Guidelines for the Diagnosis and Treatment of Psoriasis in China: 2019 Concise Edition#
2020-04-03CommitteeofPsoriasisDermatologyBranchChineseMedicalAssociation
Committee of Psoriasis, Dermatology Branch, Chinese Medical Association∗
Abstract Psoriasis is an immune-mediated chronic, recurrent, systemic inflammatory disease induced by the combination of hereditary and environmental factors.The etiology of psoriasis involves hereditary,immune,environmental,and other factors,and its pathogenesis is considered to involve excessive proliferation of keratinocytes or inflammatory activation of synovial cells and chondrocytes within joints; these processes are caused by an immune response that is mainly mediated by T lymphocytes and various other immune cells.Psoriasis is an incurable disease,and the goal of treatment is to control the progression of disease and maintain long-term efficacy.Treatment protocols should be based on the patients’conditions.Patients with mild psoriasis can be mainly treated with topical agents,and those with moderate to severe psoriasis can be treated with systemic medications.Targeted biological agents can be appropriately chosen for cases of psoriasis that are resistant to traditional systemic treatment.New drugs and treatments for psoriasis continue to evolve and emerge, and our updated guidelines are designed to deliver new achievements from China and physicians worldwide and to keep pace with global progress on psoriasis research.Compared with the previous two editions, part of contents have been modified and revised in the present guidelines; this will further facilitate standardization and increase the efficiency of the diagnosis and treatment of psoriasis in China,and improve patients’quality of life.
Keywords: psoriasis, guidelines, diagnosis, treatment, standardization, efficiency
Background for the guidelines compilation
Psoriasis is characterized by the local or extensive distribution of scaly erythema or plaques.The prevalence of psoriasis varies significantly worldwide and is associated with race, geographic area, and environment. Its prevalence in Europe and America is approximately 1%-3%.1-2The prevalence of psoriasis in China was 0.123%in 1984,3and the prevalence in nine Chinese cities was 0.47% according to a survey in 2008. Thus, approximately six million people are estimated to have psoriasis in China.4
Psoriasis can occur in all age groups without sex-related differences.Approximately 30%of patients have a family history,and most patients experience recurrent episodes or aggravation during winter and alleviation of the disease in summer.
Typical rashes are easy to diagnose. If physicians do not have a comprehensive understanding of psoriasis or lack a comprehensive ability to analyze its clinical signs, then misdiagnosis can readily occur.The treatment of psoriasis is challenging, and patients need lifelong medical care and treatment to control symptoms and improve their life quality.
According to the principles of evidence-based medicine and based on the 2008 edition of the “Guidelines for psoriasis management in China”, the Professional Committee on Psoriasis referenced the latest guidelines in China and other countries,took into account the situations across China, and invited authoritative experts in Western medicine and traditional Chinese medicine (TCM) to constituteacommitteeforthecompilationofnewguidelines anddevelop the“Guidelines for the diagnosis andtreatment of psoriasis in China”, These guidelines integrate the features of TCM treatments with the guidelines for the diagnosis and treatment of psoriasis in China.
Scope of application of the guideline and related statements
These guidelines have been established to guide dermatologists and other physicians involved in the diagnosis and treatment of psoriasis.During the compilation process,the greatest possible amount of current information regarding psoriasis diagnosis and treatment obtained from evidencebased medicine was included in the guidelines. However,because it is difficult to maintain consistency among the inclusion and exclusion criteria, the guidelines have room for improvement. Readers are welcome to provide constructive criticism and corrections. These concise guidelines are published only as a summary of the major ideas and principles that comprise the full edition of the guidelines, which has been published on Chinese Journal of Dermatology, 2019, 52(10):667-710. Readers are encouraged to gain new knowledge that will be available after the guidelines are published.
Etiology and pathogenesis of psoriasis
Neither the etiology nor the pathogenesis of psoriasis is completely clear. According to Western medicine, the etiology of this disease involves many factors, including genetics, immunology, and the environment. Psoriasis develops secondary to an immune response primarily mediated by T lymphocytes and involving various other types of immune cells, causing excessive proliferation of keratinocytes and inflammatory activation of synovial cells and chondrocytes within joints.
According to TCM, this disease is primarily associated with pathogeneses such as blazing heat toxin in the blood,a deficiency of nutrients in blood,stagnation of blood,wind dryness,and loss of nutrition in the skin and muscle.
Diagnosis, classification, and staging of psoriasis
The diagnosis of psoriasis in Western medicine is primarily based on classic findings of skin lesions (including the morphology, boundary, and distribution) and disease history (including the condition of disease onset, pattern of evolution, exacerbation, remission, accompanying symptoms,and treatment response)combined with family history.When necessary,diagnosis can be confirmed using histopathology and imaging technologies (e.g., dermatoscopy).Diagnosis and differential diagnosis of psoriasis can be determined following the procedure shown in Figure 1.
Psoriasis vulgaris
Guttate psoriasis
Guttate psoriasis is often the type of psoriasis with earliest onset. Its diagnosis is based on (1) an acute disease onset characterized by the development of extensively distributed red papular and maculopapular skin rashes covered with scales and measuring 0.3-0.5cm; (2) a history of streptococcal infection in the upper respiratory airway that precedes the disease onset;(3)increases in the white blood cell count,percentage of neutrophils,and anti-streptolysin O antibody; and (4) skin rashes that disappear within several weeks after proper treatment,although a few cases evolve to a chronic course.

Figure 1. Algorithm of psoriasis diagnosis and treatment. NSAID: non-steroidal anti-inflammatory drugs; DMARD: disease modifying antirheumatic drug.
Plaque psoriasis
Plaque psoriasis is the most common type of psoriasis and accounts for approximately 90%of all cases.Its diagnosis is based on(1)dark red plaques with sharp demarcation or infiltrating erythema covered by white and silver-white scales; (2) “wax spot phenomenon” and “last membrane phenomenon” (Auspitz sign), or clumped hairs; (3) skin rashes that primarily occur on the scalp, back, and extensional sides of the arms and legs with or without accompanying itching; (4) a progressive stage that shows the isomorphic response(i.e.,Koebner phenomenon);and(5) recurrent skin rashes, most of which are exacerbated during winter and relieved during summer.
Stages
1. Active stage: old rashes do not disappear, new rashes continuously appear, inflammation is obvious, redness might exist around the rashes,scales are thicker,and the isomorphic response occurs.
2. Stable stage: no new rash occurs, inflammation is milder, and more scales are present.
3. Regressive stage: rashes shrink or become flat, inflammation basically disappears,and residual hypopigmentation or hyperpigmentation spots appear.
Pustular psoriasis
Localized and generalized pustular psoriasis have the following diagnostic characteristics.
Localized pustular psoriasis
1. In cases of palmoplantar pustulosis, pustules overlying erythema are located in the palmoplantar area with or without coexistence of psoriatic plaques in other locations. Pathological examination shows neutrophil aggregation within the epidermis, resulting in the formation of pustules.
2. Acrodermatitis continua refers to erythema and pustules that occur at the distal portion of the fingers or toes,and the lesions are usually induced by trauma.This condition gradually evolves from one finger or toe to multiple fingers or toes.Onychoptosis and shedding of the nail plates occur,and the pathology is similar to that of palmoplantar pustulosis.
Generalized pustular psoriasis
1. Light yellow or white-yellow small, superficial sterile pustules ranging in size from pinpoint to millet grains rapidly develop with a dense distribution.
2. Flaky lakes of pus are systemically distributed with swelling and pain.
3. The condition may evolve into erythrodermic psoriasis,sometimes accompanied by joint and fingernail or toenail damage.
4. Shivering and high fever are present in the remittent fever-type of the disease.
Erythrodermic psoriasis
1. Patients usually have a history of other types of psoriasis.
2. Patients have aggravated disease conditions, or the disease is abruptly aggravated by improper medication or other stimuli, leading to the development of diffuse erythema,swelling,and desquamation.The lesion area involves more than 90%of the body surface area(BSA).
3. Lesions of psoriasis vulgaris are occasionally observed.
4. This condition can be accompanied by systemic symptoms such as fever and hypoproteinemia.
Arthropathic psoriasis
1. Patients usually have a history of other forms of psoriasis.
2. Patients have swelling and pain in their finger or toe joints, the large joints of the arms and legs, the spine,and the sacroiliac joint, consistent with the “morning stiffness” phenomenon.
3. Radiographs, magnetic resonance imaging, and Bultrasound examination show enthesitis, joint cavity effusion, and synovial thickening. Severe cases are characterized by joint deformation, arthrostenosis, or bone mass destruction.
4. The C-reactive protein level is increased,the erythrocyte sedimentation rate is high, and rheumatoid factor is usually negative. Patients with spine or sacroiliac joint involvement usually test positive for HLA-B27.
TCM symptom differentiation
The basic TCM symptom types include blood heat symptoms (observed during the active stage, primarily with inflammation), blood stasis symptoms (observed during the stable stage, primarily with epidermal hyperplasia), blood dryness symptoms (observed during the regressive stage, primarily with skin barrier dysfunction),blazing heat-toxin symptoms(observed in the erythrodermic type or generalized pustular type), accumulated dampness-heat symptoms (observed in the localized pustular type),and wind-dampness obstruction symptoms(observed in the arthropathic type).All symptom types can transform or evolve into other types and be combined with one another.
Severity classification of psoriasis vulgaris
Assessment of disease severity is the cornerstone in psoriasis management, and many tools are available for this assessment in clinical practice. Some of these tools,such as BSA measurement, the Dermatology Life Quality Index (DLQI), and the Psoriasis Area and Severity Index(PASI), have been validated and show good internal consistency,and they are acceptable to most dermatological clinical practitioners.5-6
BSA: It refers to the body surface area occupied by psoriasis lesions. When measuring the percentage of BSA involved by psoriasis, one of the patient’s full flat hands including the fingers is considered to represent 1%of BSA.
DLQI: This self-administered questionnaire is used to assess the impact of the disease on quality of life.The score ranges from 0 to 30.
PASI:This index assesses the severity based on the extent of the body surface involved and characteristics such as erythema,induration,and scaling.The score ranges from 0 to 72.
The severity of plaque psoriasis is classified as follows.
Mild: Involvement of <3% of the BSA is considered mild. Patients’ quality of life is rarely affected, and treatment is not required.The DLQI score ranges from 2 to 5 points, and the PASI score is ≤3.
Moderate:The skin rash involves 3%-10%of the BSA and affects patients’ quality of life. Patients can expect treatment to improve their quality of life.The DLQI score ranges from 6 to 10 points,and the PASI score ranges from 3 to 10.
Severe: The skin rash involves >10% of the BSA and greatly affects patients’ quality of life. Patients also often develop adverse reactions that influence their quality of life.The DLQI score is >10 points,and the PASI score is ≥10.
Psoriasis comorbidities
Psoriasis is not only limited to the skin;it is also a systemic disease.Psoriasis is associated with multiple comorbidities ranging from cardiovascular and metabolic diseases to malignancies and psychological conditions. Patients with moderate to severe psoriasis have a higher prevalence of cardiovascular disease, metabolic syndrome, and Crohn disease;the individual components of these disorders,such as hypertension,diabetes,hyperlipidemia,and abdominal obesity,vary according to disease severity.7-11A multitude of psychological comorbidities are also associated with psoriasis, including anxiety, depression, low affective expression,low problem-solving skills,sleep disturbances,sexual dysfunction, and suicidal ideation.12-14
Purpose and principles of psoriasis treatment
Purpose
Treatments are pursued to control and stabilize the disease activity; delay its progression to the whole body; relieve erythema, scales, and plaque thickening; avoid triggering factors that cause relapse or aggravation; reduce adverse reactions caused by treatment; and improve the patient’s quality of life.
Many treatment methods are available for psoriasis,including topical therapy, physical therapy, and systemic therapy.Clinical physicians should weigh the pros and cons to reasonably choose a treatment regimen based on the individual condition, disease subtype, severity, and treatment requirements. If patients with moderate to severe psoriasis experience a poor effect of one treatment method,then combined,rotational,or sequential treatments should be performed.15
Principles
1. The treatment should be standardized, and use of therapeutic drugs/methods recommended by the guidelines should be emphasized.
2. The treatment should be safe, and adverse reactions should be avoided as much as possible.
3. The treatment should be personalized. The patient’s disease condition, willingness, tolerance, economic situation,treatment history,and adverse drug reactions should be comprehensively considered to develop a reasonable treatment regimen.
Nonsystemic treatment of psoriasis
Topical drug treatment
Topical drugs are usually used to treat patients with mild psoriasis. The advantages of topical formulations include the direct application of drugs onto skin rashes, rapid onset,convenient use,and few systemic adverse reactions.The disadvantages are that long-term use can cause local adverse reactions, they are inconvenient for patients with extensive rashes, and patient compliance varies widely.
Different types and formulations of topical drugs should be chosen based on the lesions and the patient’s requirements. Commonly used topical drugs include emollients,moisturizers, vitamin D3 derivatives, retinoids, glucocorticoids, calcineurin inhibitors, anti-interleukin 8 (IL-8)monoclonal antibodies, and coal tar preparations. Compound preparations can increase the efficacy and reduce the adverse reactions of these drugs and are convenient to use; they include compound calcipotriol (calcipotriol +betamethasone),compound clobetasol propionate(tretinoin + clobetasol propionate), and compound tazarotene(tazarotene + betamethasone).
Phototherapy
Ultraviolet(UV)phototherapy includes UVA(wavelength of 320-400nm), UVB (wavelength of 290-320nm), and UVC (wavelength of 180-290nm). Narrowband UVB(NB-UVB)has the most extensive clinical applications and is suitable for treatment of moderate to severe psoriasis vulgaris (including both guttate and plaque types) and arthropathic psoriasis. Caution is needed when using phototherapy to treat patients with erythrodermic or pustular psoriasis.
When starting NB-UVB phototherapy, the patient’s minimal erythema dose should be measured. The initial irradiation dose is 0.5-0.7 minimal erythema dose three times a week. Based on the patient’s response after irradiation, the irradiation dose is gradually increased by 10%-20% at each treatment session, or a fixed dose increment (0.05 or 0.1J/cm2) can be used. If no obvious erythema is present after treatment, then the treatment dose can be gradually increased. If mild erythema is present, then irradiation is performed using the previous dose. If moderate to severe erythema is present, then the treatment can be stopped until the erythema disappears,and the irradiation dose should be reduced by 10%-20%of the previous dose. If painful erythema or blisters are present,the treatment should be stopped,and medication can be applied to relive the symptoms. When the skin rashes disappear by more than 80%, the dosage can be reduced to twice a week for one month,then once a week for one month, and then once every two weeks for more than two months. The dose should be reduced by 15%-25% based on the patient’s response to and tolerance of the irradiation.The total treatment time should be at least four months. Psoralen plus UVA (PUVA)therapy, a 308-nm excimer laser,and 308-nm filtered UV light can be used for stubborn localized rashes.16-20
TCM external treatment
TCM treatments are divided into external treatment methods and nondrug therapies. External treatments include topical applications, herb packages, medicated baths, fumigation, soaking (staining), and acupuncture therapy.Nondrug therapies include cupping,acupuncture,catgut implantation at an acupoint, fire needle, threeedged needle,and auricular acupuncture.These techniques should be performed after symptom differentiation.Indications, contraindications, and operational specifications should be mastered.
Systemic drugs for psoriasis
Methotrexate (MTX)
MTX is efficacious for all cases of moderate to severe plaque-type, arthropathic, erythrodermic, and generalized pustularpsoriasisaswellasnailandpalmoplantar psoriasis.It is particularly suitable when phototherapy,photochemical therapy,andother systemic therapies are ineffective.The indications for use of MTX in patients with psoriasis are strict. Before MTX administration, patients should be carefully evaluated to determine eligibility(Table 1).
The most commonly recommended dose of MTX is 5-25mg/week. The initial dose is usually 2.5-7.5mg/week,and it can be orally administered once every 12h, three times a week.The dose is increased by 2.5mg every two to four weeks until it gradually reaches 15-25mg/week.21After the disease is controlled,drug administration should be maintained for at least one to two months before the dose reduction the dose is reduced by 2.5mg every four weeks until the minimal maintenance dose is reached.The efficacy of MTX reaches peak after 12-16 weeks of treatment.If no obvious efficacy is obtained,the treatment should be stopped. Routine blood tests and liver and kidney function tests should be regularly performed during the MTX treatment period. If the continuous cumulativedose is higher than 1,500mg,the level of procollagen III Nterminal propeptide should be regularly measured to prevent/monitor liver fibrosis. Different opinions exist regarding whether patients who receive MTX should be supplemented with folic acid.22-23People who recommend supplementation believe that it can reduce adverse reactions without reducing efficacy.24Two recommended regimens for folic acid supplementation exist:one is 1mg/day for five consecutive days, and the other is 5mg every 12h, three times a week starting from 12h post the last MTX administration.25-26

Table 1Contraindications of methotrexate
Cyclosporine A (CsA)
CsA is effective for all types of psoriasis.It is recommended for all patients with severe or moderate to severe psoriasis for whom other therapeutic methods have failed. For children and adolescents, CsA can only be used with caution to treat severe cases for which other medications are ineffective (Table 2).
The most commonly recommended dose of CsA is 3-5mg/(kg·day), which can be divided into twice daily dosing.27The recommendedinitial dose of CsA forpsoriasis treatment is 2.5mg/(kg·day)for four weeks;the dose is then increased by 0.5mg/(kg·day) every two weeks until the maximum dose of 5mg/(kg·day)is reached.28If the patient takes the maximum dose that can be tolerated for more than six weeksandno satisfactoryefficacy is observed,thedrug is discontinued.29After the symptoms are controlled,the dose is gradually reduced by 0.5-1mg/(kg·day)every two weeks until the minimum effective dose for treatment maintenance is reached. The recurrence rate is lower and the remission period is longer when the CsA dose is gradually reduced instead of abruptly terminated.30-31The disease often recurs after CsA withdrawal.It usually returns to the pretreatment level from two weeks to two months after discontinuing CsA;therefore,long-term treatment should be maintained with a small dose.
For intermittent short-term therapy, oral CsA is administered for 12-16 weeks until the symptoms ofpsoriasis are significantly improved,and the medication is then terminated.27,30,32For sustained long-term therapy,the initial CsA dose is 4mg/(kg·day). When the clinical symptoms have significantly improved or the disease is cured, the therapy is continued using the lowest dose required to maintain efficacy.33The maintenance dose is usually 3-3.5mg/(kg·day).34Rescue therapy refers to short-term CsA therapy for certain patients with severe psoriasis; this treatment regimen enables CsA to rapidly exert its therapeutic function. Next, alternative drugs or therapies are used.35Such treatments are primarily used for patients with erythrodermic psoriasis, suberythrodermic psoriasis,or generalized pustular psoriasis.To reduce the duration of CsA use and possible adverse reactions,other systemic drug therapies (e.g., acitretin, fumarate,MTX,and mycophenolate mofetil)can be alternately used in a treatment called rotational therapy.32,35This therapy is recommended for children and adolescents when the disease is severe or other drug therapies are ineffective,although it must be used with caution.Nephrotoxicity and hypertension are highly concerning adverse reactions.The short-term treatment time is two to four months,and longterm treatment should not exceed two years.27,35-36The treatment protocol shown in Table 3 should be used in cases of inappropriate use of CsA or the appearance of obvious toxic adverse effects.
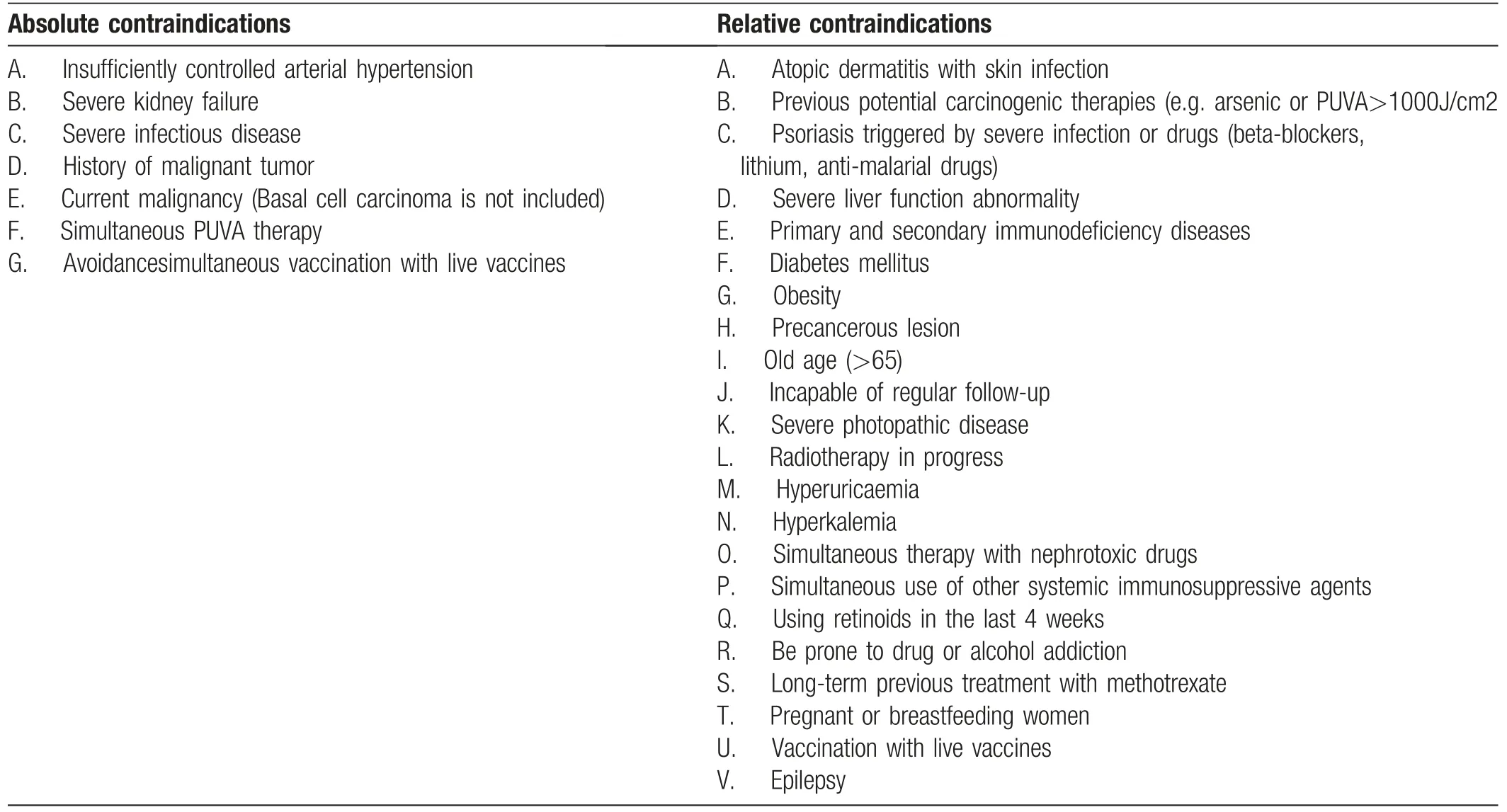
Table 2Contraindications of ciclosporin
Retinoids
Retinoids are primarily used for patients with plaque-type,pustular, or erythrodermic psoriasis. Their efficacy is poor for patients with arthropathic psoriasis. The most commonly recommended dose of oral acitretin is 0.5-1.0mg/kg/day. This drug should be taken with food to enhance its absorption.The most common dose is 30-50 mg/day.37-38The recommended initial dose of acitretin to treat plaque psoriasis ranges from 10 to 20mg/day for two to four continuous weeks.The dose is gradually increased until the optimal efficacy is reached. The maximum dose should not exceed 1.0mg/(kg·day).39There are greater individual differences in maintenance doses based on patients’conditions.During combined therapy,the recommended dose is <30mg/day.Women of childbearing age,people of advanced age, children, and adolescents should use retinoids with caution,and pregnant women should not use this drug.Because of the high risk of adverse reactions,patients should be carefully monitored during the course of treatment. Any obvious toxic adverse effects should be immediately managed by physicians(Table 4).
Biological agents
Biological agents in the form of monoclonal antibodies to inflammatory cytokines have recently been used to treat moderate to severe psoriasis and have shown excellent efficacy and safety.40Biological agents currently used in clinical work include tumor necrosis factor α (TNF-α)antagonists(etanercept,infliximab,and adalimumab),the IL-12/IL-23 antagonist ustekinumab, and IL-17A antagonists (secukinumab and ixekizumab).
Biological agents can be used for moderate to severe psoriasis.Importantly,clinicians should assess the patient’scondition, communicate adequately with the patient, and obtain informed consent prior to treatment.In addition to meeting condition in the following part(a),the patient also needs to meet one of the items listed in part(b):
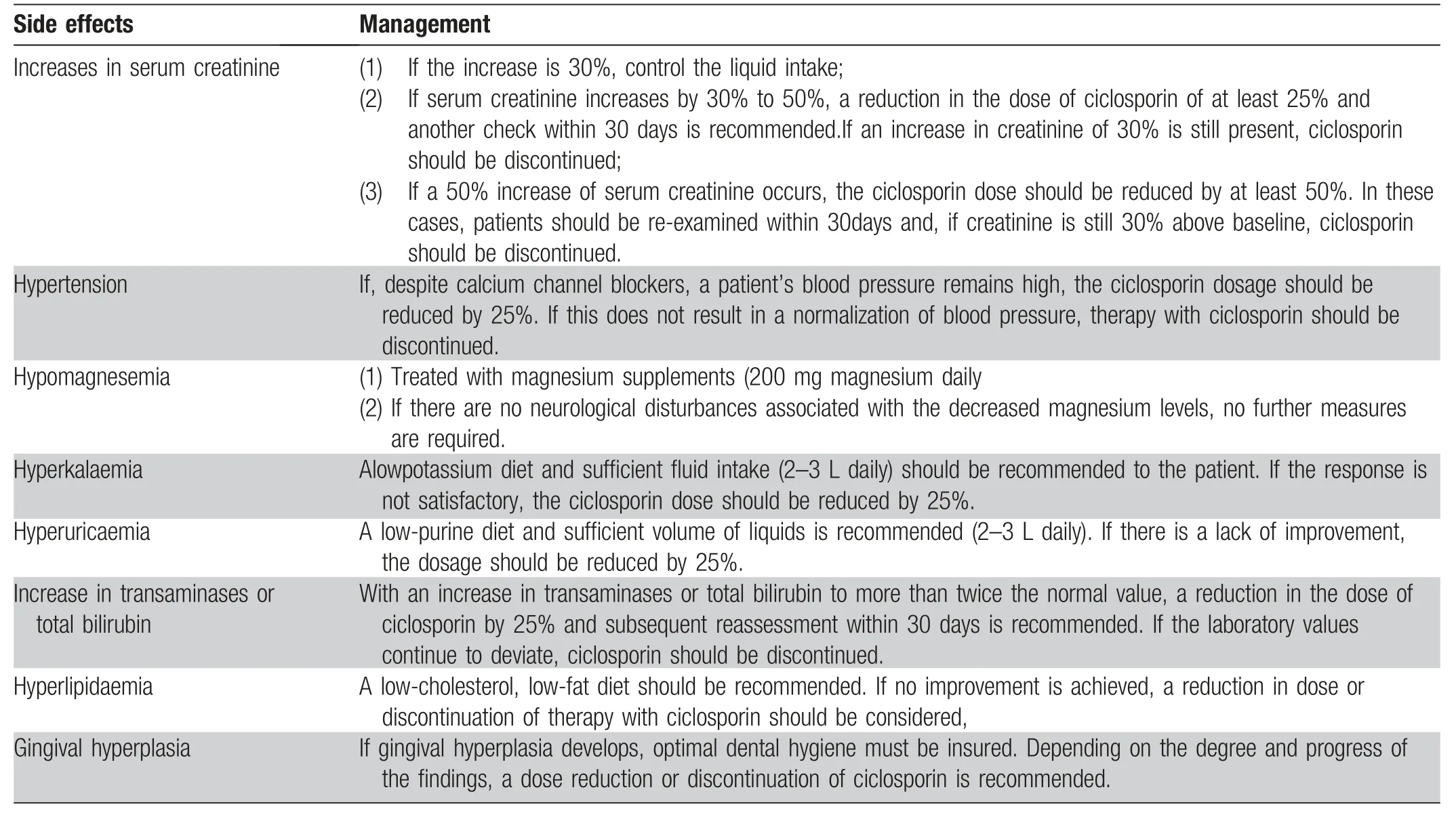
Table 3Major side effects of ciclosporin and management
(a) Moderate to severe psoriasis,PASI score of ≥10 points or area of involvement ≥10% of the BSA, and DLQI score of ≥10 (when unable to evaluate the PASI). In special cases,other areas that seriously affect physical and mental health (e.g., genital region and exposed parts of limbs)may also be candidates for treatment if they do not meet the previously stated criteria.
(b) Meet at least one of the following criteria: (1) The patient has a higher risk of serious adverse effects after the introduction of other traditional systemic treatments; (2) The patient cannot tolerate the current systematic treatments; (3) Standard systematic treatment is not effective;(4)The presence of comorbidities prevents the use of traditional systematic treatment;(5)The patient’s clinical situation is life-threatening.
Discontinuation of biological therapy is recommended when (1) serious drug-related adverse reactions occur,such as serious infections (including active tuberculosis),heart failure, tumors, demyelinating syndrome, or lupuslike syndrome;(2) treatment failure occurs;or(3)clinical remission has been achieved.
TNF-α antagonists (etanercept, infliximab, and adalimumab)
Etanercept is a recombinant human-source soluble TNF-α receptor fusion protein.It can competitively bind to TNFα in the blood,blocking TNF-α from binding to the TNF-αreceptor on the cell surface and thus reducing the activity of TNF-α. The recommended therapeutic regimen for etanercept is as follows: Patients receive subcutaneous injections of 25mg twice a week or 50mg once a week.The dose for children (4-17 years) is 0.8mg/kg every week.41Etanercept is generally effective after one to two months of administration. After treatment withdrawal, the disease sometimes shows continuous improvement.

Table 4Majorside effects of acitretin and management
Infliximab is a TNF-α monoclonal chimeric antibody formed by the antigen-binding fragment of murine immunoglobulin G(IgG)and the fragment crystallizable segment of human IgG.Infliximab binds to soluble and transmembrane TNF-α,interfering with the ability of TNF-α to bind to TNFα receptors on the cell surfaceand thuscausingTNF-α to lose its biological activity.The recommended therapeutic regimen for infliximab in patients with severe psoriasis is as follows:Patients receive intravenous injections of 5mg/kg at weeks 0,2, and 6. The drug is then administered once every eight weeks.The drug is generally effective after two weeks of drug administration.The highest efficacy is usually achieved after 10 weeks of treatment.42-43
Adalimumab is a fully human IgG1 monoclonal antibody to TNF-α. It can specifically bind to soluble and transmembrane TNF-α molecules to block their biological activity. The recommended treatment method for adalimumab is as follows. The initial dose is a subcutaneous injection of 80mg. This dose is reduced to 40mg during week 2, and drug administration is then continued at 40mg every two weeks. Clinical efficacy is evident after two weeks of treatment.The highest efficacy is generally achieved between 12 and 16 weeks.44-45
IL-12/IL-23 antagonist
Ustekinumab is a fully human monoclonal IgG1 antibody that blocks IL-12 and IL-23 and thus blocks Tlymphocyte differentiation to Th1 and Th17. The recommended treatment regimen with ustekinumab is as follows.Patients receive subcutaneous injections of 45 mg(body weight of ≤100kg)or 90mg(body weight of >100kg) during weeks 0 and 4. The drug is then administered once every 12 weeks.If the efficacy is poor,the drug dosage can be increased or administered once every eight weeks.46-47
IL-17A antagonist
Secukinumab is a fully human monoclonal antibody to IL-17A IgG1 that inhibits IL-17A activation and the inflammatory response. The recommended treatment regimen is subcutaneous injection of 300mg during weeks 0, 1, 2, 3, and 4, after which the drug is administered at 300mg once a month for maintenance.48
Ixekizumab is a humanized IgG4 monoclonal antibody that targets neutralizing IL-17A, inhibiting IL-17A activation, and the inflammatory response in a highly selective manner.Ixekizumab was approved by the China Food and Drug Administration in 2019 to treat adult patients with moderate to severe plaque psoriasis. The recommended dose is 160mg by subcutaneous injection at week 0,followed by 80mg at weeks 2, 4, 6, 8, 10, and 12; a maintenance dose of 80mg is given every four weeks thereafter. Some randomized double-blind controlled global phase III clinical trials have demonstrated excellent effectiveness of ixekizumab for severe plaque psoriasis.49-50
TCM internal treatment methods
Patients with moderate to severe psoriasis primarily use TCM internal treatment methods. TCM combined with Western medicine is recommended to treat severe/pustular/erythrodermic/arthropathic psoriasis. Heat-clearing and bloodcooling are primarily used during the active stage of guttate/plaquepsoriasis,andnourishingbloodformoistening dryness and activating blood circulation to dissipate blood stasis are primarily used during the stable and regressive stages. Patients with erythrodermic or generalized pustular psoriasis are treated with purging fire to remove toxins.Patients with localized pustular psoriasis are treated with clearing heat and promoting diuresis for detoxification.Patientswitharthropathicpsoriasisaretreatedwithdispelling wind,eliminating dampness,and dredging channels.
The TCM drugs usually applied for psoriasis treatment includecompoundQingDai capsule(pill),Yujinyinxietablet,Yinxieling, Yinxie infusing powder, Keyin pills, Xiaoyin granules, and Xiaoyin tablet; however, further studies of evidence-based medicine are still required to investigate the efficacy of these compound medications. Single-drug prescription/monomer Chinese patent drugs or plant extract drugs such as triptolide preparation, Tripterygium hypoglaucum Hutch, total glucosides of paeony, compound glycyrrhizin,glycyrrhizin,and glycyrrhizic acid are effective for assisting with psoriasis treatment. Compound glycyrrhizin can be used to prevent or attenuate the liver damage caused by treatment with certain systemic drugs.
Treatment regimens for psoriasis
The aim in selection of a treatment regimen is to effectively control the disease, reduce drug adverse reactions, and increase patient compliance. Under this principle, the sequential, combined, or rotational treatment methods based on various therapeutic drugs/therapies(e.g.,topical drugs,systemic drugs,or phototherapy)are developed for targeted individual therapy.
Treatment of different types of psoriasis
Guttate psoriasis
Guttate psoriasis is primarily treated using topical drugs or phototherapy.Vitamin D3derivatives(e.g.,tacalcitol)are suitable for acute guttate psoriasis.They can be combined with weak- or moderate-potency glucocorticoids or used alone.They can also be combined with UVB.Glucocorticoids of weak to moderate potency (e.g., hydrocortisone/mometasone furoate/fluticasone propionate ointment)can be combined with tacalcitol or UVB. The preferred phototherapy is NB-UVB. The efficacy of this treatment is much higher when it is combined with moisturizers,glucocorticoids, or vitamin D3derivatives.
Some patients with guttate psoriasis have streptococcal infection. Tonsillectomy might improve the condition of the disease, prolong the remission period, and increase treatment efficacy.
Systemic therapy includes antibiotics and TCM. Retinoids and immunosuppressive agents are effective but should be used with caution.
Plaque psoriasis
Patients with mild plaque psoriasis primarily use local therapy, and most cases can be effectively controlled.Topical preparations include vitamin D3derivatives,retinoids, moderate/high-potency glucocorticoids, and calcineurin inhibitors. Local phototherapy can also be applied. When monotherapy leads to an obvious adverse reaction or poor efficacy,the rotational or combined use of two or more medications can be chosen.Commonly used combination regimens include a vitamin D3derivative +calcineurin inhibitor, a glucocorticoid + vitamin D3derivative, and a glucocorticoid + retinoid.
Patients with moderate to severe plaque psoriasis require systemic therapy or phototherapy. Drugs include retinoids, immunosuppressive agents (e.g., MTX, CsA, or triptolide preparation), and biological preparations.Systemic therapy can be combined with topical medication to increase efficacy.Patients with extensive skin rashes can use phototherapy (e.g., NB-UVB or PUVA).
Erythrodermic psoriasis
Patients with erythrodermic psoriasis require systemic therapy. Drugs include retinoids, MTX, CsA, and biological agents. Acitretin and MTX have shown good long-term efficacy in the treatment of erythrodermic psoriasis. However, their onset of action is slow. A gradual reduction in the dose might effectively prevent recurrence.CsA or biological agents are recommended for patients with severe or unstable disease.
Local or systemic glucocorticosteroids are generally not recommended unless patients have severe,life-threatening symptoms of toxicity. When the disease is severe or the patient’s condition is urgent, systemic steroids treatment should be used to control acute inflammation; when the disease is controlled, the dose can be gradually decreased until drug withdrawal. If the patient also has a fever,hypoproteinemia,fluid and electrolyte imbalance,secondary infection, or liver dysfunction, then the systemic condition should be monitored while providing nutritional support, correction of water and electrolyte imbalance,prevention and treatment of infection, and protection of liver function. In addition, attention should be paid to protecting the function of vital organs and systems such as the heart, kidneys, and central nervous system.
Pustular psoriasis
Retinoids,MTX,CsA,and biological agents can be chosen for patients with generalized pustular psoriasis.Acitretin is the standard therapeutic drug; after the acute disease process has been controlled,the dose is gradually reduced for maintenance.In severe cases,biological agents or CsA can be applied for initial treatment. After the disease is controlled,retinoids or MTX can be used for maintenance.
Glucocorticoids can rapidly control pustule dissemination and relieve systemic symptoms;however,they should be used carefully.Glucocorticoids are recommended only when the disease is severe or life-threatening,the efficacy of other measures is poor, or other treatments are contraindicated. These treatments should be combined with acitretin or immunosuppressive agents; after satisfactory efficacy is obtained,the dose should be gradually reduced until drug withdrawal.
Topical medication is primarily applied for protection.When pustules are not broken,calamine lotion can be used to relieve swelling;after the pustules are broken,the skin is primarily treated with cleaning.
In addition to local therapy,systemic therapy can also be used to treat patients with localized pustular psoriasis.
Arthropathic psoriasis
The purpose of treatment for arthropathic psoriasis is to control inflammation and prevent joint injury and disability. The types and severity of joint injury should be fully assessed. Patients should have proper rest and avoid overwork to prevent joint strain. In addition,patients should be encouraged to engage in moderate joint function exercise. Systemic therapeutic drugs include nonsteroidal anti-inflammatory drugs,MTX,and biological agents.Triptolide preparations and total glucosides of paeony can relieve joint symptoms.
Treatment of psoriasis in specific locations
Scalp psoriasis
Approximately 45%-80% of patients have scalp psoriasis. The scalp is primarily the area of first onset, and psoriasis can develop in the scalp alone.The rash coverage is thicker than scales,usually extends over the hairline,and“hair clumps”can be observed.Coal tar and salicylic acid shampoo can be helpful. Topical glucocorticoids are effective for all mild, moderate, and severe cases.Moderate- to high-potency glucocorticoids should be used. Drug administration should be started twice a day and then gradually reduced to once a day.The efficacy of retinoids and calcipotriol is inferior to that of potent glucocorticoids;however,the tolerance of their long-term use is high,and the risk is low;thus,they can be combined with glucocorticoids.
Moderate to severe cases can also be treated with systemic therapy,and acitretin,MTX,or biological agents can be administered.
Nail psoriasis
The nails can be affected in all types of psoriasis,and 90%of patients with arthropathic psoriasis have nail changes(e.g.,pitting,oil drop sign,onycholysis,onychoptosis,and subungual hyperkeratosis). Potent/superpotent glucocorticoids are usually administered for treatment and have better effects on nail matrix involvement. Topical treatment is performed once to twice a day. Calcipotriol has a better effect on nail matrix involvement.Tazarotene shows better efficacy for onycholysis and pitting, and occlusion is required to enhance efficacy. The most common adverse reactions are erythema, local irritation,desquamation,and paronychia.An intralesional injection of a low dose of triamcinolone acetonide is effective for nail matrix involvement.Among systemic drugs,CsA has the highest efficacy in treating nail psoriasis.
Inverse psoriasis
Skin rashes involve intertriginous areas such as the armpits,under the breasts, groin, genitals, and perineum. These rashes are primarily treated with local therapy. When necessary, physical therapy can be applied. Systemic therapy is not generally used.Weak-to moderate-potency glucocorticoids are the preferred treatment.Weak-potency glucocorticoids are chosen for maintenance and are gradually replaced by vitamin D derivatives or calcineurin inhibitors. Potent/superpotent glucocorticoids are not recommended.Mild glucocorticoids(e.g.,hydrocortisone)and moderate or soft glucocorticoids (e.g., mometasone furoate and hydrocortisone butyrate)should be chosen for skin rashes on the genitals. Calcineurin inhibitors are effective for mucosal lesions.
Systemic therapy is only used for severe symptoms,combinations of inverse psoriasis with other types of psoriasis,or severe diseases that affect patients’quality of life. MTX, CsA, and retinoids can be chosen.
Treatment of psoriasis in specific populations
Psoriasis in children
Mild psoriasis in children usually requires only local therapy. Emollients should be used conventionally.Glucocorticoids are the most widely used topical drugs for psoriasis treatment. Vitamin D derivatives are also usually applied in cases of mild to moderate psoriasis in children. Calcineurin inhibitors are primarily used on the face, genitals, and skin folds and can be used alone or combined with glucocorticoids.
Phototherapy can be chosen for children with generalized plaque/guttate psoriasis or palmoplantar pustulosis. The effect of NB-UVB on guttate and small-plaque psoriasis is better than that on large-plaque psoriasis.Attention should be paid to the potential risk of cancer in children undergoing long-term phototherapy. Commonly used systemic drugs include retinoids,MTX,CsA,and biological preparations.The preferred choice for arthropathic psoriasis in children is MTX or biological agents.Guardians must be aware of the possible adverse reactions and the need for long-term monitoring of the selected regimen.
Psoriasis in pregnant or lactating women
Emollients and moisturizers are the safest basic medications in women who are pregnant or lactating. Topical glucocorticoids can be chosen based on the patient’s condition. Using weak- to moderate-potency glucocorticoids in small areas before and during pregnancy is relatively safe; however, they should not be applied to a large surface area. Topical vitamin D3derivatives should not be used during pregnancy. Systemic application of glucocorticosteroids should be avoided during early pregnancy.
Psoriasis in people of advanced age
Topical glucocorticoids should be chosen carefully in patients of advanced age. The use of irritating topical drugs should be avoided on intertriginous areas. Compound preparations reduce adverse effects, increase efficacy,are convenient to use,and have high compliance.Topical drugs have poor efficacy.Patients who cannot use systemic drugs because of complications and related risk factors should receive phototherapy.
Retinoids can be used in advanced-age patients who do not have severe liver or kidney insufficiencies. Attention should be paid to the risk of elevated triglycerides. CsA should be used carefully in older patients because of their reduced ability to excrete CsA through the kidneys.
Patient-centered psychotherapy, disease management, and prevention
Psychotherapy
Psychotherapy refers to the use of psychological methods to train, educate, and treat patients through communication and education factors to reduce or eliminate their physical symptoms,improve their mental status,and help them adapt to their family,social,and work environments.Psoriasis is a psychosomatic disease.Psychological factors play an important role in the induction, progression, and treatment of psoriasis. The effect of psoriasis on healthrelated quality of life is as great as that of cancer, heart failure, diabetes mellitus, or depression.51Most patients with psoriasis present with anxiety, nervousness, depression,or feelings of inferiority.The recurrent and prolonged features of psoriasis cause some patients to lose their confidence in treatment and develop poor adherence,which results in anxiety and irritability and thus further aggravates the disease.Psoriasis is a discosmetic dermatosis. It easily results in inferiority complexes in affected patients, severely influencing their social lives and significantly increasing the rates of suicide and death.
Psychotherapy is an indispensable part of psoriasis treatment. It is primarily divided into the following four parts.
1. Health education interventions seek to strengthen patients’ understanding of this disease and guide them in the standardized, rational use of drugs.
2. Nursing service interventions seek to optimize the relationship between doctors and patients, thereby integrating humanistic care and operation specifications to assist patients to use drugs correctly.
3. Specific psychological interventions seek to provide targeted psychological guidance and behavior interventions based on patients’ specific conditions. These interventions include relaxation training (e.g., mind relaxing, abdominal breathing, and music and muscle relaxation methods), collective psychological interventions, and biofeedback therapy (e.g., using a bioresonance therapy device).
4. Systemic psychological interventions seek to influence and improve patients’emotions,let go of their concerns and worries, boost their will and confidence to overcome the disease, and achieve early rehabilitation by the language,expression,posture,behavior,and care of the medical staff.
Providing targeted medical education for patients
When receiving targeted medical education, patients should first be made aware that psoriasis is a chronic disease.Although it severely influences their quality of life,it is not contagious. If the disease is treated early and appropriately, patients’ quality of life can be increased,and this condition is usually not life-threatening. Next,patients should believe in science and fully understand that psoriasis is a disease that is induced or aggravated by unhealthy living habits, psychological stress, infection, or environmental factors; furthermore, they should not seek out folk prescriptions or radical cures.In addition,patients should undergo targeted health interventions, a healthy lifestyle should be advocated, and patients should be encouraged to seek treatment from psoriasis clinics at local hospitals and enroll in follow-up cohorts to receive personalized treatments and healthcare education.
Popularizing medical knowledge throughout society
Science popularization should be strengthened throughout the society to enable the public to understand that psoriasis is a noncontagious chronic disease. Patients should receive understanding and respect to help eliminate their psychological concerns.Althoughgeneticfactorsarepresentinpsoriasis,current studies do not indicate that heredity is destiny.
Prevention
Multiple individual and environmental factors influence the development and recurrence of psoriasis.For example,respiratory tract infections,excessive mental stress/depression,unhealthy living habits(e.g.,smoking and drinking),and obesity induce or aggravate this disease. Patients should continuously summarize and explore their patterns of disease onset, develop healthy living habits, and cooperate with active and effective treatments to prevent the development and recurrence of psoriasis.
Authors list
Xue-Jun Zhang, The First Afiliated Hospital, Anhui Medical University; Jie Zheng, Rui Jin Hospital, School of Medicine,Shanghai Jiao Tong University;Zhi-Bo Yang,The Second Affiliated Hospital of Hunan University of Chinese Medicine;Min Zheng,Second Affiliated Hospital,Zhejiang University School of Medicine; Jun Gu, Changhai Hospital, The Second Military Medical University;Xi-Bao Zhang, Institute of Dermatology, Guangzhou Medical University,Guangzhou Institute of Dermatology;Zhi-Zhong Zheng, Huashan Hospital, Fudan University;Xu Fang,Huashan Hospital,Fudan University;Qing Sun,Qilu Hospital,Shandong University;Xiao-Ming Liu,The University of Hong Kong-Shenzhen Hospital;Xiang Chen,Xiangya Hospital, Central South University; Yong Cui,China-Japan Friendship Hospital; Wei-Xin Fan, First Affiliated Hospital of Nanjing Medical University; Heng Gu,Hospital for Skin Diseases(Institute of Dermatology),Chinese Academy of Medical Sciences; Hong-Zhong Jin,Peking Union Medical College Hospital; Bin Li, Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine; Yu-Zhen Li, The Second Affiliated Hospital of Harbin Medical University; Hong-Xia Liu, Hospital of Traditional Chinese Medicine,Xinjiang Medicine University; Qiao Liu, The Second Affiliated Hospital of Jiangxi University of Traditional Chinese Medicine; Chuan-Jian Lu,Guangdong Provincial Hospital of Chinese Medicine,Guangdong Provincial Academy of Chinese Medical Sciences, and The Second Clinical School of Guangzhou University of Chinese Medicine; Cheng-Zhi Lv, Dalian Dermatosis Hospital;Hui-Qun Ma,The Second Hospital of Xi’an Jiaotong University;Yu-Ling Shi,Shanghai Tenth People’s Hospital, Tongji University School of Medicine;Gang Wang, Xijing Hospital, Fourth Military Medical University; Jin-Hua Xu, Huashan Hospital, Fudan University; An-Ping Zhang, First Affiliated Hospital,Anhui Medical University; Chun-Lei Zhang, Peking University Third Hospital; Fu-Ren Zhang, Shandong Provincial Hospital for Skin Diseases, Shandong First Medical University & Shandong Provincial Institute of Dermatology and Venereology, Shandong Academy of Medical Sciences; Jian-Zhong Zhang, Peking University People’s Hospital; Dong-Mei Zhou, Beijing Hospital of Traditional Chinese Medicine,Capital Medical University;San-Quan Zhang, Institute of Dermatology, Guangzhou Medical University,Guangzhou Institute of Dermatology;Yao-Hua Zhang, Worldwide Medical Center, Huashan Hospital, Fudan University; Xin Li, Yueyang Hospital of Integrated Traditional Chinese and Western Medicine,Shanghai University of Traditional Chinese Medicine;Qing Yang, Shandong Provincial Hospital for Skin Diseases,Shandong First Medical University&Shandong Provincial Institute of Dermatology and Venereology,Shandong Academy of Medical Sciences.
杂志排行
国际皮肤性病学杂志的其它文章
- Chinese Guidelines for the Management of Chronic Pruritus (2018)#
- Chinese Guidelines for the Diagnosis and Treatment of Urticaria: 2018 Update#
- Effects of Honokiol on Activation of Transient Receptor Potential Channel V1 and Secretion of Thymic Stromal Lymphopoietin in HaCaT Keratinocytes
- Pathogenesis of Photoaging in Human Dermal Fibroblasts
- Lipoid Proteinosis Due to Homozygous Deletion Mutation (c.735delTG) in the ECM1 Gene Presents with Seizures and Hoarseness but No Skin Involvement
- Mycobacterium Chelonae/Abscessus Co-infection of the Limbs: A Challenging Case
