is to introduce a novel perspective for OA treatment,which can rationalize its management and also contribute to enhance future clinical trials.
TREATMENT MODALITIES: CURRENT OA TREATMENT
Current guidelines propose recommendations regarding several treatment modalities[5,6].For example,the use of valgus insoles or duloxetine is a treatment of osteoarthritis.However,an OA patient with neutral alignment will not benefit from valgus insoles.Similarly,a patient without chronic and neuropathic pain will not benefit from duloxetine.Therefore,a valgus insole is not a treatment for osteoarthritis but for varus malalignment; and duloxetine is not a treatment for osteoarthritis but for chronic pain.In this context,we need to reverse the rational paradigm.Rather than treating OA as a single disease,we propose a fragmented look at each of the many different factors involved in the genesis and evolution of OA to which we will name the targets.Therefore,we propose not the treatment of OAper sebut the management of an individual set of targets to achieve personalized OA management.We believe that,paradoxically,by fragmenting the view of the disease we will be able to treat our patients more holistically in an individualized way.
THERAPEUTIC TARGETS: WHAT THEY ARE AND HOW TO TREAT THEM
The complexity of mechanical,inflammatory,metabolic,cellular,molecular,genetic,and psychological factors is precisely what makes it difficult to classify patients into isolated groups/phenotypes given the infinite possibilities of combinations and interactions among these factors (Figure1).By directly and exclusively considering each factor,the variability of responses narrows.The following are the most commonly encountered targets in individuals with OA.The management possibilities of these targets are also briefly discussed.
Age
Age is undoubtedly the most important factor because OA is rare under 40 years of age and extremely frequent over 65 years of age[4].The age factor,although it can be considered nonmodifiable,can be “treated” through a healthy lifestyle with regular practice of moderate exercise[10],adequate diet[11],and healthy attitudes such as adequate sleep and respect for the circadian cycle.These recommendations have been shown to reduce the senescence (cellular aging) of chondrocytes[7].
Obesity
Obesity is another key factor in the development of OA,both due to the mechanical disturbance that being overweight causes on load-bearing joints and to the inflammatory disorder caused by the excessive production of inflammatory cytokines(adipokines)[12].The obesity target should be addressed with diet,weight loss,and in more extreme cases bariatric surgery[13].
Metabolic syndrome
Metabolic syndrome,of which obesity is a part,also exerts a negative influence on OA[14].Systemic arterial hypertensionviasubchondral ischemia can compromise the articular cartilage and cause bone remodeling[15].Dyslipidemia can lead to the deposition of lipids in chondrocytes,myocytes,and hepatocytes,which deregulates their metabolism[15].Concomitantly,increased production of free fatty acids signals greater expression of nuclear factor kappa beta and inflammasome activation,which will lead to intense production of proinflammatory cytokines,such as interleukin 1 beta,interleukin 18,and tumor necrosis factor alpha.This will increase inflammatory status with predominance of catabolism over anabolism on cartilage,synovial tissue,and subchondral bone[15].Hyperglycemia leads to increased production of glycation end products and oxidative stress leveraging persistent low-grade systemic inflammation contributing to a toxic environment that will exacerbate OA[15].Therefore,managing these targets is fundamental.
Sedentarism
The relationship between the regular practice of moderate exercise and improvement in OA symptoms is well established[10].The main treatment guidelines place exercise as a central treatment for all OA patients[5,6].Physiological and moderate intensity movements are fundamental for normal cartilage metabolism and consequently for its maintenance[10,16].
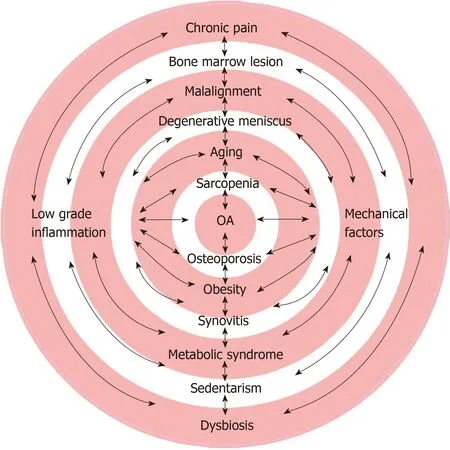
Figure1 Osteoarthritis multifactorial determinants and multitarget approaches: Combinations and interactions among these many factors.OA: Osteoarthritis.
Degenerative meniscal lesions
Degenerative meniscal lesions are frequent in OA and even in knees with no radiographic signs of the disease can be considered an initial finding of OA rather than an entity of their own[17].Degenerative meniscal lesions bring symptoms and disability and require treatment.Treatment should not be surgical even in specific cases of mechanical symptoms[17].Currently there is evidence of successful control of this target through intra-articular corticosteroid injections or hyaluronic acid injections[18].
Limb malalignment
Poorly aligned knees have an increased risk for OA and therefore a greater risk for disease progression than knees with neutral alignment[19].Knees with varus alignment have a four-fold increase in the risk of progression to OA in the medial compartment,and those with valgus alignment have approximately five times the risk of progression to lateral OA[20].The association of malalignment with the size and progression of regions with bone edema as well as with accelerated cartilage loss have been demonstrated[21].This target can be nonsurgically treated through the use of orthotics or insoles[22].
Bone marrow lesions
The presence of bone marrow lesions usually means a focal overload on the joint with microdamage of the trabecular bone.Subsequently,this leads to a vicious cycle of subchondral bone attrition,attempts at repair,pain,and progressive deformity[23].It is a predictor of unfavorable disease evolution in that compartment[24].Bone marrow lesions should also be considered a therapeutic target because they are often symptomatic and can be treated by overload reduction with the use of a cane,orthoses,body weight control,muscle rebalancing,bisphosphonates,and even surgery[25].
Chronic low-grade inflammation
In patients with OA,a low inflammatory state is present and is detectable both locally and systemically[26].Endogenous molecules called alarmins may be released into joint space after local cell stress or damage,(e.g.,cartilage matrix fragments),activating inflammasome platform and/or nuclear factor kappa beta,thus leading to joint sterile inflammation and triggering cell joint senescence[27].Chondrocytes and synovial cells(macrophages and fibroblasts) produce increased levels of inflammatory cytokines,chemokines,and lipid mediators into the synovial fluid,which in turn decreases the synthesis of collagen,aggrecans,and proteoglycans and increases catabolic mediators such as collagenases,metalloproteinases and alarmins[27].
Environmental factors,lifestyle[28],epigenomic,genomic[29],and microbiome[11]studies have been focused on clarifying molecular mechanisms of low-grade inflammation to support regulatory actions so that the expression,transcription,and translation of enzymes and structural proteins of the joints can remain at levels of homeostasis.Metabolomics is a promising field for chronic inflammation investigation[1].
Chronic low-grade inflammation plays a central role in OA pathogenesis.Apart from some promising disease modifying drugs[30],we can manage it with improvements in nutrition,rebalance of intestinal microbiome,gut health[11],restful sleep[31],and adequate physical activities[16].
Synovitis
Synovitis occurs even in the early stages of OA and may be subclinical[32].Unlike rheumatoid arthritis,synovial inflammation in OA is usually found near areas with pathologically damaged bone and cartilage[32].This hyperactive synovium can release proteinases and cytokines capable of accelerating joint destruction,thus being an important therapeutic target[32].Special attention should be given to episodes of acute synovitis,or “flares,” which are associated with the acute worsening of pain and accompanied by joint effusion usually after joint overload.In these cases,the best treatment is certainly effusion drainage followed by intra-articular corticosteroid injection[33].
Pain
Pain is a common therapeutic target for many individuals with OA.However,acute pain,which can be treated with analgesics and anti-inflammatories,must be distinguished from chronic pain,which can be treated with drugs with different mechanisms of action[34].Another aspect of this therapeutic target is pain perception.Psychological characteristics such as pain catastrophizing and depressive disorders can be addressed and treated with psychotherapy[35].Conduction disorders or hypersensitization (such as regional complex pain) also require specific treatment[36].
Other targets
Habits such as smoking and drinking can also be considered targets to be addressed[37].Other situations such as hyperuricemia,hypovitaminosis,dysbiosis,and nutritional deficiencies can also be valued and treated[11].There are large numbers of targets already identified in the medical literature and certainly many more will still be discovered.The ways to address each of the targets will also be developed and improved.
DISCUSSION: IMPLICATIONS FOR FUTURE STUDIES
There is a great deal of difficulty in obtaining convincing conclusions from clinical trials as they are currently conducted.The focus on therapeutic targets and not on OA disease could provide more homogenous groups to be compared and studied,which would boost findings.For example,McAlindonet al[38]analyzed 140 patients with KOA comparing the use of triamcinolone infiltrationversusa saline injection for a period of 2 years.They reported no difference in symptoms between groups but a greater cartilage volume loss in the group that received the triamcinolone injection.The authors concluded that the findings did not support the use of triamcinolone infiltration in patients with KOA[38].However,a large number of studies in the literature show corticosteroid injection is an effective tool for the treatment of flares[39](a specific target) but unsuitable for long-term treatment of general KOA.
The same reasoning holds for the conclusions (or lack thereof) of the current guidelines[5,6].The focus of OA pathology as a whole is the current method of analysis.But the population in which treatments are being studied is usually too heterogeneous.Instead we suggest that the efficacy of a given drug,the use of orthoses,or a given infiltration should be analyzed in the context of specific targets as discussed in this paper.
CONCLUSION
There is still no ideal treatment for OA.Much difficulty arises from the treatment of it as a single disease or as groups of patients (phenotypes),which despite some common characteristics are still very different from each other.Grouping individuals according to therapeutic targets and treating them based on these targets may bring progress in outcomes.We suggest that future studies should focus on specific targets rather than focus on OA general treatment.