Effects of ciprofloxacin on testicular tissue and sperm quality in rabbits
2020-04-08RezaKheirandishLadanEmadiBaharakAkhtardaneshShahrzadAziziMasoudImaniFatemehMahmoodabadiFereshtehIraniHomaShokrizadeh
Reza Kheirandish, Ladan Emadi, Baharak Akhtardanesh, Shahrzad Azizi✉, Masoud Imani, Fatemeh Mahmoodabadi,Fereshteh Irani, Homa Shokrizadeh
1Department of Pathobiology, Faculty of Veterinary Medicine, Shahid Bahonar University of Kerman, Kerman, Iran
2Department of Basic Sciences, Faculty of Veterinary Medicine, Shahid Bahonar University of Kerman, Kerman, Iran
3Department of Clinical Sciences, Faculty of Veterinary Medicine, Shahid Bahonar University of Kerman, Kerman, Iran
4Faculty of Veterinary Medicine, Shahid Bahonar University of Kerman, Kerman, Iran
ABSTRACT Objective: To investigate the hormonal, histopathological toxicity and sperm quality of ciprofloxacin in male genital system in the rabbit model.Methods: Twenty adult New Zealand male rabbits were randomly divided into the treatment and control groups, and respectively received 30 mg/kg/day ciprofloxacin and normal saline intraperitoneally for 14 days. Blood samples and testicular tissues were taken for testosterone by enzyme linked immunosorbent assay method, and measurement of histopathologic and histomorphometric investigations was made on the 14th day of the experiment and 56 days after the last dose of ciprofloxacin. Additionally, epididymis sperm sample was collected for quality analysis.Results: On day 14 of the experiment, histopathologic examination revealed severe degenerative changes in the epithelium of seminiferous tubules and loss of all germ cells in most tubes in the treatment group. In the histomorphometric study, significant reductions in the seminiferous tubules diameter, epithelium height,and Johnsen’ score were observed. On day 56 after the last dose of ciprofloxacin, the seminiferous tubules revealed regeneration in the treatment group and no significant difference was observed in the spermatogenesis parameters except epithelial height parameter between the control group and the treatment group. All sperm quality parameters were significantly decreased on day 56 after the last dose of ciprofloxacin. Testosterone levels did not significantly change during the follow-ups period.Conclusions: There is potential reversible testicular toxicity for ciprofloxacin in the rabbit model in according to relative regeneration of spermatogenic epithelium after 56 days of last dose of ciprofloxacin. Sperm quality will be improved with a delay after complete regeneration of seminiferous tubules.
KEYWORDS: Ciprofloxacin; Testis; Rabbits; Histopathology;Testosterone; Histomorphometry
1. Introduction
Infertility is a significant problem with a 20% incidence among couples and reported more in men[1,2]. Various agents lead to infertility in males including defects in the spermatogenesis, sperm transportation, number and morphology of sperm[1], infections of the urinary system[3,4] and anatomical factors such as varicoceles and ductal obstructions[5]. Also, male fertility may be affected by some environmental risk factors such as cigarette smoking,radiation, nutritional condition, estrogens, heavy metals, scrotal temperature and anti-bacterial drugs[6,7]. Antibiotics may induce injury to the spermatogenesis in men and animal species. One of the antibiotics is ciprofloxacin that belongs to the second-generation fluoroquinolones[8]. This broad-spectrum antibiotic enters the seminal fluid and decreases concentration, motility and viability of sperm[9]. Long use of some quinolones causes toxicity in the spermatogenesis and testicular tissue[10].
Rabbits are excellent models for many aspects of research in reproductive toxicology. In the present study, the side effects of ciprofloxacin were investigated on male rabbit system by histopathological and histomorphometric evaluation.
2. Materials and methods
2.1. Experimental animals
Twenty white adult New Zealand male rabbits (Oryctolagus caniculus) (12 months old, 2-4 kg) were kept in the cages for one week until be adapted to the environment under the standard condition [12 h light-12 h dark/ (22 ± 2) ℃] and free access to the balanced diet and waterad libitum. The animals were randomly divided into the control and ciprofloxacin (treatment) groups (n=10 in each group). The ciprofloxacin group received intraperitoneal ciprofloxacin at dose of 30 mg/kg/day for 14 days. The control group received the same volume of normal saline. The 30 mg/kg is was treatment dose with a course of 14 days for usually infetions in human[11].
2.2. Blood collection
Blood samples (5 mL) were taken from the jugular vein of each rabbit in the control and treatment groups for hormonal analysis on the 14th day after the beginning of treatment (the 2nd week) and 56th day following the last ciprofloxacin dose. 56 days was choosen according to a cycle of spermatogenesis in rabbit that is was 48 days.Serum was separated by the centrifuge at 3 000 rpm for 10 min and testosterone level was measured by DRG testosteron enzyme linked immunosorbent assay kit (EIA-1559).
2.3. Histopathological and histomorphometric investigations
Five animals were selected from each ciprofloxacin and control groups on the 14th day of the experiment and 56 days after the last ciprofloxacin dose to conduct histopathological and histomorphometric investigation. After euthanasia with sodium thiopental overdose, testes from rabbits of both groups were fixed in 10% neutral buffered formalin. After fixation, the tissue samples were processedviathe standard procedure and embedded in the paraffin wax. Tissue sections in 5 μm thickness were stained with hematoxylin-eosin (H & E) and studied by light microscopy(Olympus, Model: CX31) with 40, 100, 400 magnifications in according to investigated parameteres. For the histomorphometric study, diameter and height epithelium in 10 smallest and roundest seminiferous tubules were investigated. In addition, the diameter of 10 spermatogonia[12] and Johnsen’s score were determined in the control and ciprofloxacin testes[13]. The level of sperm maturation is was graded between 1 and 10, according to the most advanced germ cell in the tubule.
2.4. Sperm sample collection and preparation
Sperm samples were obtained from 10 cases of 20 animals of each group during the experimental period in the 14th day of the experiment and 56 days after the last ciprofloxacin treatment. In order to limit blood contamination, the cauda epididymis was dissected from the connective tissues, rinsed in the 37 ℃ normal saline and dried carefully. Samples of mature spermatozoa were collected from the caudal region of epididymis by finely mincing it in phosphate-buffered saline at 37 ℃. Sperm evaluation was carried out by Computer Assisted Semen Analysis (CASA) system(HFT CASA V6.50, Hooshmand Fanavar Tehran Co., Iran) in each experimental group.
2.5. Sperm analysis
Sperm concentration, motile sperm ratio and sperm motion characteristics were measured with the CASA system. Briefly,10 μL of sperm sample was pipetted into a sperm counting chamber with 10 μm depth that had been prewarmed to 37 ℃ on a heated microscopic stage (HT 50, Minitube Inc., Germany) and evaluated by a light microscopy (DN-PW117M, Pro Way Optics and Electronics Co., China) with magnification of ×40. At least 1 000 spermatozoa were observed in eight sequentially selected microscopic fields.The spermatozoa motility patterns were monitored by a digital video camera system (SDS-313B, Samsung Techwin Co., South Korea) connected to the light microscope. Five motion parameters obtained from CASA sperm tracker were as follows: (1) curvilinear velocity (VCL, micrometers per second): the average velocity over the total distance moved, including all deviations of sperm head movement; (2) straight-line velocity (VSL, micrometers per second):the average velocity calculated using the straight line distance between the beginning and end of the sperm track; (3) average path velocity (VAP, micrometers per second): the average velocity of the sperm head along its average path; (4) amplitude of lateral head displacement (ALH, micrometers): the mean value of the extreme side to side movement of the sperm head in each beat and (5)straightness of the path velocity (VSL/VAP) (STR). Additionally,sperms based on motion properties were divided into four categories:Class A: Motile sperm with high-velocity progressive motion; Class B: Motile sperm with low-velocity progressive motion; Class C:Sperm moving in place; Class D: Non-motile sperm.
2.6. Statistical analysis
The results were analyzed by SPSS 17.0 (SPSS Inc., Chicago,IL, USA). Independent Student’st-test were used for investigated parameters for comparing the control and ciprofloxacin groups. Data are expressed as mean standard deviation (mean±SD).P-value less than 0.05 was considered as statistically significant different level.
2.7. Ethics statement
This study was approved by the Ethical Committee of Shahid Bahonar Veterinary School (ethical approval No. IR.UK.REC.1395.001). All animals received human care in compliance with the Guide for Care and Use of Laboratory Animals published by the National Institutes of Health.
3. Results
3.1. Histopathological findings
In the control group, the microscopic study revealed normal structure of the seminiferous tubules, spermatogenesis and Sertoli cells during the experiment (Figure 1A). Fourteen days after initiation of ciprofloxacin injection, the ciprofloxacin group showed severe degenerative changes in the epithelium of the seminiferous tubules. The most tubules were wrinkled and collapsed. All the germ cells had decreased and only the spermatogonia were observed. Sertoli cells had a clear nucleus and marked nucleolus.Giant-like cells were also visible in the seminal lumen (Figure 1B).Edema and hemorrhage had occurred in the interstitial tissues between the tubules (Figure 1B). 56 days after the last ciprofloxacin dose, most of the tubules were regenerated in the ciprofloxacin group. All stages of germ cells from spermatogonia to spermatozoa were present. The epithelium of the seminiferous tubules showed the structure near to the control group (Figure 1C).
3.2. Histomorphometric evaluation
Fourteen days after initiation of ciprofloxacin injection,Johnsen’s score (indicator for spermatogenesis), the diameter and epithelium height of the seminal tubules significantly decreased in comparison to the control group (P<0.05). However, the diameter of spermatogonium nucleus in the ciprofloxacin group was significantly higher than that in the control group (P<0.05)(Table 1).
And 56 days following the last ciprofloxacin dose, evidence of regeneration was observed in the tubular epithelium and these tubules were reconstructed. The most spermatogenesis parameters were the same as the normal control group. There were no significant differences in the diameter of the seminal tubes, spermatogonia nucleus and the Johnsen score between the ciprofloxacin group and the normal control group (P>0.05) (Table 1). In the ciprofloxacin group, the epithelial height had increased in comparison to the second week but it was significantly lower than the control group at this time (P<0.05) (Table 1).
3.3. Sperm quality
Table 2 showed the effect of ciprofloxacin 14 days after initiation of drug injection and 56 days after the end of drug administration in comparison with the control group in sperm concentration,motile sperm ratio and sperm motion characteristics. Evaluation of epididymal sperm quality parameters 14 days after initiation of drug injection revealed that sperm concentration, motile sperm ratio and sperm motion parameters were slightly decreased. When the testis be was damaged, it takes took a long time about a spermatogenic cycle until sperm quality will would be affected. Therefore, during 2 weeks, sperm quality remains remained near to normal range.
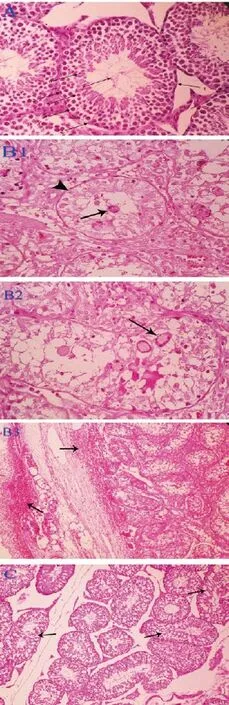
Figure 1. Histopathological findings of ciprofloxacin on the testis. A: The control group: 1) Normal seminiferous tubules in rabbit, 2) Sertoli cell, 3)Spermatogonium cell, 4) Primary spermatocyte, 5) Round spermatid, 6) Rod spermatid, 7) Spermatozoa (H & E, ×400). B: Ciprofloxacin-treated group:B1) Severe degeneration of germinal epithelium, sloughing of epithelial cells into lumen (arrow) and remained Sertoli cell with a marked nucleolus(arrowhead) (H & E, ×400); B2): Degeneration of the germ cells and presence of multinucleated cells in seminal lumen (arrow) (H & E, ×400);B3): Wrinkled and collapsed tubules due to severe degeneration of the germ cell lines as well as hemorrhage (arrows) between tubules (H & E, ×100).C: Ciprofloxacin-treated group for 56 days following last ciprofloxacin.Mild degenerative changes as vacuolation and increasing space (arrows) in germinal epithelium of seminiferous tubules (H & E, ×400).
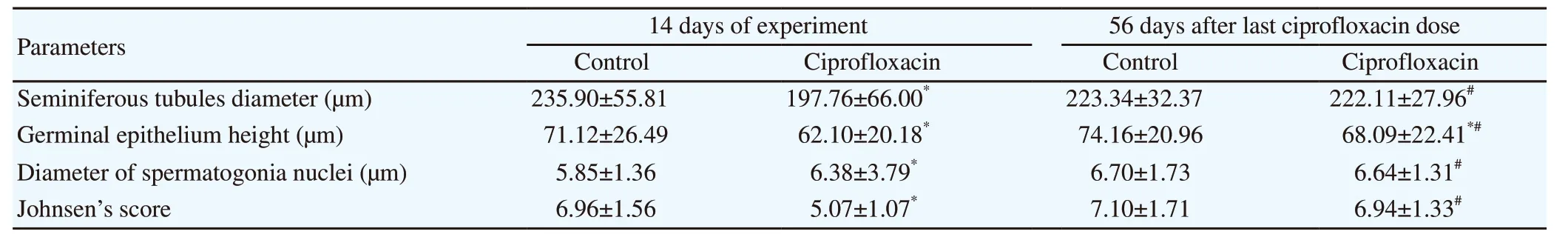
Table 1. Seminiferous tubules diameter, germinal epithelium height, diameter of spermatogonia nuclei and Johnsen’s score in the control and ciprofloxacin (30 mg/kg) groups.

Table 2. Effect of ciprofloxacin on sperm motion patterns at each evaluated time.
However, a mild elevation was seen in non-motile sperm count.While 56 days after the end of drug administration, sperm concentration significantly decreased in comparison with the control group. Motile sperm ratio (class A and B) was significantly decreased in the treatment group, whereas the proportion of nonmotile sperms (class D) was significantly increased compared to the control group. Sperm velocity parameters (VCL, VSL and VAP)significantly decreased in comparison with the control group. Motion characteristics such as ALH that showed the ability of sperm cells in penetration through the oocyte significantly decreased in the treatment group. The significant reduction of straightness of the path velocity(STR) was observed in comparison with the control group (Table 2).
3.4. Serum testosterone level
Level of the serum testosterone on the 14th day of the experiment and 56 days after the last ciprofloxacin dose showed no significant difference statistically between the ciprofloxacin and control groups(P>0.05) (Table 3).
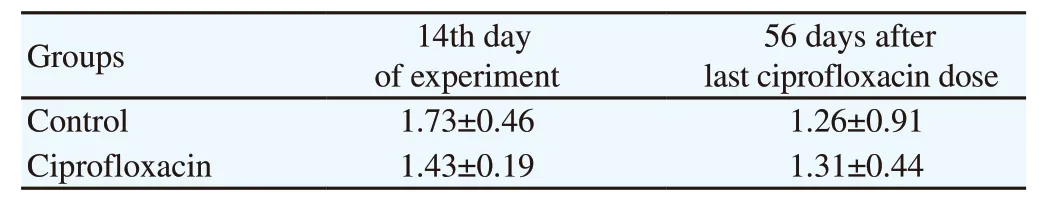
Table 3. Serum testosterone level (ng/mL) of ciprofloxacin groups following administration in 14th day of experiment and 56 days after last ciprofloxacin dose (30 mg/kg) (10th week).
4. Discussion
Ciprofloxacin is a wide spectrum antibiotic used for genitourinary tract infections. This broad-spectrum antibiotic can enter into the seminal fluid and cause toxicological effects on male reproductive organs. This antibiotic inhibits DNA gyrase and topoisomerase Ⅳthat are need for replication of prokaryotic DNA[14,15]. The common side effects of all quinolones are nausea, vomiting, dizziness and convulsions[16]. Some other ciprofloxacin adverse effects were described in the male reproductive system[8,9]. In the present study, a potential reversible testicular toxicity of ciprofloxacin was demonstrated in the rabbit model 56 days after last dose of ciprofloxacin administration. The cycle of the spermatogenesis in rabbit is 48 days. Therefore, sperm quality remains in low quality until the regeneration of damaged seminiferous tubules be completed.
Previously, some researchers reported that ciprofloxacin is a safe antibiotic[17]. In the study of Waite et al, the effects of ciprofloxacin(500 mg orally every 12 h for 4 days) on the cortisol and testosterone concentrations were investigated in the eight healthy men. Similar to our study, it was concluded that a low dose of ciprofloxacin does not have any anti-androgenic side effects and testosterone concentration was not significantly different from the control group after the first and last doses of ciprofloxacin[17]. Furthermore, fewin vivostudies described that ciprofloxacin is a proper drug without breakage or disruption in DNA[18].
In some studies, ciprofloxacin administration did not change the blood testosterone level. It may show this antibiotic inhibits mixedfunction oxidase and affects activities of necessary enzymes for metabolism of some substrates such as theophyiline and antipyrine,but the activities of responsible enzymes in synthesis of testosterone are not affected[17]. Conversely, some studies revealed that ciprofloxacin causes disorders in testicular function and structure in rats[19] that changes the level of serum testosterone[20]. Zobeiriet aldescribed that ciprofloxacin decreases the steroidal activity of the Leydig cells and leads to an imbalance of gonadotropins and testosterone in blood[21]. Leydig cells synthesize testosterone and control physiological functions of Sertoli cells. Elias and Nelson showed ciprofloxacin decreases testis weight, sperm count and significantly reduces testosterone level according to dose and time in guinea pig[8]. Khakiet alshowed oral usage of 12.5 mg/kg ciprofloxacin for 60 days significantly decreases spermatogenic cells,motility, viability, sperm concentration, and increases apoptosis of germ cells[9]. In addition, other parts of the genital system including epididymis, seminal vesicles and prostate can be damaged[22].
Production of peroxide radicals may be responsible for the disadvantage effects of ciprofloxacin in the testis[20].In vitrogenotoxicity investigations show this antibiotic breaks DNA singlestrand and makes deviations in chromosome[23,24]. Ciprofloxacin increases apoptosis by activation of caspase-3[25,26]. Zobeiriet alreported that ciprofloxacin (206 mg/kg,p.o.for 45 consecutive days) causes severe damages to DNA of immature sperm cells and results in karyorrhexis, vacuolation of primary spermatocyte and degenerative alterations in germ cells. These injuries decrease fertility and embryonic development of testis[27].
The World Health Organization recognizes that CASA offers improved precision over manual methods and can now be applied to routine analyses such as sperm counts, provided both adequate quality control procedures and high measurement standards are followed[28]. Accordingly, in the present study, CASA was used for the evaluation of ciprofloxacin treatment effects on sperm quality parameters. In the present study, all sperm quality parameters evaluated by CASA significantly reduced 56 days after discontinuation of ciprofloxacin medication. This decline in quality was a result of disruption of the spermatogenesis process, which is clearly identified in the pathology assessment. There are several studies in the literature that confirm the results of our work[9,12,29,30].Khakiet alobserved that administration of ciprofloxacin at dose of 12.5 mg/kg for two months had a severe disruptive effect on sperm concentration, motility and viability in male rats[9]. In addition,ciprofloxacin can lead to the damage of DNA content of sperm head and subsequent reduction of embryonic quality[27]. It is also clearly shown that sperm DNA damage is correlated with poor sperm quality parameters[31].
In conclusion, we describe the pathological findings of ciprofloxacin in the present study, which are associated with testicular damages. Our results suggest potential testicular toxicity for ciprofloxacin.
Conflict of interest statement
All the authors declare that there is no conflict of interest.
Funding
This work was supported by Shahid Bahonar University of Kerman and funded by grant number (AZ-91-11).
Authors’ contributions
Reza Kheirandish and Shahrzad Azizi conducted pathological evaluations; Ladan Emadi and Baharak Akhtardanesh made the study design and sperm quality assessment; Masoud Imani made revisions to the paper; Fatemeh Mahmoodabadi, Fereshteh Irani and Homa Shokrizadeh made practical procedure.
杂志排行
Asian Pacific Journal of Reproduction的其它文章
- Erectile dysfunction and statins: The assorted view of preponderance
- Effect of routine iron supplementation on copper level and oxidative stress status in pregnant women
- Effect of short-term gavage of ethanolic extract of cogon grass (Imperata cylindrica L)root on the ovarian activity and estrus behavior of female mice
- Effect of aqueous seed extract of Mucuna pruriens on arsenic-induced testicular toxicity in mice
- Influence of N-acetylcysteine on pituitary-gonadal axis hormones and protamine expression level in streptozotocin-induced diabetic male rats
- Influence of butylated hydroxytoluene addition to cryodiluents on freezability and DNA integrity of Boer and Zaraibi buck spermatozoa
