综合性康复训练对缺氧缺血性脑病早产儿患者智能及神经系统发育的影响
2020-04-05王秀娟叶金丹吴岸敏王丽珍
王秀娟 叶金丹 吴岸敏 王丽珍

[摘要] 目的 探討综合性康复训练对缺氧缺血性脑病早产儿患者智能及神经系统发育的影响。 方法 选取2013年1月~2017年2月该院儿科治疗HIE早产儿共150例,根据家长是否积极参与康复锻炼分为康复组114例与对照组36例。两组早产儿早期均予吸氧、控制惊厥、降颅压、控制血压、血糖和营养神经等基础治疗。对照组早产儿予以育儿指导、病情监测、门诊复查及父母心理干预等常规干预。康复组早产儿在对照组治疗基础上给予综合性康复训练。两组均干预24个月。观察两组早产儿干预前后智能发育指标及神经元特异性烯醇化酶(NSE)变化,并比较两组神经系统后遗症。 结果 干预12个月和24个月后,康复组早产儿适应能力、语言能力、精细运动能力、大运动能力和社交能力等智能发育评分均明显高于对照组(P<0.05)。干预24个月后,两组早产儿血清NSE水平均较干预前显著下降(P<0.05或P<0.01),且康复组早产儿下降幅度更显著(P<0.05);且康复组神经系统后遗症发生率为5.26%(6/114),明显低于对照组的19.44%(7/36)(χ2=4.06,P<0.05)。 结论 综合性康复训练用于HIE早产儿可减少中枢神经系统损伤,促进智能及神经系统发育,开发患儿潜在潜能,降低神经系统后遗症发生率,改善预后。
[关键词] 早产儿;缺氧缺血性脑病;综合性康复训练;智能发育;神经系统发育
[中图分类号] R742 [文献标识码] B [文章编号] 1673-9701(2020)04-0094-04
Effect of comprehensive rehabilitation training on intelligence and nervous system development in premature infants with hypoxic ischemic encephalopathy
WANG Xiujuan1 YE Jindan2 WU Anmin1 WANG Lizhen1
1.Department of Pediatric Internal Medicine, Taizhou Hospital of Taizhou Enze Medical Center (Group) in Zhejiang Province, Linhai 317000, China; 2.Department of Hematology and Oncology, Taizhou Hospital of Taizhou Enze Medical Center (Group) in Zhejiang Province, Linhai 317000, China
[Abstract] Objective To investigate the effects of comprehensive rehabilitation training on the intelligence and nervous system development of premature infants with hypoxic ischemic encephalopathy. Methods A total of 150 children with HIE premature infants in pediatric department of our hospital from January 2013 to February 2017 were enrolled. According to whether the parents actively participated in rehabilitation exercises,the children were divided into 114 patients in the rehabilitation group and 36 patients in the control group. Both groups of preterm infants were given basic treatment including oxygen therapy, control of convulsions, reduction of intracranial pressure, control of blood pressure and blood sugar, and nutrition for nerves. Premature infants in the control group were given routine interventions such as parenting guidance, condition monitoring, outpatient review, and parental psychological intervention. Premature infants in the rehabilitation group were given comprehensive rehabilitation training based on the treatment of the control group.Both groups were treated for 24 months. The changes of intelligent development index and neuron-specific enolase(NSE) before and after intervention in the premature infants of the two groups were observed, and the sequelae of the nervous system were compared. Results After 12 months and 24 months of intervention, the intelligent development scores of adaptablity, language ability, fine motor ability, large exercise capacity and social ability in the rehabilitation group were significantly higher than those in the control group(P<0.05). After 24 months of intervention, the serum NSE levels of the preterm infants in the two groups were significantly lower than those before the intervention(P<0.05 or P<0.01), and the decrease rate of preterm infants in the rehabilitation group was more significant (P<0.05). And the neurological sequelae occurrence rate in the rehabilitation group was 5.26%(6/114), which was significantly lower than that of the control group (19.44% (7/36)(χ2=4.06, P<0.05). Conclusion Comprehensive rehabilitation training for HIE premature infants can reduce central nervous system damage, promote intelligence and nervous system development, develop potential of children, reduce the incidence of neurological sequelae, and improve prognosis.
[Key words] Premature infants; Hypoxic ischemic encephalopathy; Comprehensive rehabilitation training; Intelligent development; Nervous system development
缺氧缺血性脑病(hypoxic ischemic encephalopathy,HIE)是新生儿,尤其是早产儿常见的危重神经系统疾病之一,主要是由于围产期窒息与产伤引起,治疗后部分患儿会遗留下永久的神经伤残率和智能障碍,对社会和家庭带来了沉重的负担[1,2]。随着围生医学的迅速发展,HIE早产儿的存活率明显上升,但后遗症的发生率仍居高不下,因此,在保证成活率的同时降低后遗症的发生是临床迫切需要解决的问题[3,4]。研究已证实2岁前儿童的中枢神经系统发育较迅速,此时可塑性和代偿功能亦最强,此段时间予以积极有效康复锻炼对其中枢神经系统发育具有积极作用[5,6]。为此,本研究分析了综合性康复训练对HIE早产儿智能及神经系统发育的影响,现报道如下。
1 资料与方法
1.1 一般资料
选择2013年1月~2017年2月期间在我科就诊HIE早产儿150例。纳入标准[7]:(1)符合HIE的诊断标准[8];(2)均胎儿宫内或分娩过程中有窘迫或明显窒息史,且具有典型表现。排除标准[9]:伴先天性畸形或遗传代谢性疾病引起的脑损伤。根据家长是否积极参与康复锻炼情况将150例HIE早产儿分为康复组114例与对照组36例。两组HIE早产儿在性别、胎龄、体重、Apgar评分和病情等方面均衡可比(P>0.05)。见表1。
1.2 治疗方法
两组HIE早产儿早期均予吸氧、控制惊厥、控制颅压、维持血压、血糖和营养神经等基础治疗。对照组早产儿给予育儿指导、病情监测、定期门诊复查及父母心理干预等常规干预。康复组早产儿给予综合性康复训练,内容包括:(1)视觉康复训练:用颜色鲜艳的物品放在患儿眼前20~25 cm处,引逗小儿的注意以训练视觉功能,15 min/次,3次/d;(2)听觉康复训练:重复播放轻音乐、钟声、铃声等方式训练患儿听觉功能,20 min/次,3次/d;(3)触觉康复训练:通过被动屈曲患儿四肢、变换患儿姿势、以奶嘴接触患儿口唇等方式使患儿作出吸吮、觅食等动作以训练触觉功能;(4)运动康复训练:予以肢体曲伸,诱导患儿伸手、抓握蹬腿、被动伸展肢体等主被动训练来训练运动功能。两组早产儿均干预24个月。
1.3 观察指标
观察两组早产儿干预前后智能发育指标及神经元特异性烯醇化酶(NSE)變化,并比较神经系统后遗症情况。
1.3.1 智能发育评估指标[10] 采用Gesell量表评估其智能发育情况,包括精细运动能力、社交能力、适应能力、语言能力和大运动能力等五项,每项100分,分数越高提示智能发育越好。
1.3.2 血清NSE水平测定 采集静脉血1~2 mL,低温离心分离出血清,冻存于-70℃冰箱,采用酶联免疫吸附法(试剂盒由美国R&D公司提供)测定血清NSE水平。
1.3.3 神经系统后遗症 包括癫痫、运动障碍、脑瘫、智力障碍、共济失调和语言障碍等。
1.4 统计学处理
采用软件SPSS18.0分析数据,计量资料用均数±标准差(x±s)表示,采用t检验,计数资料用[n(%)]表示,采用χ2检验,P<0.05为差异有统计学意义。
2 结果
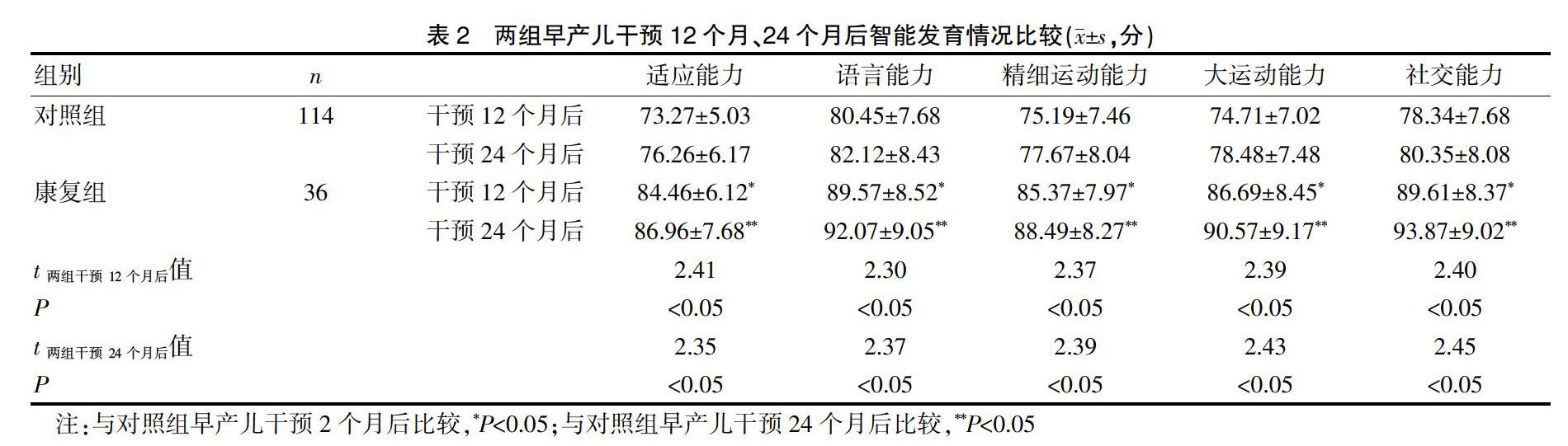
2.1 两组早产儿干预后智能发育情况比较
干预12个月和24个月后,康复组早产儿的适应能力、语言能力、精细运动能力、大运动能力和社交能力等智能发育评分明显高于对照组(P<0.05)。见表2。2.2 两组早产儿血清NSE水平比较
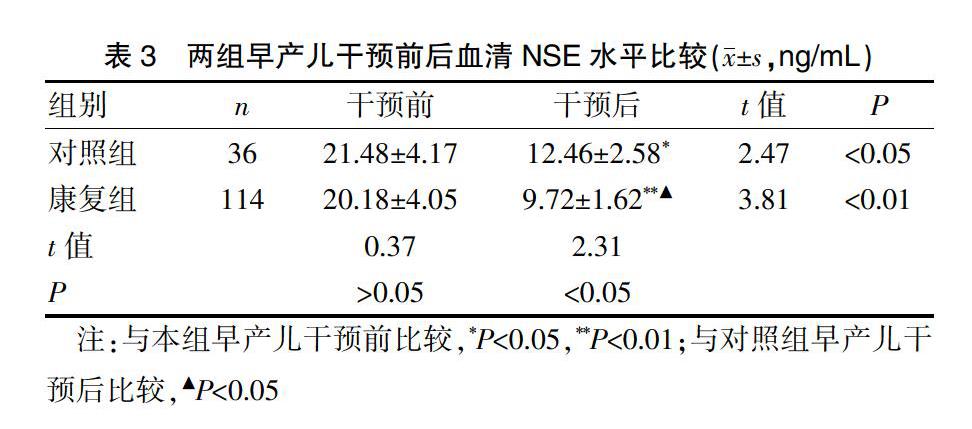
两组早产儿干预前血清NSE水平比较,差异无统计学意义(P>0.05)。干预24个月后,两组早产儿血清NSE水平较前显著下降(P<0.05或P<0.01),且康复组早产儿下降幅度更显著(P<0.05)。见表3。
2.3 两组早产儿神经系统后遗症比较
干预24个月,康复组早产儿神经系统后遗症发生率为5.26%(6/114),明显低于对照组的19.44%(7/36)(χ2=4.06,P<0.05)。见表4。
3 讨论
HIE是新生儿,尤其是早产儿在宫内窒息后发生常见且较严重的神经系统并发症,小部分患儿虽经积极有效干预治疗后仍遗留一些神经系统的后遗症,是导致儿童神经系统残疾的常见原因[11,12]。以往对HIE早产儿处理首先考虑的是早期生命的抢救,而对HIE早产儿治疗后遗留的神经系统后遗症往往忽视。随着医学的进步,改善HIE早产儿的预后,减轻或避免神经系统后遗症日益受临床关注[13,14]。目前HIE的发病机制迄今国内外尚未完全研究透彻,近年来研究发现反映颅内组织细胞病理损伤的早期特异性指标如NSE在HIE发病中起及其重要作用[15]。NSE是中枢神经系统损伤的特异性敏感指标。当中枢神经系统发生缺血、缺氧改变时引起中枢神经细胞会发生变性坏死和髓鞘崩解,破坏了脑部神经细胞膜的完整性,胞浆内的NSE可溢出神经细胞大量进入脑脊液,并通过受损血-脑屏障释放进入外周血中,引起血清NSE水平异常升高,因此,血清NSE水平可反映中枢神经系统损伤的程度,可作为评估HIE患儿治疗效果的指标[16,17]。
2岁前儿童正处于大脑系统发育核心期和快速期,具有较高的可塑性,代偿性和重组能力较强,此时脑细胞具有特殊功能变更,通过轴突绕道投射、桥接和重组,树突出现不寻常分叉或发生非常规的神经突触等方式代替临近受损细胞的功能[18,19],如此期间为患儿予以积极有效的康复锻炼,可激活神经细胞并提高其兴奋性,有利于神经轴突及树突的形成及加快神经纤维发生髓鞘化,这不仅有利于受损的脑细胞发生功能性适应,而且使得周围神经细胞发生功能代偿,减少或避免中枢神经细胞发生损伤,有利于神经细胞的修复及再生[20-22]。综合性康复训练对HIE早产儿的干预主要通过视觉、听觉、触觉和运动等康复训练进行刺激,通过外周感受器传导进入中枢神经系统,能刺激人体脑细胞发生修复与再生,有利于受损脑细胞功能发生代偿,从而使脑细胞逐渐恢复并促进其正常发育,有利于肌肉及肢体运动的协调性;而良好的肢体运动功能锻炼又可促进脑细胞的生长发育,进一步加快受损神经功能的恢复过程,促进智力、运动和语言功能的发育,减少神经伤残率,逐渐发生良性循环,改善预后[23-24]。本研究显示,干预12个月和24个月后,康复组HIE早产儿的适应能力、语言能力、精细运动能力、大运动能力和社交能力等智能发育评分明显高于对照组,提示综合性康复训练用于HIE早产儿可促进智能发育,开发患儿潜在潜能。同时研究发现干预24个月后,康复组血清NSE水平下降的幅度较对照组更明显,且神经系统后遗症发生率较对照组更低。提示综合性康复训练用于HIE早产儿可减少或避免中枢神经受损,使得神经系统后遗症发生率更低。
总之,综合性康复训练用于HIE早产儿可减少中枢神经系统损伤,促进智能及神经系统发育,开发患儿潜在潜能,减少神经伤残率,改善其预后。但本研究纳入的样本量相对较小,研究所得结果和结论还需进一步通过扩大样本量进行深入研究探讨证实。
[参考文献]
[1] Gunn AJ,Wyatt JS,Whitelaw A,et al.Therapeutic hypothermia changes the prognostic value of clinical evaluation of neonatal encephalopathy[J].J Pediatr,2008,152(1):55-58.
[2] Olivieri I,Bova SM,Urgesi C,et al. Outcome of extremely low birth weight infants:Whats new in the third millennium? Neuropsychological profiles at four years[J]. Early Hum Dev,2012,88(4):241-250.
[3] Alvarez-Diaz A,Hilario E,de Cerio FG,et al. Hypoxic-ischemic injury in the immature brain-key vascular and cellular players[J]. Neonatology,2007,92(4):227-235.
[4] Douglas-Escobar M,Weiss MD. Hypoxic-ischemic encephalopathy:A review for the clinician[J].Jama Pediatrics,2015,169(4):397-403.
[5] Titomanlio L,Kavelaars A,Dalous J,et al. Stem cell therapy for neonatal brain injury:Perspectives and challenges[J].Ann Neurol,2011,70(5):698-712.
[6] Kolb B,Gibb R.Brain plasticity and behaviour in the developing brain[J]. J Can Acad Child Adolesc Psychiatry,2011,20(4):265-276
[7] Shetty J.Neonatal seizures in hypoxic-ischaemic encepha-lopathy risks and benefits of anticonvulsant therapy[J].Developmental Medicine & Child Neurology,2015, 57(S3):40-43.
[8] 中華医学会儿科学分会新生儿学组.新生儿缺氧缺血性脑病诊断标准[J].中华当代儿科杂志,2005,7(2):97-98.
[9] Benjamin Y,Castillo M. Hypoxic-ischemic brain injury:Imaging findings from birth to adulthood[J].Radiographics,2008,28(2):417-439.
[10] 刘敬,杨于嘉,封志纯.“早产儿脑损伤诊断与防治专家共识”解读[J].中国当代儿科杂志,2012,14(7):885-887.
[11] Logitharajah P,Rutherford MA,Cowan FM. Hypoxic-ischemic encephalopathy in preterm infants:Antecedent factors,brain imaging,and outcome[J].Pediatric Research,2009,66(2):222 -229.
[12] Nancy Fathali,Nikan H,Khatibi,et al.The evolving landscape of neuroinflammation after neonatal hypoxia- ischemia[J].Acta Neurochir Suppl,2011,111(111):93-100.
[13] Dixon BJ,Reis C,Ho WM,et al. Neuroprotective strategies after neonatal hypoxic ischemic encephalopathy[J].International Journal of Molecular Sciences,2015,16(9):22368-22401.
[14] 邵肖梅.新生儿缺氧缺血性脑病的诊治进展及相应问题[J].临床儿科杂志,2007,25(3):179-182.
[15] Douglasescobar M,Weiss MD.Biomarkers of hypoxic-ischemic encephalopathy in newborns[J].Frontiers in Neurology,2012,11(3):144-154.
[16] 钱庆燕,童仁香,王菊,等.神经元特异性烯醇化酶在新生儿缺氧缺血性脑病中的诊断价值[J].重庆医学,2016, 45(18):2516-2517.
[17] 王世界,李操,李明星.回顾性分析 43 例足月窒息新生儿脑血流动力学与血清神经元特异性烯醇化酶(S-NSE)动态变化的临床意义[J].中国临床医学影像杂志,2017,28(7): 466-470.
[18] 李墨,何靜雅.早期综合康复治疗对缺氧缺血性脑病新生儿神经系统后遗症及生活质量的影响[J].中国实用神经疾病杂志,2014,17(12):70-72.
[19] McManus BM,Carle AC,Poehlmann J. Effectiveness of part C early intervention physical,occupational,and speech therapy services for preterm or low birth weight infants in Wisconsin,United States[J].Acad Pediatr,2012, 12(2):96-103.
[20] Gulczynska E,Kesiak M,Kryszczynska J,et al.The first application of therapeutic hypothermia in Poland- selective head cooling(Cool-Cap) with whole- body moderate hypothermia in a newborn with features of hypoxic ischemic encephalopathy[J]. Ginekol Pol,2012,83(5):384-387.
[21] Baroncelli L,Braschi C,Maffei L.Visual depth perception in normal and deprived rats:Effects of environmental enrichment[J].Neuroscience,2013,236(3): 313-319.
[22] De Bruine FT,van den Berg-Huysmans AA,Leijser LM,et al. Clinical implications of MR imaging findings in the white matter in very preterm infants:A 2-year follow-up study[J].Radiology,2011,261(3):899-906.
[23] Holt RL,Mikati MA.Care for child development:Basic science rationale and effects of interventions[J].Pediatr Neurol,2011,44(4):239-253.
[24] Cioni G,D'Acunto G,Guzzetta A.Perinatal brain damage in children:neuroplasticity,early intervention,and molecular mechanisms of recovery[J]. Prong Brain Res,2011, 189(2):139-154.
(收稿日期:2019-06-14)
