Correlation between myocardial infarction activity assessed by cardiac magnetic resonance imaging and the evolution of cardiac function after PCI
2020-07-10JiangJunQinHongXiuXiaoShanGaoZhiWeiLiQunQinMingLiuYiNanChen
Jiang-Jun Qin, Hong-Xiu Xiao, Shan Gao, Zhi-Wei Li, Qun Qin, Ming Liu, Yi-Nan Chen
1. Department of radiology, Third people’s Hospital of Hainan Province, Sanya, 572000
2. Hainan Medical University,Haikou,571199
3. Department of Ultrasound, Sanya Maternal and Child Health Hospital, Sanya, 572000
Keywords:Myocardial infarction Cardiac magnetic resonance imaging Myocardial activity Cardiac function
ABSTRACT Objective: To investigate the correlation of cardiac magnetic resonance imaging (MRI) in the assessment of myocardial activity in patients with myocardial infarction and the outcome of cardiac function after PCI. Methods: 30 patients with myocardial infarction (MI) who had complete clinical and imaging data from July 2016 to December 2018 after PCI were analyzed retrospectively. MR and echocardiogram were performed before and 6 months after PCI, and the parameters related to left ventricular function were measured by postprocessing software of MRI workstation. The left ventricular transmural degree of CMR late gadolinium enhancement was compared with the left ventricular wall motion degree of 6-month echocardiography as a standard to judge the viable myocardium. Result: There were 193 left ventricular segmental abnormalities in 30 cases, including 121 viable myocardium and 72 non viable myocardium in CMR-LGE before operation. Six months after PCI, echocardiography showed that 125 of 193 abnormal segments of left ventricle detected by CMR-LGE before PCI were viable myocardium and 68 were non viable myocaridium.The sensitivity and specificity of CMR-LGE to determinate of viable myocardium were 92.0% and 91.1% respectively. The larger the non-viable myocardial area of the left ventricular wall, the worse the recovery of wall motion ability, and there was a negative correlation between them (r=0.416, P<0.05).The first-pass perfusion time in CMR-LEG region was significantly longer than that in normal myocardial region (4.85 (+) 1.51) s and (3.79 (+) 1.73) s, respectively. The difference was statistically significant (t = 5.191, P < 0.05). Conclusion: MRI can evaluate the myocardial activity of myocardial infarction, reflect the range of viable myocardium, and provide imaging basis for clinical treatment and prognosis.
1. Introduction
Myocardial infarction (MI) is myocardial ischemic necrosis caused by persistent ischemia and hypoxia of coronary artery, which mostly occurs on the basis of coronary atherosclerotic stenosis[1].Percutaneous coronary intervention (PCI) is one of the important methods to treat MI. Previous studies have shown that when there is a salvageable myocardium (i.e. viable myocardium), PCI can increase myocardial blood perfusion and restore the myocardial function of viable myocardium. Therefore, immediate treatment of the activity of ischemic myocardium can help clinical select the best therapeutic schedule,which has great significance to improve the prognosis.
Cardiac magnetic resonance (CMR) has unique advantages such as high soft tissue resolution and spatial resolution, no radiation damage to human body, and little influence by subjective factors of operators. Especially with the emergence of many new technologies, such as mapping technology and 3D or even 4D technology, CMR technology has been increasingly applied in clinic [2].The aim of this study was to investigate the role of CMR in evaluating myocardial activity in infarction and its improvement in cardiac function after PCI, so as to provide more imaging basis for clinical practice.
2. Materials and methods
2.1 Study subjects
Patients with MI admitted to our hospital from July 2016 to December 2018 were collected, and the following conditions were excluded: 1) there were contraindications for PCI and magnetic resonance examination; 2) there were definite stages 4-5 renal insufficiency (eGFR < 30 ml/min/1.73 m); 3) old myocardial infarction with abnormal Q wave on ECG; 4) severe arrhythmia and arrhythmia; 5) patients with severe valvular disease, hypertrophic cardiomyopathy, chronic obstructive pulmonary disease and heart failure.Among the 30 cases that met the inclusion criteria, there were 17 males and 13 females, with an average age of (52.6±14.7 )years.
2.2 Inspection methods
2.2.1 CMR sequence
Siemens 1.5T Aera scanner was applied, 8-channel dedicated coil for heart, ECG gating technology and end-expiratory breath-hold scanning. The scan sequence includes:
1) FIESTA cine sequence: Bright blood sequence is selected for cine imaging, and real steady-state precession fast imaging with retrospective ECG gating is used for left ventricular two-chamber, four-chamber, outflow tract and short-axis cine scanning. Scanning parameters: TE/TR=1.5/3.5ms, FA=45 degrees, bandwidth=125Hz, Cardiac phase to Reconstruct=80, NEX=1, Matrix=224x128, FOV=38x38cm, slice thickness=8mm, Trigger delay=minimum (10ms), Acceleration=2, scanning time about 6s, local homogeneous field, ECG-gated, end-expiratory breath-hold scanning.
2) Myocardial perfusion scan: divided into two parts: first-pass perfusion and delayed perfusion of CMR: (a) first-pass perfusion: using rapid destructive gradient echo sequence (Turbo FLASH), gadolinium contrast agent 0.1 mmol/kg was injected through anterior cubital vein at 3-5 ml/s flow rate, followed by 20 ml normal saline at the same flow rate.(b) Late gadolinium enhancement (LEG): Turbo FLASH sequence was restored by ECG-gated breath-hold phasesensitive inversion, and 0.05-0.1 mmol/kg of contrast was added after the first perfusion examination at a flow rate of 2 ml/s; endexpiratory breath-hold scanning was performed 5-15 min after the contrast injection.
All patients underwent CMR examination and echocardiography before PCI, within 7 days after PCI and 6 m after PCI, in which the method and sequence of CMR scanning were the same.
2.2.2 Image analysis
Relevant parameters of left ventricular function were measured by post-processing software of MRI workstation;first-pass perfusion time with delayed enhancement area and without delayed enhancement area and myocardial area of left ventricular wall delayed enhancement area were calculated; abnormal segments of left ventricular myocardium were graded and scored by LGE image, the specific method was: 17-segment method recommended by American Heart Association (AHA. through LGE,the transmural degree was divided into five grades: 0 point, no enhancement; 1 point, 0-25% enhancement; 2 points, 26-50% enhancement; 3 points, 51-75% enhancement; 4 points, 76-100% enhancement; the existing literature showed that the LGE transmural degree <50% was the relevant criterion for judging viable myocardium [3], so the myocardial segments with LGE score of 1-2 were used as viable myocardium.The sensitivity and specificity of cardiac magnetic resonance imaging in detecting viable myocardium were calculated using improvement of left ventricular function on echocardiographic images 6 months after PCI as the gold standard for judging viable myocardium.
All images were analyzed independently by two experienced radiologists who were unaware of the clinical data, and if there were disagreements, the myocardial segment was analyzed repeatedly until consensus was reached.
2.2.3 Judgment criteria
The improvement of echocardiographic cardiac function after PCI was used as the gold standard to determine whether there was viable myocardium.Six months after PCI, echocardiography was performed to evaluate the motion of each segment of the left ventricular wall with the 16-segment method recommended by the American Society of Echocardiography: 1 point for normal motion (endocardial motion≥5 mm), 2 points for weakened motion (0≤endocardial motion≤5 mm), 3 points for no motion, and 4 points for paradoxical motion; if the wall motion improved ≥1 point after PCI compared with that before PCI, it was considered as having viable myocardium.
2.3 Statistical analysis
SPSS 23.0 software was used for analysis.The first-pass perfusion rate time of normal myocardium and delayed-enhanced myocardium was compared using independent sample t-test; the relationship between percentage of delayed-enhanced myocardial area and left ventricular motor capacity was analyzed using linear regression analysis, P < 0.05 considered that the difference was statistically significant.
3. Results
3.1 Results and correlation analysis of viable myocardium detected by CMR
A total of 193 abnormal myocardial segments were present in 30 MI patients, with at least one segment per MI patient showing delayed enhancement.The results of LGE transmural grading of abnormal myocardial segments were as follows: 52 myocardial segments with 1 point, 69 myocardial segments with 2 points (Fig. 1, 2), 44 myocardial segments with 3 points and 28 myocardial segments with 4 points (Fig. 3).A total of 121 myocardial segments with LGE score of 1-2 were identified as viable myocardium; 72 myocardial segments with LGE score of 3-4 were identified as nonviable myocardium.
The first-pass perfusion time in the delayed enhancement region (4.85 + 1.51) s was significantly longer than that in the normal myocardial region (3.79 + 1.73) s (t = 5.191, P < 0.05).Univariate regression analysis showed that the larger the delayed enhancement area of the ventricular wall, the worse the left ventricular systolic capacity, and there was a negative correlation between the two (r = 0.416, P < 0.05).

Figure 1: acute MI patients, male, 57y, CMR examination showed that the signal of the anterior septum (segment 8) in the middle of the left ventricle increased on T2WI, and strip delayed enhancement signal shadow was seen under the endocardium of the delayed scanning position, but the range was smaller thn that of the myocardial edema area.
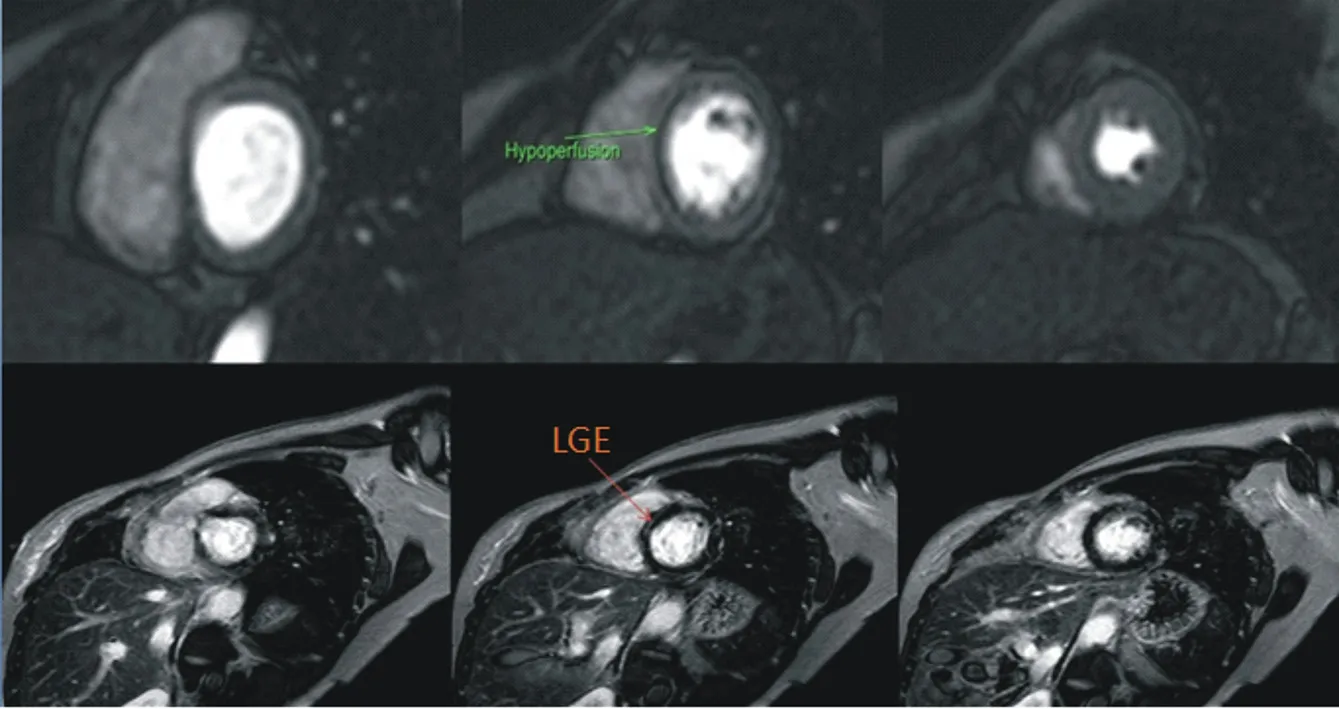
Figure 2: acute non ST elevation MI patients, female, 47y, CMR examination, perfusion imaging showed linear hypoperfusion area in the anterior septum and the inferior septum (segments 2 and 3) of the left ventricular bottom, and strip delayed enhancement signal was found in the corresponding position of delayed scanning.

Figure 3: acute MI patients, male, 39y, CMR examination showed that the left ventricle was enlarged, the signal of left ventricular myocardium was slightly less uniform on T2WI, the delayed scan showed that the front wall, the lower wall, the lower wall, the heart and the apex walls (segments 1, 4, 5, 7-17) of the left ventricular basement were extensively enhanced with multiple patchy delayed enhancement, which was subintimal and transmural.
3.2 Sensitivity and specificity of MRI-LGE for detecting viable myocardium
Six months after PCI, echocardiography was reexamined and 193 segments with abnormal wall motion were followed up, of which 125 segments had improved left ventricular function and were judged as viable myocardium; 68 segments had no significant improvement and were judged as non-viable myocardium (Table 1). Compared with gold standard echocardiography, preoperative MRILEG detected 115 viable myocardium, 10 non-viable myocardium, 62 non-viable myocardium and 6 non-viable myocardium. The sensitivity and specificity of MRI-LEG for determining viable myocardium were 92.0% (115/125) and 91.1% (62/68), respectively (Table 2).
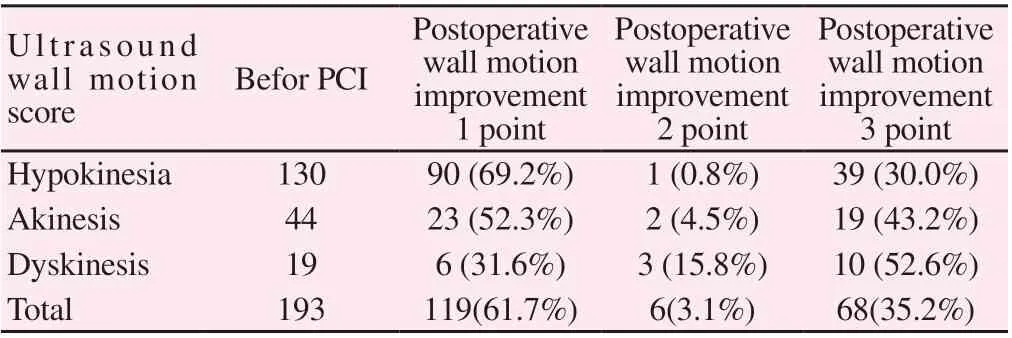
Table 1 Echocardiography to Evaluate the Wall Motion of MI Patients before and after PCI (cases (%))
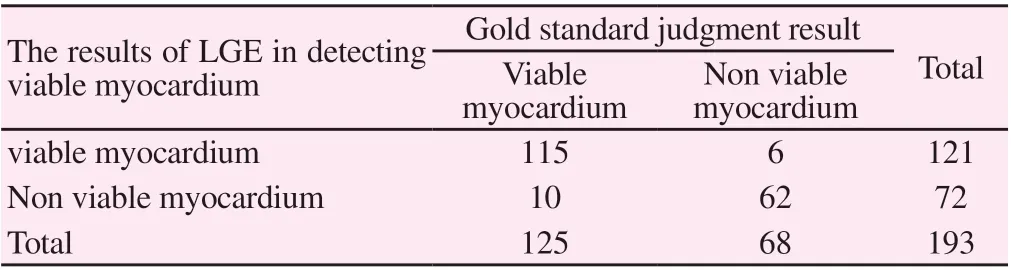
Table 2 Comparison of Viable Myocardium in 193 Segments with Abnormal Wall Motion in MI Patients Evaluated by LGE and Gold Standard
4. Discussion
Myocardial cells and nerve cells are similar to each other. Once they are necrotic, they cannot regenerate. Therefore, it is of great clinical significance for the patients with myocardial infarction to determine the activity of ischemic myocardium, the number of viable myocardium and the scope of infarct area in time, so as to select treatment methods and improve prognosis of such diseases. In patients with myocardial infarction, there is a kind of myocardial which can be saved because of temporary ischemia and loss of function, i.e. viable myocardium (including stunned myocardium and hibernating myocardium) [4]. Early and timely reperfusion treatment can restore all or part of the systolic function of the viable myocardium, so it is very important to detect the viable myocardium quickly and grasp the treatment time window accurately.
At present, there are many methods to evaluate the activity of infarcted myocardium, including radionuclide (SPECT, pet, PETCT), MSCT, ultrasound and MRI. Although radionuclide myocardial perfusion imaging has been regarded as the main classical method for the diagnosis of myocardial infarction focus [5], the spatial resolution of SPECT and PET images is relatively low, and accurate quantitative analysis is difficult, especially for the diaphragmatic heart disease focus. MSCT has high time and density resolution, especially the current energy spectrum CT[6], combined with ECG gating, can be used when the heart is relatively still (such as the end of diastole) Scan, reduce or eliminate the moving artifacts of beating heart, keep the same phase, facilitate the measurement of myocardial perfusion, so as to find the location and range of myocardial ischemia in reversible myocardial period as early as possible, analyze the hemodynamic changes in the heart or myocardial lesions, and make CT myocardial perfusion imaging show certain advantages in the evaluation of coronary artery and cardiac function, However, CT radiation has always been a concern of the academic community. PET-CT has the advantages of both pet and CT, and is regarded as the reference standard to judge the myocardial activity. However, the resolution of metabolic imaging is lower than CMR, and the cost of examination is high. Domestic hospitals at all levels have not been widely used, so it is difficult to promote. Echocardiography (especially drug loading echocardiography) can be used to observe the contractile function of abnormal myocardial segments in multi-slice and real-time dynamic way to judge the myocardial activity. Because of its advantages of safety, low price and strong repeatability, it has attracted clinical attention. However, this technique has strong operator dependence, and it can not be used to evaluate the existence of wall motion dysfunction in MI patients prospectively The existence of living myocardium has certain limitations [7,8].
CMR has good soft tissue and spatial resolution, and has no radiation damage to human body. It can comprehensively detect myocardial activity by using morphology, dynamic film, contrast enhancement and other technologies, so as to clearly show the transmural extent of myocardial infarction between endocardium and epicardium and the range of myocardial infarction area that can save myocardium. CMR has important clinical application value. With the development of this technology, With the continuous improvement of time resolution, it has attracted wide attention of clinicians and is one of the main methods to evaluate the viable myocardium [9,10].
It has been shown by some scholars that the prolongation of the first myocardial perfusion time of CMR can help to detect the different stages of myocardial cell survival and whether the myocardial cells survive [11,12]. In this study, we found that the time of delayed enhancement of first pass perfusion (4.85 ± 1.51) s in myocardial infarction area was significantly longer than that of normal myocardial area (3.79 ± 1.73) s, which indicated that the speed of contrast medium flowing into myocardial infarction area was significantly slower than that of normal myocardial area, which may be related to the serious stenosis or occlusion of coronary artery and the microcirculation disturbance in myocardial infarction area or ischemic area.
The clearance rate of normal myocardium after gadolinium contrast agent injection is much faster than that of fibrosis or scar area of myocardial infarction, so there is no delayed enhancement in normal myocardium; once myocardial infarction fibrosis or scar formation occurs, the clearance rate of gadolinium contrast agent is obviously slowed down, and the retention time of contrast agent in infarcted myocardium is prolonged, showing delayed enhancement. Previous studies have shown that the delayed enhancement of contrast medium at 5-20 min after injection can maximize the detection of fibrotic or scarred myocardium, so it can distinguish the salvable myocardium from the completely necrotic myocardium, which has become the reference "gold standard" for evaluating the formation of localized myocardial scarring after myocardial infarction, and has important clinical significance for the assessment of myocardial activity after myocardial infarction [13-15]. In this study, we found that the sensitivity (92.0%) and specificity (91.1%) of LGE in CMR perfusion imaging were higher in evaluating myocardial activity in patients with myocardial infarction, basically similar to the research conclusion in the literature. Our study also found that there was a negative correlation between the area of delayed enhancement of left ventricular wall and left ventricular systolic capacity, i.e. the larger the area of delayed enhancement, the less viable myocardium, the worse the recovery of left ventricular systolic capacity.
The latest research [12] found that CMR mapping quantitative technology plays an important role in quantitative evaluation of myocardial viability, which can not only reduce the impact of various artifacts (motion artifacts and subendocardial slow flow artifacts), but also accurately, rapidly and quantitatively analyze the pathological and physiological state of ischemic myocardium, with a higher diagnostic value.
In a word, with the continuous development of MRI hardware and software technology, the higher spatial-temporal resolution, the emergence of 3D technology and even 4D dynamic imaging, cardiac MRI will become an indispensable tool to diagnose heart disease and evaluate the recovery of cardiac function after coronary intervention, which can provide important imaging basis for clinical selection of MI patients' treatment plan and evaluation of PCI prognosis. The main shortcomings of this study are: (1) the sample size is small, and large sample study is needed to quantitatively evaluate the infarcted myocardium; (2) the evolution of cardiac function of 6m after PCI in this study is not completely accurate, some scholars have shown that some myocardial edema after MI can exist for a longer time, so the follow-up time for patients after PCI may need to be extended.
杂志排行
Journal of Hainan Medical College的其它文章
- Effects of virtual reality balance games combined with muscle strength training on balance function and motor ability of Parkinson's patients
- Epidemiological characteristics of 168 cases of COVID-19 in Hainan Island, tropical China: A descriptive study
- Survey and analysis of anxiety of 804 residents in Hainan during the COVID-19 epidemic
- Analysis of treatment strategies of traditional Chinese medicine for COVID-19 in tropical regions based on the pathogens of dampness and heat
- Evaluation of hepatic fibrosis parameter model and elastic modulus of liver and spleen for the diagnosis of hepatic fibrosis in chronic hepatitis b
- Effect of aripiprazole and olanzapine on the cognitive function in patients with schizophrenia
