Deep anterior lamellar keratoplasty versus penetrating keratoplasty in the treatment of stromal corneal dystrophies
2020-07-06
Abstract
•KEYWORDS:CDs; deep anterior lamellar keratoplasty; penetrating keratoplasty; IC3D
INTRODUCTION
Corneal dystrophies (CDs) comprise a heterogeneous set of genetically-based, gradually-progressive corneal diseases that affect both eyes and are restricted to the cornea. CD was first described by Groenouw[1]in 1890, in which two patients with corneal macular dystrophies were identified, yet a clear distinction between both types was not provided at that time. Typically, these conditions are manifested bilaterally with considerable variations in their clinical severity[2]. However, some exceptions are apparent. For instance, the majority of patients with central cloudy dystrophy of François and epithelial basement membrane dystrophy exhibit degenerative, rather than hereditary, forms of CDs[3]. Additionally, while most patients have no systemic manifestations, almost 66% of patients with Schnyder corneal dystrophy experience hypercholesterolemia[4]. The International Committee for Classification of Corneal Dystrophies (IC3D) was created to devise a current and accurate nomenclature, incorporates many aspects of the traditional definitions of corneal dystrophies with new clinical, genetic and pathologic information. A series of descriptive, evidential categories indicate that they are epithelial and sub epithelial, Bowman layer, stromal and those affecting Descemet membrane and the endothelium. The majority of the dystrophy names are identical or similar to those in the current nomenclature. However, dystrophies with a known common genetic basis, clinical and histopathologic features that are characteristic for that dystrophy. Each is assigned a level of evidence category of 1, 2, 3, or 4, depending on the amount of clinical and genetic information available. Clinically, CDs entities are classified into three groups based on the predominantly-affected anatomical location: anterior or superficial CDs (affecting the corneal epithelium or Bowman’s layer), stromal CDs (such as macular and lattice CDs), and posterior CDs (primarily affecting the corneal endothelium or Descemet’s membrane).Recently, a subset of epithelial-stromal CDs has been integrated according to the involvement of the transforming growth factor beta-induced mutations since these entities often affect multiple corneal layers[5]. For most CD types, corneal opacities are seen with varied shapes. Besides, visual loss may be developed in patients with anterior basement membrane dystrophy, Avellino CD, and macular CD[6]. Nonetheless, the clinical presentation of visual acuity may differ in various CD types, such that stable visual acuity is predominantly reported in posterior polymorphous corneal dystrophy, whereas aged individuals with macular CD may suffer blindness[2].
Notwithstanding the expanding knowledge achieved in gene sequencing as well as the remarkable diagnostic advances in ophthalmological diagnostic techniques, including confocal microscopy and high-definition optical coherence tomography[7-8], knowledge about the exact pathogenic mechanisms of CDs and their treatments is still limited. Therefore, treatment of patients with CDs requires adequate classification of the genetic, clinical, and histopathological aspects of the condition. Basically, topical medications, contact lenses, and several types of microsurgeries could be performed[9].
Keratoplasty (PK) has been traditionally performed as the mainstay transplantation approach of stromal CDs[10-11]. PK involves full-thickness replacement of the cornea and it provides good long-term outcomes with appropriate implementation of preoperative, operative and postoperative considerations for selected corneal disorders, such as Fuchs’ dystrophy[12]. However, newer lamellar surgical modalities have been widely employed for the treatment of anterior stromal or epithelial dystrophies[13]. In particular, there is an increasing trend of using deep anterior lamellar keratoplasty (DALK) for corneal stromal dystrophies since DALK mitigates the risk of endothelial rejection while preserving endothelial cell density[14]. Nonetheless, disease recurrence, interface irregularities, and separation of the Descemet’s membrane of the donor from that of the host (double anterior chamber) may develop, especially with less-experienced surgeons.
This way, whether to perform a penetrating or lamellar surgery is a matter of debate and the preferential use of either surgical technique is largely dependent on balancing the clinical benefits attained for each individual patient. This is because there is a lack of robust evidence that suggests the use of one technique over the other one. A recent Meta-analysis has shown that the visual outcomes, as demonstrated by best-corrected visual acuity (BCVA), were significantly better for DALK than those following PK procedures for the treatment of keratoconus[15]. However, to the best of our knowledge, no studies have been conducted to investigate the outcomes of both procedures in CDs. In this context, we sought to comprehensively and statistically review the efficacy and safety of DALK and PK surgical approaches in the treatment of CDs.
SUBJECTS AND METHODS
A systematic review and Meta-analysis was conducted following the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)[16]. The principles outlined in the Declaration of Helsinki (2008) are followed.
EligibilityCriteriaRandomized clinical trials (RCTs) and those employing a prospective, retrospective or case-control design were eligible. Following the histopathological confirmation of CD of any type, patients undergoing DALK or PK should be evaluated postoperatively for at least 12mo. No restrictions for sample size were applied. Comparative studies of both procedures in patients with keratoconus were excluded since it was primarily considered a separate entity from CDs as suggested by the International Classification of Corneal Dystrophies (IC3D)[5]. In addition, conference proceedings, case series, review articles, and full-texts lacking primary outcomes of interest were ineligible.
TypesofOutcomesMeasuresThe logarithm of the minimum angle of resolution (LogMAR) BCVA obtained at certain intervals following surgeries (3, 6, 12, and 24mo) represented the primary efficacy outcome. Besides, the secondary outcomes were the frequency of patients with postoperative BCVA of ≥ 6/12 and corneal endothelial cell density. Safety measures after DALK and PK included the frequencies of intraoperative complications, including Descemet’s membrane micro perforation and conversion to PK as well as postoperative complications [high intraocular pressure (IOP), cataract, interface irregularity, double anterior chamber and CD recurrence] and graft-related outcomes (graft clarity, graft rejection, endothelial rejection or graft failure).

Figure 1 Article included in both qualitative and quantitative analysis.
SearchStrategyAuthor accessed the following databases in June 2019: Embrace, PubMed, and Google Scholar. No restrictions were considered for the date of publication of screened articles. A specific search strategy was set using different combinations of subject headings and Boolean operators, such as AND andOR. Appendix demonstrates an example of the used search strategy in PubMed. Reference lists of the screened articles were thoroughly searched for additional investigations to be included based on eligibility criteria.
StudySelectionandDataCollectionSearch results were uploaded to reference organizing software (Endnote X7.0.1, Thomson Reuters, and USA) and the titles and abstracts of the obtained records were screened for inclusion by the author. Data were collated in a specifically-designed Microsoft Excel spreadsheet. These included: 1) study data: the last name of the first author, data of publication, study design, country, follow-up period; 2) patients’ data: age, gender distribution, and the number of affected eyes undergoing DALK or PK; 3) efficacy outcomes: mean values of postoperative BCVA and corneal endothelial cell density as well as the number of patients with BCVA ≥6/12; 4) safety outcomes: intraoperative and postoperative complications and graft-related outcomes at the last visit of the follow-up.
AssessmentofMethodologicalQualityThe quality of included studies was assessed using the Downs and Black quality checklist[17], which can be used for both randomized and non-randomized clinical studies. Such a scale employs 27 questions to evaluate specific quality domains, including data reporting, external and validity, and sample size power analysis. The total score of each study is 28, where four ranges indicate poor, moderate, high and excellent quality (≤14, 15-19, 20-25 and 26-28, respectively).
StatisticalAnalysisThe RevMan software (Review Manager, the Cochrane Collaboration, and Oxford, United Kingdom) was used to perform statistical analysis. When appropriate, mean means±SD values were computed from median values and interquartile ranges as described previously[18]. Continuous variables presented as means±SD, such as BCVA and corneal endothelial cell density, were expressed as weighted mean difference (WMD) and its relevant 95% confidence interval. For dichotomous variables (e.g. the frequency of patients/complications), risk ratios (RRs) and their 95%CIswere reported. Between-study heterogeneity was assessed using anI2test, where a significant heterogeneity was considered atI2> 50%. In such an instance, a random-effects model was applied. Otherwise, a fixed effects model was employed. APvalue of < 0.05 indicated statistical significance.
RESULTS
OutcomesoftheSearchProcessThe full-text versions of 7 articles were assessed for eligibility. However, one study was written in a non-English language[19], and another one entailed a comment to a relevant article[20]were excluded. Eventually, five articles were included in both qualitative and quantitative analysis (Figure 1).
StudyCharacteristicsEligibleStudies included one RCT[21]Department of Ophthalmology, Medical Faculty, Balkesir University, Balikesir, Turkey and four retrospective investigations[22-25]which were published between 2006 and 2018. Only one study was published in a European country[21]while the remaining studies were published in Asia. As for CD types, three studies assessed the outcomes of DALK and PK surgeries in patients with macular CD[21,22,25], one in lattice CD[24], and one included both lattice and macular CDs[23]. A total of 350 patients, 446 eyes (308 did PK and 138 eye did DALK) 96 patients did bilateral surgery of same procedure and neither of them did different procedure in his both eyes (59.71% males) were investigated and sample sizes ranged between 51 and 104 patients (Table 1).
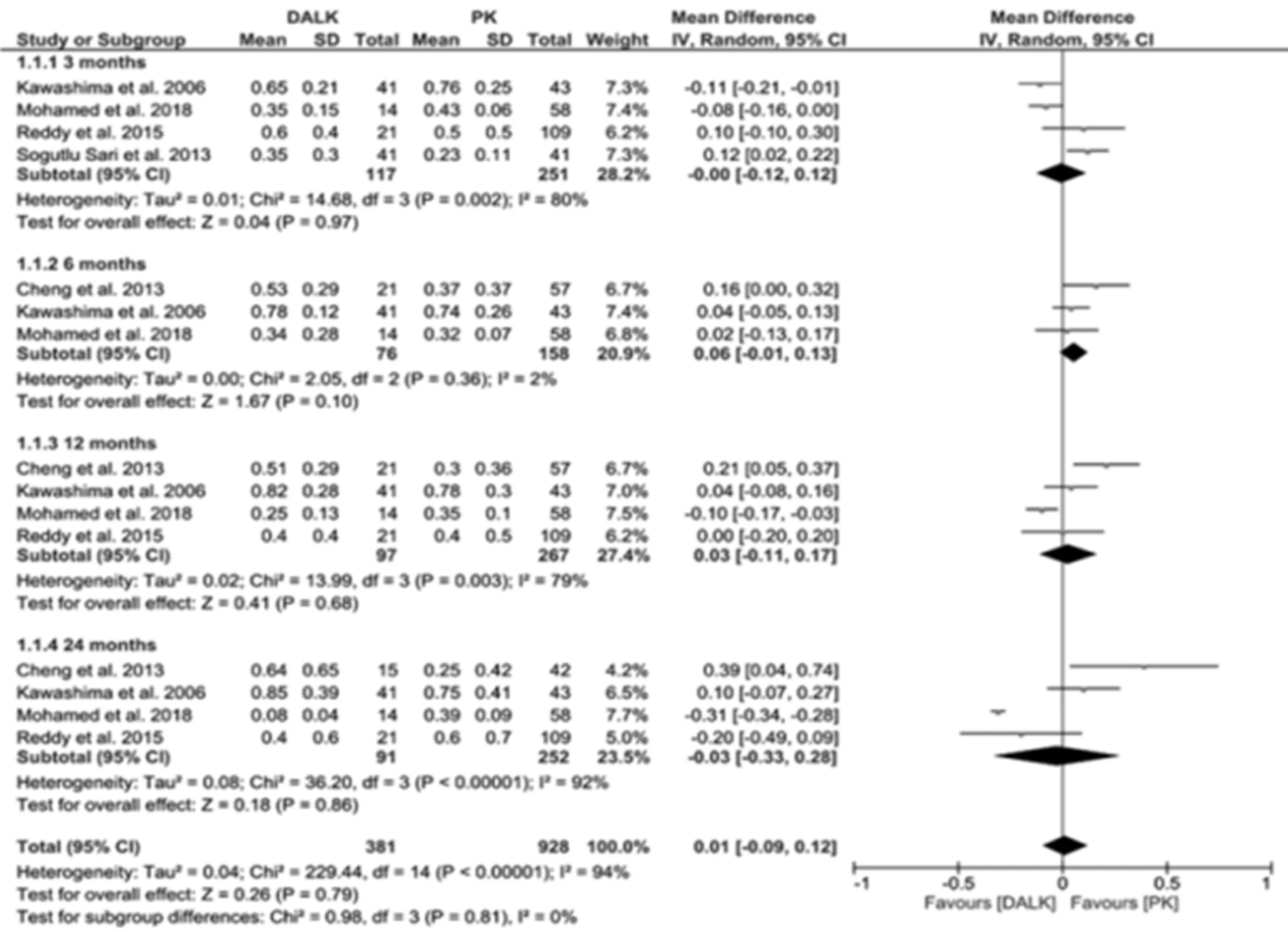
Figure 2 The pooled analysis of visual acuity outcomes.
Table 1 Characteristics of the included studies

AuthorsDesignsCountriesDBSFollow-up (mo)M/F/TDALK, aPK, aDALK, nPK, nCD typesCheng et al[22]RetrospectiveChina1768.4±54.024/27/5137.9±13.537.9±13.52157Macular CDKawashima et al[23]RetrospectiveJapan1556.8±29.357/27/8455±1555±13.04143Lattice & macular CDMohamed et al[24]RetrospectiveIndia1747.6±20.339/18/5740.7±9.745.4±12.01458Lattice CDReddy et al[25]RetrospectiveIndia1723.0±9.162/42/10430.0±11.934±11.521109Macular CDSogutlu Sari et al[21]RCTTurkey2030.5±8.827/27/5429.7±11.333.0±13.04141Macular CD
CD:Corneal dystrophy; DALK: Deep anterior lamellar keratoplasty; DBS: Downs and Black score; F: Female; M: Male; PK: Penetrating keratoplasty; T: total.
MethodologicalQualityIn general, non-randomized studies were of moderate methodological qualities (scores ranging between 15 and 17), while the included RCT was of high quality (score: 20, Table 1). The most notable limitations were the lack of description of surgical interventions in two studies[24-25], the characteristics of patients lost during follow-up were not described[22-23], and the inability to determine the suitability of prepared patients to be representative to the entire population in all studies.
VisualAcuityThe pooled analysis of visual acuity outcomes showed no significant differences in the mean LogMAR BCVA following DALK and PK surgeries when patients were followed-up over 3mo (WMD: 0.95%CI: -0.12 to 0.12,P=0.97), 6mo (WMD: 0.06, 95%CI: -0.01 to 0.13,P=0.10), 12mo (WMD: 0.03, 95%CI: -0.11 to 0.17,P=0.68), and 24mo (WMD: -0.03 95%CI: -0.33 to 0.28,P=0.86).
Similarly, weighted outcomes of three studies[21,24-25]recruiting 384 eyes (73.24% undergoing PK surgeries) showed that the proportions of eyes with postoperative BCVA ≥6/12 were 56.58% and 50.96% after DALK and PK procedures, respectively, with no statistically significant differences between both outcomes (RR=1.02, 95%CI: 0.81-1.28,P=0.89) and no significant heterogeneity between studies [I2: 39%,Heterogeneity(h): 0.19, data not shown].
CornealEndothelialDensityAlthough corneal endothelial cell count was similar after DALK and PK operations up to 12mo of follow-up, endothelial density was significantly higher 24mo after DALK procedures as compared to PK procedures (WMD: 401.62, 95%CI: 285.39-517.85,P<0.001,I2=34%,Ph=0.22) (Figure 3).
SafetyOutcomesDescemet’s membrane perforation represented the predominant intraoperative complication during DALK than PK procedures and the difference was statistically significant (RR=19.34, 95%CI: 3.95-94.66,P<0.001; Table 2).
In addition, among 193 patients in the DALK group, 15 cases (7.77%) required conversion to PK due to macro perforations in the Descemet’s membrane. Postoperatively, the DALK group experienced a double anterior chamber more frequently than those in the PK group (RR=27.14, 95%CI: 7.43-99.13,P<0.001; Table 2). No differences were reported in other complications between groups, including increased IOP, cataract, and CD recurrence.

Figure 3 Endothelial cell count was similar after DALK and PK operations up to 12mo of follow-up.
Table 2 The risks of intraoperative and postoperative complications in patients underwent DALK and PK procedures

OutcomesNo. studiesEyes, nDALKPKHeterogeneityModel (I2)PhEffect size RR (95% CI)PIntraoperativeDM microperfora-tion3103193F (0%)0.7119.34 (3.95, 94.66)<0.001PostoperativeHigh-IOP5138308F (0%)0.70.67 (0.32, 1.38)0.27DAC4117251F (0%)0.4327.14 (7.43, 99.13)<0.001Cataract497267F (0%)0.981.02 (0.49, 2.10)0.97CD recurrence396142F (0%)0.920.88 (0.46, 1.68)0.70
CD:Corneal dystrophy; DAC: Double anterior chamber; DALK: Deep anterior lamellar keratoplasty; DM: Descemet’s membrane; IOP: Intraocular pressure Ph: P for heterogeneity; PK: Penetrating keratoplasty; RR: Risk ratio.
Graft-relatedOutcomesAt the most recent visit of follow-up, the proportion of graft clarity and the risk of graft failure in patients who underwent DALK or PK were similar. However, DALK procedures were associated with a significantly lower frequency of stromal rejection and endothelial rejection when compared to PK procedures (RR=0.30, 95%CI: 0.14-0.64,P=0.002;RR=0.09, 95%CI: 0.02-0.46,P=0.004, respectively) without apparent heterogeneity between studies (Figure 4).
DISCUSSION
The adoption of novel forms of lamellar corneal transplantation techniques has introduced revolutionary changes in the past two decades. This was consistent with the endeavor to improving graft survival and minimizing surgical complications. The recent transformation from PKs to newer lamellar surgeries necessitates an adequate investigation of these procedures in terms of efficacy and safety. In this study, evidence from clinical studies for the treatment of corneal stromal dystrophies (lattice and macular CD) revealed that DALK procedures exhibited relatively similar efficacy outcomes to those implied by PK surgeries, with better corneal endothelial density achieved only over long-term periods (2y).
Indeed, these results are not surprising since DALK surgeries are more conservative. The procedure is indicated in corneal stromal dystrophies and other corneal conditions where the endothelium is still functional, such as superficial corneal scars and keratoconus[26]. It entails the fixation of the corneal button of the donor (deprived of the DM and the endothelium) after removal of affected corneal tissue, leaving behind the healthy endothelium and DM of the host. Traditionally, the technique included baring of the DM after partial trephination yet the procedures was tedious and resulted in frequent perforations of the DM[27]. DALK utilization seems to be feasible in CDs because the technique maximizes the depth of dissection through the stroma while preserving the DM. In a prospective, non-comparative case series, Vajpayeeetal[28]emphasized the efficacy of the big-bubble technique in eight patients (ten eyes) with macular, lattice, and granular dystrophies as well as corneal defects attributable to mucopolysaccharidoses and infectious keratitis. The authors reported that BCVA >6/12 was achieved in all patients and they had no intraoperative or postoperative complications. Nevertheless, early and recent reports indicated the unsuitability of DALK techniques in macular CD owing to the involvement of deep stromal layers and potentially the endothelium, which might eventually lead to increased endothelial cell attrition, DM fragility and dystrophy recurrence in donor tissues[23,29]. These studies were based on comparing their recurrence rates of macular CD with those reported in individuals studies of PK surgeries[30]. When considering direct comparative analysis, only one relevant RCT included in our study revealed insignificant differences in macular CD recurrence rates following both procedures[21].Since endothelial cells are involved in macular CD, the encouraging outcomes of low rates of endothelial rejection in DALK surgeries suggest that further investigation in macular dystrophies are needed, although the effects of these procedures on the affected and residual endothelial cells are still unknown.
Figure 4 The proportion of graft clarity and the risk of graft failure in patients who underwent DALK or PK.
Taken together, the advantages of DALK surgeries led to their gradual replacement of PKs and other lamellar techniques. Interestingly, DALK shares the same advantages of other lamellar surgeries but it overcomes the disadvantage of suboptimal improvements in visual acuity following lamellar operations that may occur due to interface irregularity and manual lamellar dissection[31]. Furthermore, both stromal and rejection rates were significantly lower than those reported after PK procedures as indicated in our study. In addition, individual investigations indicated significant increases in postoperative IOP in patients in the PK group when compared to DALK[22-23]. This is may be ascribed to the use of corticosteroids for long periods after PK and, on the other hand, unaffected intraocular tissues during DALK. However, the pooled statistical differences in IOP were not apparent in our analysis.
(三)促进文明城市建设。一个城市的阅读数量和质量,是一个城市文明形成的显性和潜在的双向元素。“书中自有黄金屋,书中自有千钟粟……”而一个文明的、高素质的人文环境构架下的城市,文明、和谐皆为水到渠成之事。
In the present study, long-term endothelial density was significantly higher after DALK as compared to PK. Kubalogluetal[32]showed that the annual loss of endothelial cell density was 14.12% after PK, which is significantly higher than that reported after DALK (5.78%). Additionally, the cumulative loss at four years of follow-up was significantly different in the DALK and PK groups (21.6% and 47.8%, respectively). Actually, the clinical significance of this finding is pertinent to long-term visual ability and graft survival. The penetrating approach may be followed by increased immune reactions, enhanced peripheral endothelial cell migration, and more prolonged corticosteroid use. The latter has proven worsening on endothelial healing and had negative impacts on the corneal endothelium[33].
On the other hand, in DALK surgeries, most of the complications were noted intraoperatively or in the early postoperative period. DMmicro perforation occurred in 16.5% of CD patients in the DALK group and the majority of patients with these perforations (88.2%) required conversion to PK surgeries. These complications might be related to surgeons’ experiences. As with other surgeries, DALK has a learning curve. Smadjaetal[34]have shown that 12 DALK surgeries (out of 42 consecutive keratoplasties) for patients with keratoconus were converted to PK surgeries, while the incidence of intraoperative DM perforation was 31.8%. Notably, the majority of these perforations occurred during the initial phase of the study and their incidence reduced significantly with the progression of the study with increased surgeons’ experience.
In addition, double anterior chamber is a frequent complication after DALK keratoplasties and it may be related to intraoperative DM perforation. Such a complication may resolve spontaneously in long-standing cases[35], or occasionally as early as four weeks postoperatively, or may require air injection into the anterior chamber to tamponade the separated DM. It is plausible that these complications would be reduced with advanced surgical expertise.
The present Meta-analysis is not without limitations. Although we were able to conclude significant correlations, the number of eligible studies was relatively small. The rarity of CDs and the small number of comparative analyses could contribute to this drawback. In addition, only one RCT was included, while other studies employed a retrospective design. This would eventually affect the reliability of the outcomes that may arise from reporting bias or selection bias. Moreover, we evidenced significant heterogeneity in the parameters of BCVA and corneal endothelial density. Hence, the lack of significant differences in these outcomes between DALK and PK may be misinterpreted. We were unable to address this issue by conducting a subgroup analysis because of the small number of studies. However, we acknowledge that the outcomes presented in this study are valuable for those planning to replace PK surgeries by DALK, particularly for patients with stromal CDs.
In patients with corneal stromal dystrophies, DALK and PK surgeries remains the treatment frequently used and had comparable outcomes on visual acuity and short-term endothelial cell density. However, DALK procedures caused a significant improvement of endothelial density two years after the operation, which could be beneficial for graft survival and visual outcomes. In addition, patients exhibited lower rates of graft stromal and endothelial rejection with DALK rather than PK. Nevertheless, DALK procedures require adequate technical experience to reduce the likelihood of intraoperative DM perforation and the subsequent development of double anterior chamber. Future studies should consider a comparative analysis of these procedures based on a randomized design, large sample sizes, long follow-up periods and including the assessment of the effects of adequate technical training of novel lamellar techniques on the patient’s outcomes also the limitation of this study that it needs further study about the decemetic and pre-decemetic DALK with femto or without femto machine should be considered as well for Meta-analysis.
