Evaluation of the changes in choroidal thickness in patients with central serous chorioretinopathy as measured by optical coherence tomography
2020-04-04
Abstract
INTRODUCTION
Central serous chorioretinopathy (CSCR) is mostly a middle-aged disease that affects predominantly men. It is considered as a benign condition that ends almost in spontaneous complete resolution over a period of 3mo with good visual prognosis[1].
CSCR is defined as an area of well-defined serous neurosensory retinal detachment in the posterior pole[2]with leakage of subretinal fluid through the damaged retinal pigment epithelium (RPE)[3].
The pathophysiology is not fully established and includes abnormal ion transport across the RPE as well as focal choroidal vasculopathy. Indocyanine green (ICG) angiography has shown the importance of the choroidal circulation to the pathogenesis of CSCR. Increased choroidal hyper-permeability and focal choroidal vascular compromise are believed to lead to secondary dysfunction of the overlying RPE[4-5].
CSCR can be divided into 2 clinical presentations. Classic CSCR: one or two isolated leaking points at the level of the RPE as seen on fluorescein angiography (FA). Diffuse: characterized by neurosensory retinal detachment over areas of RPE atrophy and pigment mottling. Areas of granular hyperfluorescence that contain one or many subtle leaks are seen using FA as seen in diffuse retinal pigment epithelial dysfunction (e.g. diffuse retinal pigment epitheliopathy, chronic CSCR, decompensated RPE). “The retinal function imager RFI was used to detect a reduced flow velocity in the retinal venules, whilst the arterial flow velocity measurements were not significantly altered”[6]. The baseline subfoveal and temporal CT may have a predictive value for chronicity[7].
Progress in retinal imaging has led to the discovery of a variety of chorioretinal disorders. The use of enhanced depth imaging (EDI) and swept source OCT technologies have enabled a precise qualitative and quantitative analysis of the choroid[8-9]. Pachychoroid a term that indicates abnormal and permanent increase in choroidal thickness. This entity usually occurs in eyes with central serous chorioretinopathy (CSCR) or CSCR-like features[10]. Pachychoroid often shows dilatation of the large choroidal vessels compressing the overlying choriocapillaris and Sattler’s layer[11].
In this study, we measured the choroidal thickness (CT), using spectral-domain optical coherence tomography (SD-OCT) in acute unilateral CSCR patients and compared it to the fellow unaffected eye and a healthy control group. We aimed to reveal the differences in the CT during the 3-month follow-up and whether these differences can be related to the disease as a step to understand the role of the choroid in pathogenesis and course of this disease. The increased choroidal thickness in the fellow eye at the time of the acute attack and its significant increase compared to the normal eye confirms the presence of pachychoroid in both eyes and can predict that the fellow eye is more prone to develop CSR than eyes of normal people.
SUBJECTS AND METHODS
The study was approved by the Ethical Committee of Fayoum University. A consent of approval was signed by each patient. The study was prospective, included 60 eyes; both eyes of 20 patients and 20 eyes of healthy volunteers acting as controls during the period from September 2016 to March 2017.
The study has followed the Tenets of the Declaration of Helsinki.All patients received a comprehensive full ophthalmological examination that would lead to the diagnosis of CSCR including refraction, visual acuity, best corrected visual acuity, slit lamp biomicroscopy, intraocular pressure measurements, dilated fundus examination, fundus photography, fluorescein angiography and OCT.
Inclusion criteria: patients with classic CSCR with duration less than one month with normal fellow eye.
ExclusionCriteriaPatients with bilateral CSCR, other cause of CSCR as CNV, pigment epitheliopathy and chronic CSCR, also patients receiving any medical treatment that may affect the course of the disease as corticosteroids as well as patients with refraction more than -2.00 dioptres. These cases were excluded to limit the analysis to only one pathological disease; acute CSCR and eliminate other factors that may affect the thickness. Choroidal thickness in different degrees of myopia is significantly thinner than that of normal control eyes[12].
The study was subdivided into 3 groups: Group 1 included 20 eyes with CSCR; Group 2 included 20 fellow eyes and Group 3 included 20 eyes of normal controls.
A three-dimensional SD-OCT system, the RTVue XR Avanti with AngioVue software for OCTA (Optovue, Inc., Fremont, CA), was used to measure the subfoveal choroidal thickness and to measure central macular thickness CMT in eyes with CSCR. This system has optical resolution of 5 μm depth resolution and 15 μm beam spot with image sample rate of 2.9 μm depth and 8 μm transverse. Three-dimensional data were obtained using the Raster and HD line scan centred on the fovea, covering an area measuring 6 mm horizontal, 6 mm vertical, and 1.7 mm axial depth. The imaging data were obtained using the split spectrum amplitude-decorrelation angiography (SSADA) software. The choroidal thickness was measured from the outer portion of the hyper reflective line corresponding to the RPE to the chorioscleral junction at three different locations: at the centre of the fovea, 1000 μm temporal to the centre of the fovea and 1000 μm nasal to the centre of the fovea. The subretinal fluid was measured manually using callipers.
StatisticalAnalysisThe collected data was organized, tabulated and statistically analyzed using SPSS software statistical computer package version 18 (SPSS Inc, USA). For quantitative data, the mean and standard deviation were calculated. Comparison between 2 study groups as regards age was done usingt-test. One way analysis of variance (ANOVA) followed by least significance difference LSD (post hoc test) was performed to compare between the three eyes groups regarding values of choroid thickness in different locations at different times. Within each group,t-test was used to test the difference changes in choroid thickness in different locations at different times. Sex was described as frequencies (number of cases) and percentages; Chi-square test was used as a test of significance. For interpretation of results of tests of significance, significance was adopted atP≤0.05.
RESULTS
The study included 40 eyes of 20 patients and 20 eyes of healthy volunteers, with total of 60 eyes divided into 3 groups.
The mean age of the patients was 33.65±5.24 years, 15 males and 5 females. All patients suffered from acute, unilateral CSCR. All of them have shown complete recovery with disappearance of subretinal fluid except for 4 patients at the end of the follow-up period.

Figure 1 A: OCT of the affected eye showing measurements at the three locations; B: After 3mo follow-up; C: FFA showing the ink blot leaking point.
At baseline, the mean subfoveal choroidal thickness of affected eyes (Group 1) was 372.40±34.39 μm after the 3-month follow-up period; the mean thickness was 337.0±35.9 μm with a statistically significant decrease (P<0.001). At the temporal location the mean thickness was 353.00±29.85 μm and decrease to a mean of 318.4±24.96 μm at 3mo follow-up; a change that was statistically significant (P<0.001). The mean thickness at the nasal location was 351.20±29.98 μm and decrease to a mean of 312.05±17.01 μm at 3mo follow-up with a statistically significant change (P<0.001). Figure 1 shows the representative images of the group while Figure 2 shows the average choroidal thickness at each location.
In fellow eyes(Group 2) at baseline, the mean subfoveal choroidal thickness was 302.10±8.9 μm after 3mo and the mean thickness was 299.55±8.7 μm; a decrease that was statistically significant (P<0.001). At the temporal location, the mean thickness was 283.55±7.1 μm and change to a mean of 287.75±23.37 μm; a changes that was statistically insignificant (P<0.408). At the Nasal location the mean thickness was 280.60±7.18 μm and decrease to a mean of 280.30±7.66 μm at 3mo follow-up; a changes that was not statistically significant (P<0.868). The representative image of the group is shown in Figure 3 while Figure 4 demonstrates the average choroidal thickness at each location.
Thickness of the choroid varied with location, with the maximum thickness at the centre of the fovea. There were statistical significant difference between Groups 1 and 2 at the three different locations at time of presentation and at the end of the follow-up period (P<0.001).
Healthy control group: the mean age of the control group was 31.35±4.23 years (15 males, 5 females) with no history of ophthalmological complaints.
At baseline, the mean subfoveal choroidal thickness was 279.80±14.49 μm. After the 3-month follow-up period, the average thickness was 279.30±13.67 μm a decrease that was not statistically significant (P<0.415). At the temporal location, the mean thickness was 272.75±16.17 μm and decrease to 271.80±15.52 μm at 3mo; a change that was statistically insignificant (P<0.081). The mean thickness at the nasal location was 270.24±15.52 μm. It decreased to a mean of 269.40±15.96 μm at 3mo, a change that was not statistically significant (P<0.077).

Figure 2 Mean choroidal thickness at the three locations of the affected eyes.

Figure 3 Measurements at the three locations of the unaffected eye.
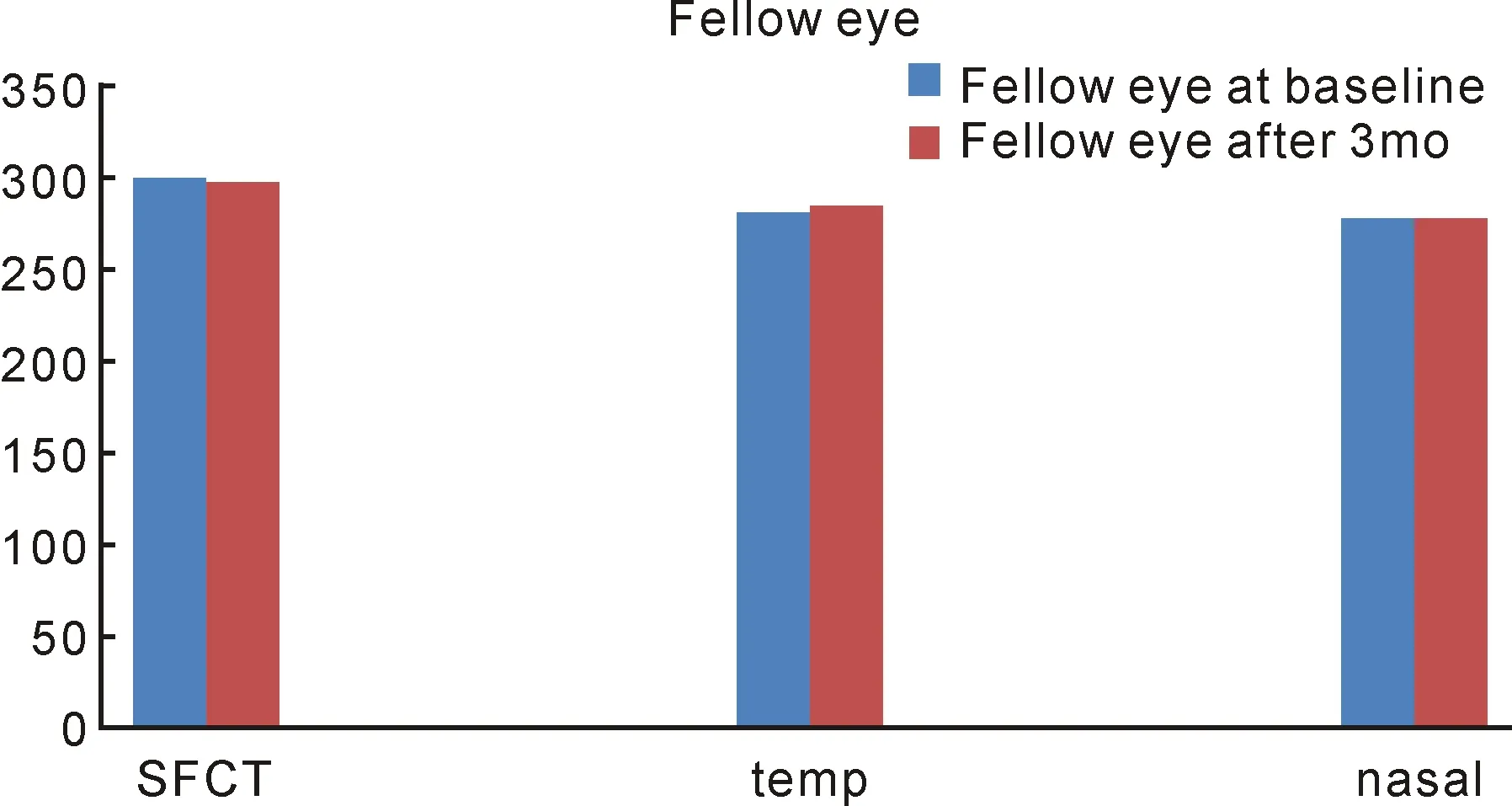
Figure 4 Mean choroidal thickness at different locations of the fellow eyes.
Figure 5 shows the representative images of the group while the average choroidal thickness at each location is shown in Figure 6.
There was a statistically significant difference in SFCT among the three groups at the three different locations. SFCT in eyes with CSCR was significantly greater than that in each of the unaffected fellow eyes (P<0.001) and normal control eyes (P<0.001) at the base line but with no statistically significant difference in SFCT between the unaffected fellow eyes and normal control eyes (P>0.05) at the end of follow up period (results are shown in Figure 7). The relation among the 3 groups at the baseline and after 3mo follow-up are shown in Table 1. There were no statically significant changes between the baseline and the follow-up measurements in Groups 2 and 3 except for the CT at the temporal and nasal locations in the fellow eye that showed statistically significant decrease at the end of the follow-up period (P<0.05).

Figure 5 The measurements at the three locations in the control group.

Figure 6 Mean choroidal thickness of the healthy control group at different locations.
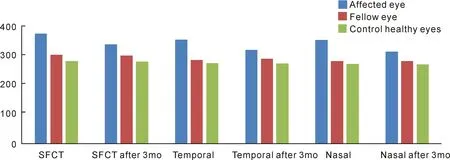
Figure 7 The measurements of the choroidal thickness among the three groups at the three locations after 3mo follow-up.

Table 1 The measurements of the choroidal thickness among the three groups at the three locations after 3mo(n=20)
Group 1: Affected eyes; Group 2: Fellow eyes; Group 3: Healthy control eyes; SFCT: Subfoveal choroidal thickness.
The serous retinal detachment, was manually measured in Group 1 eyes with CSCR to determine whether there was a correlation between SFCT and CMT. The mean CMT in eyes with CSCR was 317±141.86 μm with a range from 130 to 619 μm, and there was a statistically significant positive correlation between SFCT and CMT in these eyes (P<0.001).
DISCUSSION
The study aimed to evaluate the role of choroid in the pathogenesis of the CSCR through measuring choroidal thickness in the subfoveal area and whether an increase in the thickness can be related to the disease. This was done by measuring the thickness of the affected eye and compared it to the fellow unaffected eye and to the normal choroidal thickness through a healthy control group using the OCT. Different levels of visual function may be related to structural OCT changes, and OCT findings could be important parameters for both follow-up and treatment[13].
In this study, the mean SFCT of eyes with CSCR was significantly greater than that in the unaffected fellow eyes and in normal control eyes, as well as between unaffected fellow eyes and normal control eyes and between the fellow and normal eyes. These results matched with Chungetal[14]where the subfoveal choroidal thickness and the thickness of Haller layer were greater in the affected and the unaffected fellow eyes compared to normal eyes. Regatierietal[15]reported that choroid in older patients, older than 60 years old with active CSCR was thicker than the choroid in age-matched normal eyes. The results of the current study were also in agreement with other studies; Goktas[3], Dangetal[16], and Yangetal[17], concluding that the mean SFCT in symptomatic eyes with CSCR is significantly greater than that in fellow eye and control group. Other studies demonstrated that SFCT was increased in CSCR eyes, as well as in unaffected fellow eyes, thus suggesting that CSCR may be a bilateral disorder. The frequency of the bilaterality is reported at 20% to 40%[18-19]. The data of Brandletal[20]and associates indicated that after 3mo, normalisation of choroidal thickness was not yet completed.
In fellow eyes (Group 2: unaffected eyes), the mean subfoveal choroidal thickness at baseline was 302.10±8.9 μm while after the 3-month follow-up period the mean thickness was 299.55±8.7 μm; a decrease that was statistically significant (P<0.001). That what statistically significant is not necessarily clinically significant. The sample size and random variation play an important role in whether a result is statistically significant or not and, together with the effect size, whether the study is “powered” to detect statistical differences[21]. In our study, although the observed differences were tiny, the results were statistically significant. These findings may be attributed to the low variability of the individual values around their average, which can be identified as low standard deviation.
While Jirarattanasopaetal[22]found the macular choroidal thickness in unaffected fellow eyes less than that the CSCR eyes but it did not differ from normal control eyes. Dansinganietal[23]in another study by using swept-source OCTenfaceimaging of patients with pachychoroid found dilated choroidal vessels in eyes without manifest pathology, projecting that pachychoroid is a bilateral phenomenon with a systemic basis.
The current study measured the SFCT at three different locations, at thecenter of the fovea, 1000 μm temporal and 1000 μm nasal to the center of the fovea and the measurements showed significant increase in the thickness in eyes with CSCR as compared to the unaffected and control eyes. These results were in agreement with Kimetal[24]who measured the choroidal thicknesses at five points (centre of the fovea, 500 μm, 1000 μm and 1500 μm temporal and nasal to the fovea) and showed them significantly higher for CSCR eyes than for controls at all locations. Manabeetal[25]measured the choroidal thickness at a wider area by using inner and outer circle of the macula in active chronic CSCR and found them significantly greater than in normal controls.
The current study evaluated the SFCT after three months follow-up which have seen almost spontaneous total resolution in 16 cases and a near totalresolution in the other 4 cases. Among the three groups: a decrease in the choroidal thickness at the three locations was noted but was only statistically significant in the group with the affected eye (Group 1) which suggest the basic role of the choroidal circulation in the pathogenesis of CSCR. A follow-up study by Kangetal[26]of CSCR eyes found a decrease by about -9% in the SFCT after a spontaneous resolution but not returning to normal values suggesting a threshold of choroidal thickness above which accumulation of subretinal fluid starts to occur.
In the current study measurements of the choroidal thickness were taken from 10 a.m. to 2 p.m. to avoid the circadian pattern that may affect the outcome of study, as previous studies showed that choroidal thickness presents higher level at night and lower level during the day in young adults[27-29].
The current study also investigated the correlation between SFCT and CMT, including elevation of the serous retinal detachment, in eyes with CSCR and found a significant positive correlation. Iijimaetal[5], instead, studied the correlation of SFCT and subretinal fluid volume, which was estimated using a built-in segmentation-modifying tool of SD-OCT, and found no association between these two parameters in eyes with acute CSCR. Therefore, he suggested that formation of subretinal fluid might not solely be associated with choroidal vasculature and that some additional factors such as RPE dysfunction could have a role in the pathogenesis of CSCR, which might need further studies to clarify.
The results of this study was limited by the small number of cases as well as the manual measurement of the choroidal thickness as no automatic measures of mapping where available. A larger group of patients and a longer period of follow-up as well as a more advanced way in measuring the choroidal thickness would have added to our study. However, the accurate and reliable measurements of the choroidal thickness and the changes through the study that occurs during the process of the disease may be of great value in helping researchers to know more about the actual pathological nature of the disease.
The increase in the choroidal thickness as well as hyper-dilated and hyper-permeable vessels known as “pachychoroid” seems to play an important role in a broad spectrum of diseases that includes CSCR.
