Immunotherapy – new perspective in lung cancer
2020-06-19FillipeDantasPinheiroAdrianoFernandesTeixeiraBrenoBittencourtdeBritoFilipeAntnioFrandaSilvaMariaLusaCordeiroSantosFabrcioFreiredeMelo
Fillipe Dantas Pinheiro, Adriano Fernandes Teixeira, Breno Bittencourt de Brito, Filipe Antônio França da Silva,Maria Luísa Cordeiro Santos, Fabrício Freire de Melo
Abstract Lung carcinoma is associated with a high mortality worldwide, being the leading cause of cancer death. It is mainly classified into squamous non-small cell lung cancer (NSCLC), non-squamous NSCLC, and small cell lung cancer. However,such malignancy has been increasingly subdivided into histological and molecular subtypes to guide treatment. Therapies can be used in adjuvant and palliative settings. Regarding immunotherapy, it has been widely tested in both first or subsequent palliative lines. In this sense, drugs such as pembrolizumab,nivolumab, atezolizumab, ipilimumab, avelumab, and durvalumab have been assessed in large studies. Some of these trials have also studied these medicines in adjuvant and in maintenance therapy. In recent years, advances in immunotherapy have raised the hope that the unfavorable prognosis observed in several affected individuals can be changed. Immunotherapy has increased the overall survival in squamous NSCLC, non-squamous NSCLC, and small cell lung cancer. However, it has added to the oncology practice some side effects that are unusual in standard chemotherapy and require special clinical support. In order to show how immunotherapy is being applied in the treatment of lung carcinoma, we reviewed the main studies in adjuvant and palliative scenarios.What is the better scheme? What is the better combination? What is the better dose? When should we use immunotherapy? Does programmed cell death ligand 1 expression significantly interfere in immunotherapy efficiency? Some of these questions have already been answered, while others require more investigations.
Key words: Lung cancer; Treatment; Immunotherapy; Squamous non-small cell lung cancer; Non-squamous non-small cell lung cancer; Small cell lung cancer
INTRODUCTION
The immunotherapy was thought in the 19th century by Coley in the treatment of sarcoma in patients with erysipelas[1]. In the 20th century, the idea of immunologic approaches in cancer treatment was presented and has been evaluated in different tumors. Interestingly, in 1986, interferon-alpha was approved for hairy-cell leukemia[2], and, in the 90’s, BCG was approved for adjuvant setting in bladder cancer.Furthermore, interleukin-2 was a new approach for metastatic melanoma in 1993[3].However, during 20 years the immunotherapy was forgotten, arising in 2011 with the approval of anti-cytotoxic T-lymphocyte antigen 4 for metastatic melanoma[4].
Lung cancer is the first cause of death in oncology and the past global survival curve used to be poor. The revolution provided by immunotherapy in oncology has represented a new hope in the treatment of this disease. But new different adverse effects have also been observed accompanying these advances, most of them immunemediated[5]. In addition, improvements in global survival curves in metastatic disease and local advanced disease have been noted with immunotherapy[6]. In this review,we discuss some aspects regarding immunotherapy in non-small cell lung cancer(NSCLC) and some perspectives about the use of this therapeutic modality in the adjuvant scenario and in small cell lung cancer (SCLC).
IMMUNOTHERAPY AS FIRST LINE IN METASTIC NONSQUAMOUS NSCLC
Immunotherapy with checkpoint inhibitors has become the standard treatment for advanced nondriver-mutated non-squamous NSCLC, mainly with anti-programmed cell death protein 1 and anti-programmed cell death ligand 1 (anti-PD-L1) and, in a few cases, with anti-cytotoxic T-lymphocyte antigen 4. The selection of the adequate therapy for each patient is guided by a proper immunohistochemistry, according IALSC Atlas of PD-L1 immunohistochemistry testing in lung cancer (2017)[5]. It is important to be highlighted that the above-mentioned analysis allows the stratification of patients in 3 groups of PD-L1 expression: < 1%, 1%-49%, and > 50%,and this classification correlates with overall rate response to treatment[6]. Nowadays,various challenges have been faced in the anatomopathological examination scenario.Increasingly, biopsies have been performed using less invasive procedures,generating less anatomopathological material for analysis. That circumstances increase the need of careful handling of the biopsy specimen material. Moreover, an aggravating situation is the demand for the identification of a growing number of molecular targets for treatment[7].
A phase 2 trial, keynote-021, has compared pemetrexed with carboplatin with or without pembrolizumab in metastatic non-squamous NSCLC. The overall rate response was better (56.7%) in the group with pembrolizumab after 23.9 mo when compared with patients that did not receive this drug (30.2%), as well as progressionfree survival (PFS), with a hazard ratio (HR) = 0.53. The HR for overall survival (OS)was 0.56 in favor of pembrolizumab[7]. After this trial, there were many trials analyzing the effectiveness of immunotherapy in NSCLC. In patients with the expression of PD-L1 < 50%, some trials tried to have a north in treatment.
The keynote-189, a phase III trial that included unselected patients for PD-L1, also evaluated the above-mentioned treatment. This trial showed that the immunotherapy with chemotherapyvschemotherapy alone presents a significant difference in OS within 12 mo, 69.2%vs49.5% respectively. Adverse events (AEs) occurred with grade 3 or higher in 67.2% and 65.8%. It is interesting to notice that acute kidney injury grade 3 or higher was more present in pembrolizumab group (5.2%vs0.5%).Referring to immune-mediated effects the group with immunotherapy had 22.7% of grade 3 or highervs11.9% in the group that lacked pembrolizumab. It is important to note three deaths by pneumonitis (immune-mediated side effect) in that group.Moreover, the correlation between expression of PD-L1 and time of progression or death was also reaffirmed[8].
As an alternative treatment for the patient with non-squamous NSCLC, there are combinations with atezolizumab with bevacizumab, carboplatin and paclitaxel(ABCP). This combination was tested in IMpower 150 trial, in which patients were randomized for the combination above or bevacizumab, carboplatin and paclitaxel(BCP) or atezolizumab, carboplatin and paclitaxel (ACP). After the phase of induction they received bevacizumab or atezolizumab or both in combination until progression or unmanageable toxic effects. From 1202 patients enrolled in three groups, almost half were PD-L1 negative. It is important to be highlighted that patients with drive mutation were included in this study because the specific therapy was not available in their countries. PFS was significantly longer in the group of atezolizumab, 8.3 movs6.8 mo (BCP). The same occurred with OS: 19.2 movs14.7 mo. The median duration of response was also longer in immunotherapy group (ABCP and ACP), 9.0 movs5.7 mo (BCP). Immune-mediated AEs grade 1 and 2 were present in 77.4% of patients with atezolizumab, but no grade 5 side-effect was observed. Deaths by AEs were similar in each group[9].
In 2019, another trial was published with a subgroup of patients from IMpower 150 that were affected by liver metastasis at presentation. Improved median OS was observed in favor of combination of anti-VEGF with immunotherapy groupvsbevacizumab group, 13.3 movs9.4 mo respectively. Importantly, the OS didn’t differ when groups ACPvsBCP were evaluated. However, the groups ABCP and ACP were not compared[10].
Another trial that validated atezolizumab was the IMpower 130. This trial compared a combination of chemotherapy with atezolizumabvschemotherapy alone.The scheme of chemotherapy was carboplatin with nab-paclitaxel. The median OS and PFS was significantly longer for immunotherapy group, 18.6 movs13.9 mo and 7.0 movs5.5 mo[11].
Nivolumab and Ipilimumab are an option to treat in first-line non-squamous and squamous NSCLC. This therapy was evaluated by a study conducted by Hellmannet al[12], 2019. In such a study, almost 70% of included patients had non-squamous NSCLC. Patients with PD-L1 > 1% were separated into three groups: Nivolumab alone, nivolumab with ipilimumab or chemotherapy alone. On the other hand,patients with PD-L1 < 1% were randomized for nivolumab plus ipilimumab,nivolumab with chemotherapy or chemotherapy alone. The median OS in PD-L1 > 1%was 17.1 mo in nivolumab and ipilimumabvs14.9 mo in the chemotherapy group,while in PD-L1 < 1% patients, that measure was of 17.2 mo in ipilimumab and nivolumabvs12.2 mo in the chemotherapy group. With regards to AEs we could observe similarity between groups, 32.8% with ipilimumab and nivolumabvs36% in chemotherapy group. In immunotherapy combination, the most common side effects were skin reactions and endocrine events. Treatment-related deaths were too similar,8 patients in immunotherapy combinationvs6 in chemotherapy group[12].
A different trial evaluated pembrolizumabvschemotherapy in patients with more than 50% of PD-L1 expression. Almost 30% of the patients had squamous NSCLC.The median OS was 30 mo in pembrolizumab groupvs14.2 mo in the chemotherapy group. AEs grade 3 to 5, incidences of serious treatment-related effects and treatment discontinuation were similar in both groups. Immune-mediated reactions occurred in 33.8% in pembrolizumab groups and in 5.3% in the chemotherapy group. There were 2 deaths in the immunotherapy groupvs3 in the chemotherapy one[13].
In keynote 042 the included patients had squamous (38%) and non-squamous (62%)NSCLC. The population was divided into stratum of PD-L1 expression, ≥ 50%, ≥ 20%and ≥ 1%. In patients with PD-L1 ≥ 50% the OS of pembrolizumab group was 20 movs12.2 mo in patients that did not receive the therapy. The same was observed in PDL1 ≥ 20%, with 17.7 movs13 mo, and in PD-L1 ≥ 1%, 16.7 movs12.1 mo. Adverse immune-mediated events and infusion reactions, grade 3 or worse, were higher in pembrolizumab group, 8%vs1%, and, in all grade side effects, 28%vs7%. The most common grade 3 or worse in immune-mediated adverse effects in the immunotherapy group were pneumonitis, severe skin reactions and hepatitis[14].
Since we have no trials comparing pembrolizumabvschemotherapy and pembrolizumab, Zhouet al[15], 2019 published an indirect comparison meta-analysis trying to solve this problem. It was evaluated the efficacy of pembrolizumab plus chemotherapyvspembrolizumab alone (pem) in first-line treatment of NSCLC and PD-L1 ≥ 50%. Comparisons were made with 2 blocks of two groups. Arm A with pembrolizumab plus chemotherapyvsarm C with chemotherapy and arm B with pembrolizumabvsarm C with chemotherapy. Five trials were selected, keynote 021,189, 407, 024 and 042. In direct meta-analysis OS was better for the use of pembrolizumab with chemotherapy or alonevschemotherapy alone, HR = 0.51 and 0.67 respectively. In indirect meta-analysis, however, the result was not observed, HR= 0.76, confidence interval: 0.51–1.14[15].
Nivolumab as first-line therapy was not successful. A trial published in 2017 compared nivolumab alonevschemotherapy alone. The median PFS was 4.2 mo with nivolumabvs5.9 mo with chemotherapy and median OS was 14.4vs13.2 mo respectively. AEs of grade 3 or 4 were lower in nivolumabvschemotherapy group,18%vs51%. The most immune-mediated AEs were skin-related[16].
Regarding Durvalumab, in an abstract published in 2018, 1118 patients were randomized for durvalumabvschemotherapy and durvalumab plus Tremelimumabvschemotherapy in NSCLC. However, no statistical significance in OS and PFS was observed between groups[17]. Two abstracts show better OS when patients had PD-L1≥ 25% and used statistical methods to evaluate the effect of subsequent immunotherapy, HR = 0.66 in favor of durvalumab[18,19]. Another abstract was published analyzing patients with high tumor mutational burden. In this group of patients median OS was better in durvalumab alone and associated with tremelimumabvschemotherapy, HR = 0.77 and 0.49 respectively[20].
IMMUNOTHERAPY AFTER AT LEAST ONE LINE IN METASTATIC NON-SQUAMOUS NSCLC
Nivolumab was compared with docetaxel as second-line after platinum-based doublet chemotherapy. The median OS was longer in the immunotherapy group, 12.2 movs9.4 mo. AEs grade 3 and 4 were lower in nivolumab group, 10%vs54%. The most common AEs in nivolumab group were fatigue, nausea, decreased appetite, and asthenia. In immunotherapy treatment, pneumonitis (3%vs< 1%) and hypothyroidism (7%vs0%) were more frequent. There were 2 deaths, one in each group (by encephalitis in the nivolumab group and by febrile neutropenia in the docetaxel group)[21]. In an update of this study, the median OS in two years was 29%in nivolumab groupvs16% in docetaxel group. The duration of response was longer in the nivolumab group, with 34% of the responders having a response even within two years. In patients in whom immune-modulating medications were administered to manage treatment-related AEs, nearly all AEs resolved[22]. In patients pools of checkmate 017 (squamous NSCLC) and 057 (non-squamous NSCLC), mean treatment duration of patients treated with nivolumab and docetaxel was 8.3 mo and 3.1 mo,respectively[23]. It was suggested that nivolumab provides health-related quality of life advantages compared with docetaxel, in addition to longer OS, in previously treated patients with advanced non-squamous or squamous NSCLC[24].
Atezolizumab is another option to treat patients after at least one line of treatment.A trial with non-squamous and squamous NSCLC evaluated patients to receive atezolizumab or docetaxel. It had excluded patients with previous immunotherapy or docetaxel use. The median OS was better in immunotherapyvsdocetaxel group, 13.8 movs9.6 mo. Patients with PD-L1 expression ≥ 50% had the greatest benefit from atezolizumab, median OS 20.5 movs8.9 mo. AEs grade 3 to 4 were 37% in atezolizumab groupvs54% in docetaxel group. The most common AEs were fatigue,nausea, decreased appetite and asthenia in the immunotherapy group.Musculoskeletal pain and pruritus, immune-mediated AEs, were more common in this group. Complementarily, pneumonitis was observed in 6 patients (grade 3),hepatitis was present in 2 patients (grade 3) and colitis also affected 2 patients (grade 2)[25]. The 24-mo landmark OS rate (30.9%vs21.1%) and HR (0.75) were better for atezolizumab group. In this trial, the most common immune-related AEs were rash(16.9%) and hepatitis (12.6%). Hypothyroidism (4.8%) and pneumonitis (2.3%) were also present[26].
Pembrolizumab after first-line was tested in 2016. In keynote 010, NSCLC patients were randomized in pembrolizumab (high or low dose) and docetaxel groups, of which almost 20% had squamous NSCLC and about 70% had non-squamous NSCLC.Moreover, all of them presented PD-L1 expression ≥ 1%. The median OS was 12.7 mo(high dose) and 10.4 mo (low dose)vs8.5 mo (docetaxel)[27]. An update with patients that completed 2 years of treatment and patients who received a second course of pembrolizumab was published. The OS remained longer for immunotherapy treatment with HR = 0.53 and 0.69 for PD-L1 expression ≥ 50% and ≥1%,respectively[28]. The health-related quality of life was evaluated in keynote 010 and it was better for patients in immunotherapy group[29]. The most common AEs were hypothyroidism, hyperthyroidism, and pneumonitis. Deaths occurred in five patients of each group, pneumonitis was the cause of 3 deaths in pembrolizumab group[27].
In JAVELIN lung 200 trial, avelumab was evaluatedvsdocetaxel after at least one line of treatment. All patients had expression of PD-L1. The median OS did not differ significantly between both groups, 11.4 movs10.3 mo[30].
IMMUNOTHERAPY IN METASTATIC SQUAMOUS NSCLC
There were fewer trials with only squamous NSCLC patients evaluating immunotherapy since most studies mainly evaluated patients with non-squamous NSCLC.The checkmate 227, keynote 042 and keynote 024 cited above had 30%, 38%, and 29%of squamous NSCLC patients, respectively[12,13,14].
The keynote 407 evaluated pembrolizumab only in patients with squamous NSCLC with PD-L1 expression ≥ 1%, as first-line treatment. The individuals were randomized for pembrolizumabvsplacebo with carboplatin in combination with paclitaxel or nabpaclitaxel for 4 cycles. Pembrolizumab was maintained up for 35 cycles. The median OS was better in immunotherapy group, 15.9 movs11.3 mo. Immune-mediated AEs and infusion reactions occurred in 28.8% in pembrolizumab groupvs8.6% in placebo group. Grade 3 or higher AEs were present in pembrolizumab group (10.8%) and placebo group (3.2%). There was one death in each group, both by pneumonitis. In pembrolizumab group, the most common grade 3 to 5 immune-mediated AEs were pneumonitis (2.5%), colitis (2.2%), and hepatitis (1.8%), while the other ones accounted less than 1%[31].
Another trial that evaluated only squamous NSCLC was IMpower 131. Patients were randomized for atezolizumabvsplacebo, both associated with chemotherapy.The median PFS was 6.3 movs5.6 mo, better for immunotherapy[32]. An update of that study published and presented by Jotteet al[33], 2019, at the International Association for the Study of Lung Cancer 2019 World Conference on Lung Cancer, concluded that median OS was 14.2 mo for atezolizumabvs13.5 mo for placebo. In high expression PD-L1 patients, the median OS was 23.4 movs10.2 mo, better for atezolizumab group.It is important to emphasize that the above-mentioned data were published only in abstracts[33].
There is a trial published in 2015 that compared nivolumabvschemotherapy after at least one prior therapy in metastatic setting in patients with squamous NSCLC. The median OS was better for the immunotherapy group, 9.2 movs6 mo. All patients had an expression of PD-L1. The major cause of discontinuation of treatment in nivolumab group was pneumonitis (2%), and no death was related in this group[5].
IMMUNOTHERAPY IN ADJUVANT SCENARIO ON NSCLC
Durvalumab was compared to placebo in stage III NSCLC patients after unsuccessful chemoradiotherapy. The 24-mo OS rate was better in the immunotherapy group(66.3%vs55.6%). The median time to death or distant metastasis was 28.3 movs16.2 mo also better in the durvalumab group. The most frequent AE leading to the discontinuation of treatment was pneumonitis (4.8% in durvalumab groupvs2.6% in placebo group). Death due to AEs occurred in durvalumab (4.4%) and placebo group(6.4%)[34]. After that trial, the idea of immunotherapy for adjuvant setting was rekindled, and, nowadays, have been evaluated by an amount of current studies[35](Table 1).
IMMUNOTHERAPY IN SMALL CELL LUNG CANCER
SCLC patients present lower survival rates when compared to NSCLC. Immunotherapy presents various limitations in SCLC, but advances in this field have been achieved.
There is no data on the use of immunotherapy as primary or adjuvant therapy in limited-stage SCLC. However, atezolizumab has been incorporated for extensivestage disease. A phase III trial randomized patients with extensive-stage SCLC for carboplatin and etoposide with atezolizumab or placebo for four cycles followed by maintenance phase. The median OS was 12.3 mo (atezolizumab)vs10.3 mo (placebo).It is interesting to note that the patients were not tested for PD-L1 due to the nonstandardization of samples obtained and because a low PD-L1 prevalence in tumor cells were expected. Moreover, no evidence of correlation between PD-L1 expressionand atezolizumab activity have been described. The HR was 0.7 in benefit for atezolizumab. AEs of any grade were similar in both groups. In the atezolizumab group the most common grade 3 and 4 AEs were neutropenia, anemia and decreased neutrophil count. There were three deaths in each group. In atezolizumab group, they occured due to pneumonia in one patient and neutropenia in another patient.Moreover, one death verified in this group presented unspecified cause. Regarding placebo group, deaths were due to pneumonia, septic shock and cardiopulmonary failure. Immune-mediated AEs, mainly hypothyroidism and rash, occurred in 39.9%vs24.5% in atezolizumab and placebo group, respectively. Most grade 3 and 4 immune-mediated AEs in atezolizumab group were rash (2%), infusion-related reaction (2%), hepatitis (1.5%), and colitis (1%)[36].
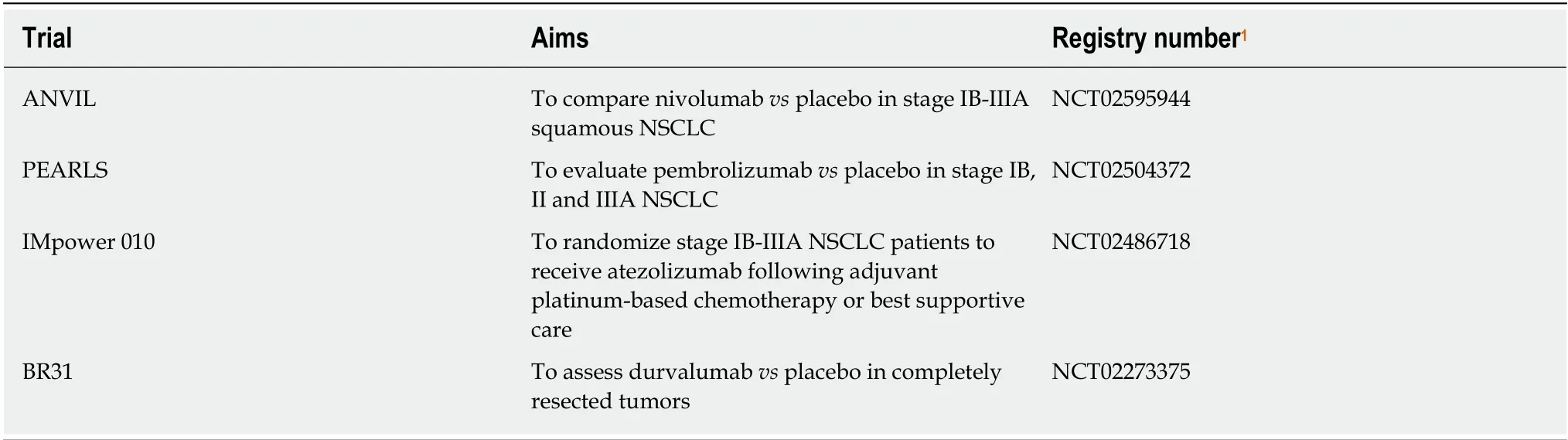
Table 1 Ongoing trials on lung cancer immunotherapy
In the treatment of patients suffering relapses of 6 mo or fewer, some immunotherapy options have been tried, but the treatment standardization is being sought by some trials. In this framework, one possibility is the combination of ipilimumab and nivolumab. There is a phase 1/2 trial that tested nivolumab alone or nivolumab with ipilimumab for patients with limited or extensive-stage diseases after progression with at least one platinum-based chemotherapy regimen. Due to the same reasons reported by the above-mentioned trial, PD-L1 expression was not tested, and this parameter was assessed only retrospectively. There were four groups with different doses of nivolumab and ipilimumab. The objective response was 23% in nivolumab 1 mg/kg plus ipilimumab 3 mg/kg groupvs10% in nivolumab 3 mg/kg groupvs19% in nivolumab 3 mg/kg plus ipilimumab 1 mg/kg groupvs33% in nivolumab 1 mg/kg plus ipilimumab 1 mg/kg group (just 3 patients in this group).Grade 3 and 4 AEs occurred in 30%, 13%, 19%, 0% patients, respectively, and the most common of them were increased lipase and diarrhoea[37].
An update of Checkmate 032 was published as abstract in 2017. In which, the randomization was to nivolumab or nivolumab 1 mg/kg plus ipilimumab 3 mg/kg.The median disease control rate was 36%vs49%, respectively[38].
Pembrolizumab is another possibility in SCLC immunotherapy. That drug was tested in phase 2 trial with advanced SCLC with one or two previous treatment. All patients were tested for PD-L1 expression and it was positive if ≥ 1%. The objective response rate was 35.7% in positive PD-L1 expression and 6% in negative PD-L1 expression. The median OS was 14.6 mo in PD-L1 positive group and 7.7 mo in PD-L1 negative group[39].
There are few studies published for immunotherapy in SCLC, but there are almost 30 open trials with immunotherapy in different lung cancer settings[40]. Figure 1 summarizes the safety level for an indication of immunotherapeutic drugs in the treatment of lung cancer.
CONCLUSION

Figure 1 Safety level for indication of immunotherapeutic drugs in the treatment of lung cancer. SCLC: Small-cell lung cancer; NSCLC: Non-small-cell lung cancer.
As a conclusion, immunotherapy is considered the new standard in advanced and metastatic NSCLC, with or without chemotherapy. Moreover, it is evident that adequate immunohistochemistry is essential in NSCLC approach since it strongly correlates with treatment response. The benefit of immunotherapy was documented in patients with different sites of metastasis, chemotherapy combination, and expression of PD-L1, although OS in patients with PD-L1 expression ≥ 50% was higher. It is important to be highlighted that promising results have been achieved in both squamous and non-squamous NSCLC, as well as in SCLC. Furthermore, either in first-line or after at least one line, immunotherapy has presented good effects.However, almost all the trials that tested immunotherapy showed immune-mediated AEs and even deaths related to this. In addition, when two immunotherapies are combined, the immune-mediated side effects tend to be worse. The most commonly observed immune-mediated AEs were pneumonitis, hepatitis and skin reactions. In a near future, it is expected that new treatment schemes involving immunotherapy and its combinations will be established. Even now, there are many doubts on what are the optimal doses and the adequate duration for immunotherapies. Finally, the expansion of the knowledge about the use of this therapeutic modality as adjuvant treatment, and new studies on the immune-mediated adverse effects due to these treatments will improve their application in clinical practice.
杂志排行
World Journal of Clinical Oncology的其它文章
- Human epidermal growth factor receptor 2 positive rates in invasive lobular breast carcinoma: The Singapore experience
- CITED2 and the modulation of the hypoxic response in cancer
- Impact of primary tumour location on colorectal liver metastases: A systematic review
- Formulation strategies in immunotherapeutic pharmaceutical products