Mid-term follow-up of one-stage posterior debridement, intertransverse process bone grafting and screw-rod system fixation for Brucella spondylitis of the lumbar spine
2020-07-10PeiNanZhangXinMingYangGuangXue
Pei-Nan Zhang, Xin-Ming Yang, Guang Xue
1. Orthopedic Department of The First Hospital Affiliated to Hebei North University, Zhangjiakou, Hebei 075000 2. Graduate Department of Hebei North University, Zhangjiakou, Hebei 075000
Keywords:Brucella spondylitis of lumbar spine Posterior debridement Intertransverse process bone grafting Screw-rod system fixation Curative effect
ABSTRACT Objective: To investigate the short-term and medium-term efficacy of one-stage posterior debridement, intertransverse process bone grafting and screw-rod system fixation in the treatment of Brucella spondylitis of the lumbar spine. Method: 156 cases of Brucella spondylitis of lumbar spine were selected and divided into experimental group (n = 80) and combined group (n = 76) according to different surgical methods. The experimental group was treated with one-stage posterior debridement, intertransverse process bone grafting and screwrod system fixation. The combined group was treated with one-stage anterior debridement and intertransverse process bone grafting combined with posterior internal fixation. The operative indexes and clinical effects were compared between the two groups. Result: The operation time, intraoperative bleeding volume and time of landing after operation in the experimental group were less than those in the combined group, with statistical significance (P<0.05). VAS score, ODI index, Cobb angle and Frankel grade of nervous function in the two groups were significantly improved after 3 months and 36 months of treatment (P<0.05), but there was no significant difference between the two groups at the same time (P>0.05). There was no significant difference in the excellent and good rate between the two groups after 3 and 36 months of treatment (P>0.05). There was no recurrence of the lesion in both groups. The intertransverse process bone graft healed and the screw-rod system was well fixed. Conclusion: One-stage posterior debridement, intertransverse process bone grafting and screw-rod system fixation for treatment of Brucella spondylitis of lumbar spine are effective, with short operation time and less trauma, which are worthy of clinical promotion.
1. Introduction
Brucella spondylitis of the lumbar spine is a kind of spine infection disease caused by Brucella. The focus is mostly in the thoracic and lumbar segments of the spine, which often causes persistent pain in the lower back and lumbar region. The spinal movement is easy to be limited, which brings great pain to the patients[1]. In the past, antibiotics were mostly used for conservative treatment, most patients could be cured by drugs, but there were many complications[2]. When the drug conservative treatment can not achieve the expected effect or combined with spinal cord and nerve root compression, surgical intervention is needed. In recent years, clinical studies have shown that focal debridement and bone graft fusion have a certain effect in surgical treatment, and combined with posterior internal fixation can further improve the prognosis of patients[3]. Based on this, this study took the patients with Brucella spondylitis of the lumbar spine as the research object, and analyzes the differences between one-stage posterior debridement, intertransverse process bone grafting, screw-rod system fixation and anterior debridement, intertransverse process bone grafting combined with posterior internal fixation. The specific analysis is as follows.
2. Data and methods
2.1 Clinical data
The data of 156 patients with Brucella spondylitis of lumbar spine were collected from January 2015 to July 2016. The patients were divided into experimental group (n = 80) and combined group (n = 76). Experimental group: 46 males and 34 females, aged 23-61 years, with an average age of (42.29 ± 3.61) years and an average course of disease of (6.89 ± 0.76) months. 69 cases involved 2 vertebrae and 11 cases involved 3 vertebrae. In the combined group, 44 males and 32 females, aged 23-60 years, with an average age of (42.08 ± 3.56) years and an average course of disease of (6.81 ± 0.72) months. 67 cases involved 2 vertebrae and 9 cases involved 3 vertebrae. With the approval of the hospital ethics committee, there was no significant difference in gender, age, average course of disease and vertebral body involvement between the two groups (P>0.05).
Inclusion criteria: ①The patients had different degrees of muscle strength decline, accompanied by low back pain, fatigue, muscle spasm, numbness and spinal activity limitation[4].②The patients met the World Health Organization diagnostic criteria for Brucella spondylitis of the lumbar spine.③All the patients were confirmed by X-ray, CT and MRI imaging, tiger red plate agglutination test, standard serum tube agglutination test and other laboratory tests. ④The lesion of vertebral body was large and the compression of spinal cord or nerve root required surgical treatment. ⑤The patient agreed to cooperate with the study and signed the informed consent.Exclusion criteria: ①Patients with serious diseases such as heart, liver and kidney.②Patients with other spinal infection.③Patients with good spinal stability, simple intervertebral space or vertebral infection, and no neurological dysfunction[5].
2.2 Method
After admission, all patients were given doxycycline, rifampicin, sulfamethoxazole and other antimicrobial treatment, requiring patients to rest in bed, supplemented by nutritional support. The patients were operated when the symptoms of poisoning and malnutrition were improved and the erythrocyte sedimentation rate was lower than 45mm/1h.
The experimental group was treated with one-stage posterior debridement, intertransverse process bone grafting and screw-rod system fixation. After tracheal intubation and general anesthesia, the spine process of the diseased vertebral body was located in prone position by C-arm fluoroscopy. The posterior approach of the spine was used as the central median incision with a length of 15-25cm. The subcutaneous and fascial layers of the skin were cut layer by layer, the vertical spine muscle and paravertebral soft tissue were separated, and the diseased spine process, articular process, lamina and the upper and lower vertebral bodies of the diseased vertebral body were exposed. Pedicle screws were inserted under fluoroscopy. Then the focus was removed under the C-arm fluoroscopy, the spinal canal was expanded and decompressed, and the abscesses, inflammatory granulomas and bone destruction foci in the spinal canal and in front of the posterior longitudinal ligament were scraped off with surgical instruments after the corresponding segment of spinal cord and nerve root of the diseased vertebral body were fully exposed. The diseased intervertebral disc, sclerotic bone and cartilage surface were removed under the intervertebral disc endoscope until the blood seeped on the bone surface. Then, the inflammatory granuloma and abscess at the anterior edge of the vertebral body were scraped off, compressed to stop bleeding, washed clean, and the clearance status of the pathological tissue was observed through the endoscope of the intervertebral disc. If there was any residual, the debridement was performed again, and the wound was washed with hydrogen peroxide. At last, the bone graft was polished and the crushed vertebrae were implanted into the bone defects between vertebrae, transverse processes and facet processes, and drainage tubes were placed to suture the incision.
The combined group was treated with one-stage anterior debridement, intertransverse process bone grafting and posterior internal fixation. First, posterior internal fixation, the method was the same as that of the experimental group. After the incision was sutured, the lateral or supine position was taken. The lesions of the patients with low thoracolumbar spine were removed through the right thoracotomy and the patients with lumbar spine through the extraperitoneal cavity. After the exposure of the diseased segments, the paravertebral and anterior vertebral abscesses and inflammatory granulomas are scraped off with surgical instruments. Then the two diseased intervertebral discs, sclerotic bone and dead bone in the vertebral body were removed, and the wounds were washed with hydrogen peroxide. The method of bone grafting was the same as that of the experimental group.
After operation, routine antibiotics were used to prevent infection, nutritional support was strengthened, primary care was given, and changes of vital signs, sensation and movement of both legs were regularly observed.
2.3 Efficacy evaluation
The operative time, intraoperative hemorrhage and time of landing after operation were recorded, and the differences of operative indexes between the two groups were compared.
After 36 months of continuous follow-up, VAS score was used to evaluate the pain relief degree of patients' waist and lower extremity [6]. ODI index was used to evaluate the ability of daily life, including ten items such as pain intensity, self-care, standing and social life, and the higher the score was, the more serious the dysfunction was [7].According to Frankel grade, nerve function was evaluated, which was divided into A, B, C, D and E. The higher the grade, the smaller the damage of nerve function[8]. The changes of VAS score, ODI index, Cobb angle and Frankel grade were compared before treatment, after 3 months and 36 months of treatment.
According to the relevant evaluation criteria of curative effect, the curative effect of patients after 3 and 36 months of treatment was evaluated, which was divided into three levels: excellent, good and bad. Excellent: the body temperature is normal, the symptoms of low back pain are completely relieved, the X-ray film shows that the spine is stable, the CT examination shows that the abscess disappears or calcification, the bone destruction focus is repaired, and the ability of daily activities is completely restored. Good: the body temperature is normal, the symptoms of low back pain are relieved by more than 50%, the X-ray film shows that the spine is stable, the CT examination shows that the abscess is reduced, the bone destruction focus is repaired, and the ability of daily activities is improved by more than 50%. Poor: the body temperature is unstable, the symptoms of low back pain are relieved by less than 50%, the X-ray film shows that the spine is instable, the CT examination shows no improvement compared with that before operation, and the ability of daily activities is improved by less than 50% [9].
X-ray films were taken regularly after operation to check the loosening, fracture and fusion of bone graft.
2.4 Statistical analysis
Spss21.0 software was used for statistical analysis. The operation time and other measurement data were expressed in the form of (mean± standard deviation). The difference was compared by t test. Count data in % form such as excellence rate, Frankel grade. And the difference was compared by chi square test or rank sum test. If P<0.05, the difference was statistically significant.
3. Results
3.1 Comparison of operative indexes between two groups
It can be seen from table 1 that the operation time, intraoperative bleeding volume and time of landing after operation in the experimental group were less than those in the combined group (P<0.05), with a statistically significant difference.

Table 1 Comparison of operative indexes between two groups
3.2 Comparison of VAS score, ODI index and Cobb angle between two groups
It can be seen from table 2 that there was no significant difference in VAS score, ODI index and Cobb angle between the two groups before treatment (P>0.05).After treatment, the above indicators of the two groups were significantly improved (P<0.05), but there was no significant difference between the two groups at the same time, and the difference was not statistically significant(P>0.05).

Table 2 Comparison of VAS score, ODI index and Cobb angle between two groups
3.3 Comparison of Frankel grade between two groups
According to table 3, there was no significant difference in Frankel grade between the two groups before treatment(P>0.05). After treatment, the Frankel grade of the two groups improved significantly (P<0.05), but there was no significant difference between the two groups at the same time point, and the difference was not statistically significant(P>0.05).

Table 3 Comparison of Frankel grade between two groups
3.4 Comparison of therapeutic effects between the two groups
After 3 and 36 months of treatment, the excellent and good rates of the experimental group were 91.25% and 100%, respectively, and those of the combined group were 90.79% and 100%, respectively. By X2test, the difference between the two groups was not statistically significant (P >0.05).
There were no complications such as recurrence, incision infection and sinus formation in the two groups. The X-ray showed that the bone graft between the transverse process healed, the screw-rod system was fixed well, and no loosening or broken nail was found.
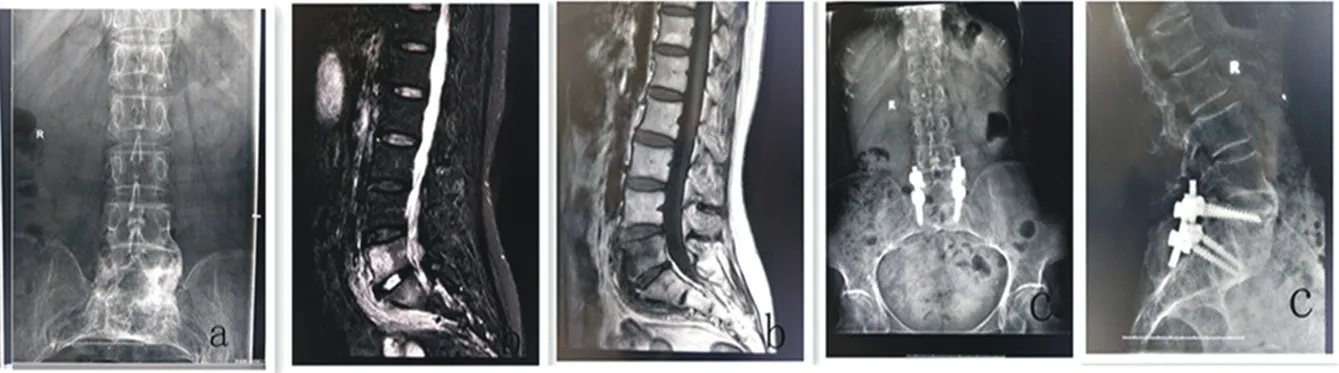
Figure 1: experimental group, male, Brucella spondylitis of the lumbar spine, a: preoperative positive X-ray film, indicating the narrowing of the intervertebral space and the unclear edge of the vertebral body; b: preoperative MRI image, indicating the inflammatory information of the vertebral body and the intervertebral body, and the destruction of the vertebral body; c: after 12 months of the operation, positive and lateral X-ray film, indicating that the recovery of the vertebral space was good, the bone graft was fully reasonable and fused, and the screw-rod system was well fixed.
4. Discussion
Brucella spondylitis of the lumbar spine is an infectious disease of the spine caused by the invasion of the normal bone tissue by the Brucella pathogen. Its main clinical manifestations are fever, joint pain and fatigue. The first choice of treatment is antibiotic conservative treatment. Doxycycline, rifampicin and other drugs used in the early treatment has a good effect[10]. In the late stage of the disease, after the abscess or granulation tissue oppresses the spinal cord, nerve root and cauda equina nerve to produce nerve injury, surgical intervention is needed[11]. Surgical treatment can accurately intervene the clinical symptoms of patients, quickly and accurately clear the focus, and immediately restore the stability of lumbar spine. The goal of surgical treatment is to completely remove the focus and restore the stability of the spine, while simple focus removal and neurodecompression cannot or immediately restore the stability of the spine. Clinical practice has proved that the combination of posterior internal fixation can further improve the prognosis of patients[12].
At present, there are two types of operation for Brucella spondylitis: posterior approach and combination of anterior and posterior approach. The anterior and posterior combined operation includes posterior internal fixation, anterior debridement and interbody bone grafting. The anterior approach has the advantages of complete focus removal and sufficient interbody bone grafting. However, the operation needs to change the patient's position. The incision of the two surgical approaches is long and the amount of bleeding during the operation is large. The operation involves the incision or stripping of transverse abdominal muscle, internal and external oblique abdominal muscle and psoas major muscle, which is difficult to operate. It has a great influence on the stability of lumbar spine, and the possibility of intraoperative hemorrhage is increased[13,14]. At the same time, the length of the posterior fixation segment will limit the range of lumbar motion and increase the possibility of vertebral degeneration in the adjacent segment.
The posterior approach operation does not need to change the position, only needs to separate the erector spine muscle and remove part of the structure of the diseased vertebral body to expose enough visual field for operation, with short operation time and small trauma[15]. The stability of the posterior spine can be maintained in the short term by the screw -rod system and in the long term by bone graft fusion. The treatment of posterior debridement, intertransverse process bone grafting and screw -rod system fixation can completely remove the lesion abscess or hyperplasia tissue, reduce the pressure of spinal canal and nerve root canal, and the posterior screw-rod system internal fixation can maintain the stability of the spine, maintain the physiological curvature and avoid the instability of the lumbar spine after operation[16]. The results of this study showed that VAS score, ODI index, Cobb angle and Frankel grade of nerve function were significantly improved in the two groups after 3 and 36 months of treatment, and there was no significant difference between the two groups at the same time. It was revealed that the two methods could alleviate the degree of low back pain, improve nerve function injury and improve the ability of daily activities. The follow-up showed that there was no recurrence in both groups, the bone graft between the transverse process healed and the screw rod system was fixed well, the excellent and good rate of treatment was good in 3 months and 36 months, indicating that the effect of both methods was significant. Compared with the combination of anterior and posterior surgery, the operation time, intraoperative bleeding volume and time of landing after operation in the experimental group were less than that in the combined group, which indicated that the operation of posterior approach had less trauma and shorter postoperative recovery time. As Brucella spondylitis of the lumbar spine is a chronic consumptive disease, most of the patients have suffered from moderate and severe malnutrition before operation, and often can not tolerate operation. Therefore, the posterior approach has a significant advantage.
To sum up, one-stage posterior debridement, intertransverse bone grafting, and screw-rod system fixation are effective in the treatment of Brucella spondylitis of lumbar spine. The operation time is short, the amount of bleeding is small, and the trauma to the patients is small, which is worth clinical promotion.
杂志排行
Journal of Hainan Medical College的其它文章
- Effect of aripiprazole and olanzapine on the cognitive function in patients with schizophrenia
- Evaluation of hepatic fibrosis parameter model and elastic modulus of liver and spleen for the diagnosis of hepatic fibrosis in chronic hepatitis b
- Effects of virtual reality balance games combined with muscle strength training on balance function and motor ability of Parkinson's patients
- Analysis of treatment strategies of traditional Chinese medicine for COVID-19 in tropical regions based on the pathogens of dampness and heat
- Survey and analysis of anxiety of 804 residents in Hainan during the COVID-19 epidemic
- Epidemiological characteristics of 168 cases of COVID-19 in Hainan Island, tropical China: A descriptive study
