Successful robotic radical resection of hepatic echinococcosis located in posterosuperior liver segments
2020-06-17ZhiMingZhaoZhuZengYinYuanMengNanJiangZhiGangMaLiChaoPanXiangLongTanXiongChenRongLiu
Zhi-Ming Zhao, Zhu-Zeng Yin, Yuan Meng, Nan Jiang, Zhi-Gang Ma, Li-Chao Pan, Xiang-Long Tan,Xiong Chen, Rong Liu
Abstract
Key words: Cystic echinococcosis; Alveolar echinococcosis; Robotic surgery;Posterosuperior segment; Caudate lobe; Liver
INTRODUCTION
Echinococcosis is a zoonotic disease caused byEchinococcustapeworms, which can lead to damage to tissues and organs such as the liver, lungs, and brain. Human liver echinococcosis mainly includes cystic echinococcosis (CE) caused byEchinococcus granulosusinfection and alveolar echinococcosis (AE) caused byEchinococcus multilocularisinfection[1]. The worldwide spread of echinococcosis has made the disease a serious threat to public health, especially in Western China. The World Health Organization (WHO) has listed echinococcosis as one of the 17 diseases to be controlled or eliminated by 2050[2].
According to the classification by the WHO Informal Working Group on Echinococcosis[3,4], the treatment methods for hepatic echinococcosis include surgery,medication, and puncture and drainage. Radical resection remains the primary treatment for CE2, CE3, and AE[5]. Since the first laparoscopic pericystectomy for hepatic echinococcosis carried out in France in 1991 by Katkhoudaet al[6], there have been increasing reports on the laparoscopic treatment of CE[7-10]. The posterosuperior region of the liver - such as the caudate lobe (segment I), segment VII, and segment VIII - is considered to be the site where difficult lesions reside and remains the most challenging region for complex laparoscopic hepatectomy. Thus, extensive experience in open laparoscopic hepatectomy is imperative[11,12].
The da Vinci Surgical System (Intuitive Surgical Inc., United States) is an advanced and minimally invasive surgery tool, which has been shown to have advantages in complex hepatectomy[13,14]. Since Giulianottiet al[15]reported two cases of robotic hepatic hydatid surgery in 2011, the literature on robotic hepatic hydatid surgery in difficult lesions has mostly been presented in case reports[16]. The aim of this study was to retrospectively analyze the data on robotic surgery for hepatic echinococcosis in difficult lesions from two centers in China and to explore the experience of performing robotic surgery for CE and AE.
MATERIALS AND METHODS
Study population and data collection
A retrospective analysis was conducted of the clinical data of patients with hepatic echinococcosis who underwent robotic surgery at the Second Department of Hepatopancreatobiliary Surgery, The First Medical Center, Chinese People’s Liberation Army General Hospital as well as the Department of Hepatobiliary Surgery, The People’s Hospital of Xinjiang Uygur Autonomous Region, from September to December 2019. The inclusion criteria were: (1) Patients who had pathologically confirmed CE or AE; (2) Patients who had lesions located in the caudate lobe of the liver (segment I), segment VII, and segment VIII; and (3) Patients who underwent total pericystectomy, segmental hepatectomy, or hemihepatectomy.The exclusion criteria were: (1) Patients who had multiple organ echinococcoses; and(2) Patients who could not tolerate anesthesia or surgery.
Overall, 5 patients (all men, aged 21-56 years, with a median age of 37 years) were enrolled. The body mass index was 21.22-30.1 kg/m2, with a median body mass index of 25.54 kg/m2. The classification by the American Society of Anesthesiologists was IIII. Among them, 4 cases presented with CE alongside 1 case of AE, with a median tumor diameter of 75 mm (51-80 mm) (Table 1).
All patients completed abdominal ultrasound, computed tomography and magnetic resonance imaging examinations (Figure 1) before operation, and multidisciplinary discussion and WHO Informal Working Group on Echinococcosis classification were performed. All patients provided written informed consent. The research was approved by the hospital ethics committee, which complies with medical ethics regulations. All operations were performed by surgeons with vast experience in laparotomy and robotic hepatectomy.
Surgical procedure
Position and trocar hole layout: Tracheal intubation integrated with intravenous general anesthesia was performed in a 25° reverse Trendelenburg position and a lithotomy position. When resection of segment of VII or VIII was required, the patient was turned 45° to his left side. The CO2pneumoperitoneum pressure was controlled at 14 mmHg, and the central venous pressure was maintained at 0-5 cm H2O[17].Robotic procedures were performed using the da Vinci Si or Xi Surgical Systems(Intuitive Surgical Inc., United States).
The trocar layout consists of the optic port: 12 mm trocar, located at 3 cm on the right side of the umbilicus; assistant port: 12 mm trocar, located on the umbilicus (3 cm above the umbilicus when segment VII is excised); robotic arm 1:8 mm trocar,located 3-5 cm below the xiphoid processes (below the xiphoid process when segment VII is excised); robotic arm 2:8 mm trocar, located below the costal margin of the right anterior axillary line; and robotic arm 3:8 mm trocar, located below the costal margin of the left anterior axillary line.
Operation methods: Intraoperative ultrasound and the Pringle maneuver were routinely used. According to previous reports[18,19], the operation methods can be summarized as follows. (1) Caudate lobectomy: The left lateral and Spiegel’s lobes were dissociated, and the short hepatic vessels of the caudate lobe were ligated using Hemolock clip (TFX Medical, RTP Durham, NC, USA). After the caudate lobe was separated from the inferior vena, the Arantius ligament and the hepatic pedicle branch of the caudate lobe were ligated using Hemolock clip. The hepatic parenchyma of the caudate lobe was detached using an ultrasonic scalpel, and the hydatid cyst was detached from the middle and the right hepatic veins. During intraoperative hepatic vein hemorrhage, the CO2pneumoperitoneum pressure was increased to 15 mmHg at first; the hemorrhage of branches < 2 mm could be bipolarly occluded; and the ethmoidal foramina > 2 mm in hepatic veins were treated with 6-0 prolene suture. After the detachment of the hepatic parenchyma, wound surface was fully exposed in the inferior vena cava as well as the left, middle, and right hepatic veins (Figure 2A and B). (2) Hepatectomy of segment VII: The right liver needed complete mobilization. The hepatic parenchyma was detached along the cephalic approach of the right hepatic vein; the right hepatic vein branch of segment VII and the hepatic pedicle branch of segment VII were ligated using Hemolock clip; and the hydatid cyst was removed from the right hepatic vein (Figure 2B and C). (3)Pericystectomy of segment VIII: After appropriate mobilization of the right liver, the hepatic parenchyma was detached at 2 cm from the margin of the hydatid cyst; the branches of the right and middle hepatic veins as well as the hepatic pedicle branch of segment VIII were ligated using Hemolock clip; and the focus was resected completely. and (4) Right hemihepatectomy: The right gallbladder was resected, and the right hepatic artery and the right branch of the portal vein were ligated. After complete right liver mobilization, the right hepatic parenchyma was detached with an ultrasound scalpel; the branches of segment V and segment VIII of the middle hepatic vein were ligated using Hemolock clip; and the right hepatic duct and right hepatic vein were detached, respectively.
The drainage tube was routinely placed on the cross section of the liver or through the Winslow hole, which was led out from robotic arm 2. The specimens were taken using the extended assistant port in the midline of the upper abdomen.
Perioperative results and follow-up
The operation time, intraoperative blood loss and blood transfusion rate,postoperative complications, drainage tube removal time, and postoperative hospital stay were assessed. The data were expressed as median and analyzedviaIBM SPSS Statistics 20 statistical software. No patient took albendazole orally after the operation,and all patients underwent abdominal ultrasound or computed tomography 1 and 3 months after operation.
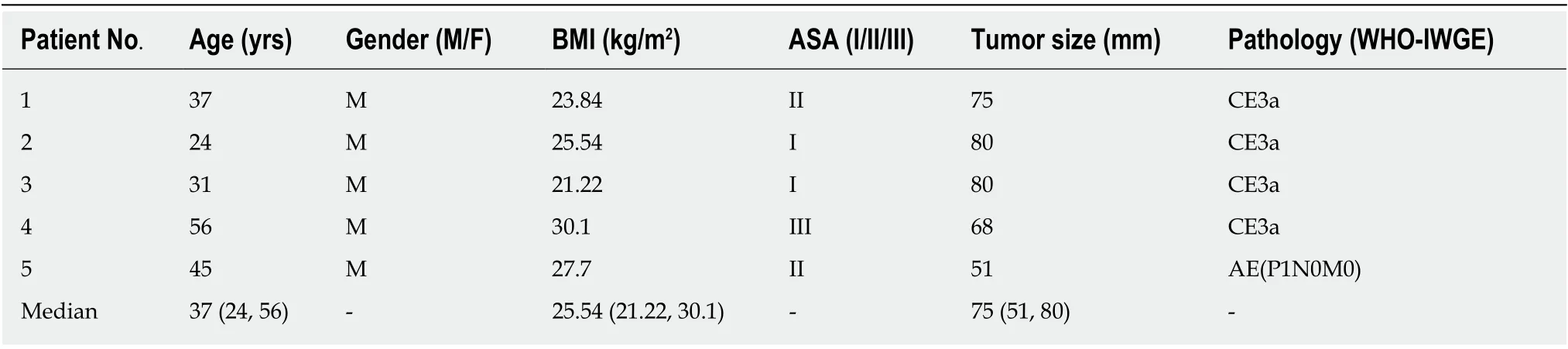
Table 1 Demographic and clinical characteristics of the patients
RESULTS
All 5 patients successfully underwent robotic radical hepatectomy for hepatic echinococcosis, including total caudate lobectomy (n= 2), hepatectomy of segment VII(n= 1), total pericystectomy of segment VIII (n= 1), and right hemihepatectomy (n=1), without conversion to laparotomy or perioperative deaths. The median operation time was 225 min (175-300 min); the median blood loss was 100 mL (50-600 mL), with 4 U of red blood cell suspension transfused in 1 patient because of an intraoperative blood loss of 600 mL; the median postoperative hospital stay was 10 d (5-19 d); and the median drainage tube removal time was 10 d (4-16 d). No bile leakage was found in any of the patients. According to the Clavien-Dindo complication grading, there were 4 cases of grade I and 1 case of grade II complications. The case of grade II complications with CE of the caudate lobe had postoperative right hepatic subcapsular hematoma; however, the patient recovered after bed rest and symptomatic treatment (Table 2). No recurrence of echinococcosis was found in any of the patients at 3 mo of follow-up.
DISCUSSION
Surgery is an important treatment method for hepatic echinococcosis, and the postoperative recurrence rate of hepatic echinococcosis has been reported to be 2%-25%[20]. The surgery for CE includes radical surgery and palliative surgery. In accordance with the report of Georgiouet al[21], the complication rate and 3-year postoperative recurrence rate of radical surgery are 10.95% and 6.9%, respectively,whereas the complication rate of palliative surgery is 24.13%. At present, the preferred radical resection approach for CE includes pericystectomy and segmental or partial hepatectomy[2]. The imaging findings of AE are similar to those of liver malignancies, and AE is associated with a 90% mortality rate in untreated patients.Hepatectomy is the main surgical method for AE, and liver transplantation can be considered as the last resort for end-stage AE[22].
In 2016, Di Benedettoet al[23]reported a case of caudate lobectomy (Spiegel’s lobe)for CE for the first time. The focus diameter was 5.6 cm; the operation time was 280 min; the blood loss was 200 mL; and the postoperative hospital stay was 3 d. To date,robotic total caudate lobectomy alone has not been reported in the literature. During traditional laparoscopic anatomical caudate lobectomy, due to the defects in twodimensional visual field and endoscopic instruments, the dorsal part of the middle hepatic vein is often poorly exposed, and tearing of the small branches of the paracaval portion and the middle hepatic vein often results in catastrophic hemorrhage, which is difficult to treat under endoscopy[24]. In the present study,lesions in the caudate lobe in 2 cases of CE involved the Spiegel’s lobes, caudate processes, and paracaval portion; the focus diameter was 8 cm; and the hydatid cyst was adjacent to the hepatic vein, inferior vena cava, and hepatic pedicle. We adopted the left approach, completely removed the hydatid cyst from the surface of the hepatic vein, and successfully performed robotic total caudate lobectomy.
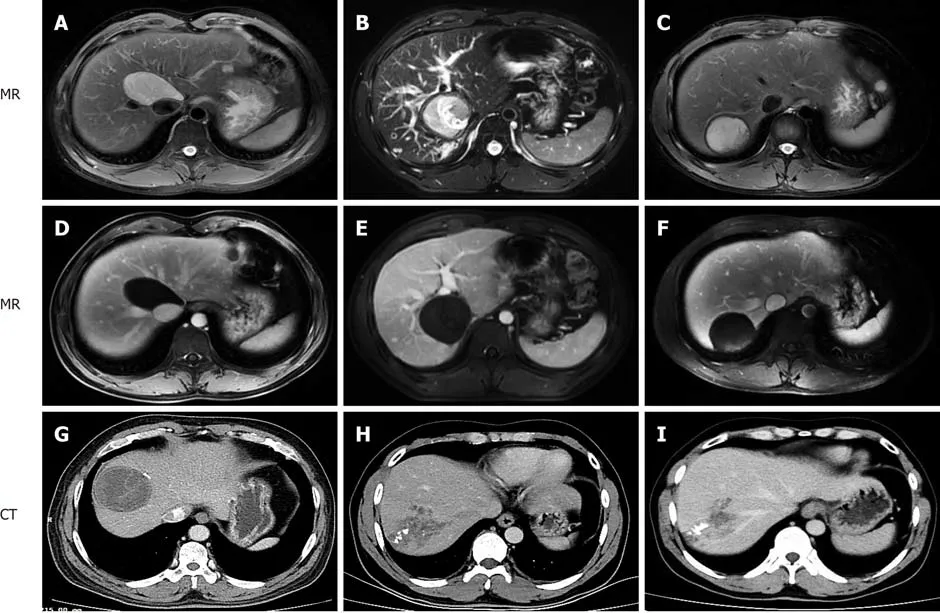
Figure 1 Contrast-enhanced magnetic resonance imaging and computed tomography manifestations of hepatic cystic and alveolar echinococcosis. A, D:Patient 1, cystic echinococcosis in caudate lobe; B, E: Patient 2, cystic echinococcosis in caudate lobe; C, F: Patient 3, cystic echinococcosis in segment VII; G:Patient 4, cystic echinococcosis in segment VIII; H, I: Patient 5, alveolar echinococcosis in segment VII/VIII. MR: Magnetic resonance; CT: Computed tomography.
In 2011, Casciolaet al[25]reported robotic partial hepatectomy of segments I-VIII,including pericystectomy of segment IVa in 1 case and segment VII in 1 case. The study showed that robots had certain advantages in partial hepatectomy in the posterosuperior region of the liver or in cases with the focus adjacent to the hepatic vein. In 2013, Troisiet al[26]also found that compared with laparoscopic hepatectomy,robotic surgery is safe and feasible in hepatectomy for difficult lesions of the posterosuperior region of the liver, and thus, has certain advantages in hepatectomy with the preservation of the liver parenchyma. In the current study, the focus of CE at segment VII was adjacent to the right hepatic vein in 1 case. After the focus was located by ultrasound during the operation, the hydatid cyst and the right hepatic vein were finely detached via the cephalic approach of the right hepatic vein, and segment VII was resected completely. In addition, pericystectomy was successfully performed in 1 case of CE at segment VIII. The operation time in 2 patients were 175 min and 300 min, respectively; the intraoperative blood loss was 100 mL; the postoperative hospital stay was 11 d and 5 d, respectively; and the Clavien-Dindo complication grades were grade I in both.
In 2019, Magistriet al[16]reported the results of robotic surgery in 15 cases of CE from 3 centers in Italy, including resection of the Spiegel’s lobe (as reported by Di Benedettoet al[23]), and other difficult segments. Consequently, we believe that the robot’s video imaging system, which provides a magnified high-definition threedimensional visual field, can ensure full exposure of the deep space of the caudate lobe, segment VII, and segment VIII. With the advantages of simulating the flexibility of the human wrist, eliminating hand tremor, and providing continuous and stable traction, the robotic arm can assist in the fine separation of hydatid cyst from the hepatic vein and suturing of the hepatic vein hiatus, and reduce uncontrollable hemorrhage.
Radical hepatectomy for AE requires that the normal liver tissues should be more than 1 cm above the edge of the focus, so as to eliminate the active hyperplasia region of the focus. Laparoscopic and robotic hepatectomy for AE, however, has not been reported in the literature. In the present study, robotic right hepatectomy was successfully performed in 1 case of AE involving segment VII and segment VIII. The operation time was 225 min; the blood loss was 200 mL; the postoperative hospital stay was 9 d; and the Clavien-Dindo complication grade was grade I. As such, we believe that robotic hepatectomy is safe and feasible for AE partially confined to the hemiliver or hepatic segment.
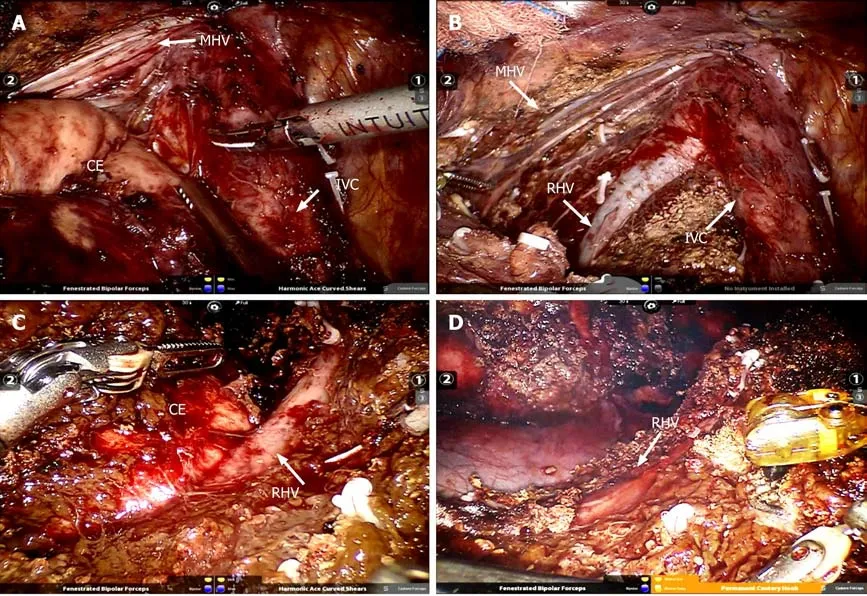
Figure 2 lntraoperative visual field and status after removal of the specimen. A: Cystic echinococcosis was located in caudate lobe adjacent to the inferior vena and hepatic vein; B: Complete caudate resection; C: cystic echinococcosis was located in segment VII adjacent to the right hepatic vein; D: Segment VII resection.CE: Cystic echinococcosis; IVC: Inferior vena cava; RHV: Right hepatic vein; MHV: Middle hepatic vein.
In summary, robotic radical surgery for cystic and selected alveolar echinococcosis in difficult liver lesions is safe and feasible.
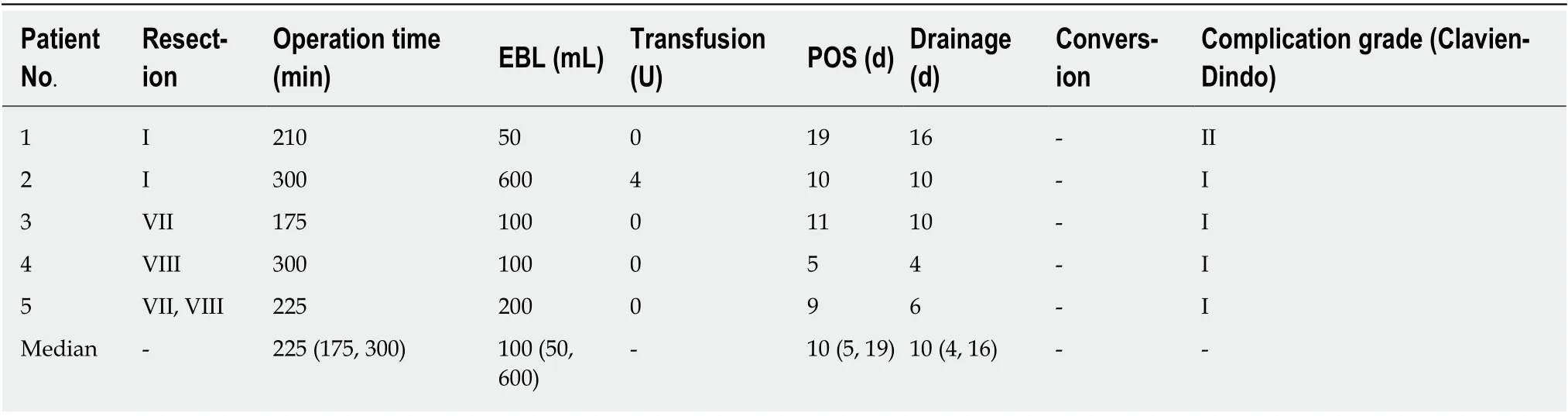
Table 2 Perioperative data and outcomes
ARTICLE HIGHLIGHTS
Research background
Radical resection is an important treatment method for hepatic echinococcosis. The posterosuperior segments of the liver remain the most challenging region for laparoscopic or robotic hepatectomy.
Research motivation
This study intended to retrospectively analyze the clinical data on robotic surgery for hepatic echinococcosis in difficult lesions from two centers in China and to explore the experience of performing robotic surgery for cystic and alveolar echinococcosis.
Research objectives
The aim of this study was to demonstrate the safety and preliminary experience of robotic radical resection of cystic and alveolar echinococcosis in posterosuperior liver segments.
Research methods
A retrospective analysis was conducted on the clinical data of patients with hepatic echinococcosis who underwent robotic surgery from September to December 2019.
Research results
All 5 patients successfully underwent robotic radical hepatectomy for hepatic echinococcosis,including total caudate lobectomy, hepatectomy of segment VII, total pericystectomy of segment VIII, and right hemihepatectomy, without conversion to laparotomy or perioperative deaths. The operation time was 225 min; the blood loss was 100 mL; and the postoperative hospital stay duration was 10 d. The Clavien-Dindo complication grade was grade I in 4 cases and grade II in 1 case. No recurrence of echinococcosis was found in any of the patients after 3 mo of follow-up.
Research conclusions
This study suggested that robotic radical surgery for cystic and selected alveolar echinococcosis in difficult liver lesions is safe and feasible.
Research perspectives
Robotic transabdominal approach can be an option for resection of cystic and selected alveolar echinococcosis located in the posterosuperior hepatic segments.
杂志排行
World Journal of Gastroenterology的其它文章
- Tailored classification of portal vein thrombosis for liver transplantation: Focus on strategies for portal vein inflow reconstruction
- Alternative uses of lumen apposing metal stents
- lnnate immune recognition and modulation in hepatitis D virus infection
- Use of zebrafish embryos as avatar of patients with pancreatic cancer: A new xenotransplantation model towards personalized medicine
- Gan Shen Fu Fang ameliorates liver fibrosis in vitro and in vivo by inhibiting the inflammatory response and extracellular signalregulated kinase phosphorylation
- Periportal thickening on magnetic resonance imaging for hepatic fibrosis in infantile cholestasis
