Mycobacterium Chelonae/Abscessus Co-infection of the Limbs: A Challenging Case
2020-04-03LiDanZhangXinZhouLingLinXinTianQuanLuo
Li-Dan Zhang, Xin Zhou, Ling Lin, Xin Tian, Quan Luo,∗
1Department of Dermatology, The Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, Guangdong 510150,China; 2Department of Dermatology, Guangzhou Institute of Dermatology, Guangzhou, Guangdong 510095, China.
Introduction
Mycobacterium abscessus(M.abscessus)and Mycobacterium chelonae (M. chelonae) are two species of rapidly growing mycobacteria that are frequently associated with nosocomial outbreaks and pseudo-outbreaks.1They are a type of non-tuberculous mycobacteria classified as rapidly growing mycobacteria (RGM, group IV in the Runyon classification).2M. chelonae and M. abscessus are commonly associated with skin and soft tissue infections.3Infected patients often exhibit non-specific clinical symptoms that may lead to a delayed diagnosis. Few reports have described M. chelonae/abscessus complex infection,especially in patients without immunologic suppression.The present case we reported provides information that may assist clinician to understand the rare co-infection of M. chelonae/abscessus.
Case report
In February 2017, a 26-year-old woman was admitted to the Dermatology Department, Guangzhou Institute of Dermatology, with a 5-month history of various skin lesions on both lower limbs. She had developed two abscesses 5 months ago; however, no tissue culture was performed at that time, so we were unable to know the nature of infection. After surgical drainage of the abscesses, the original lesions developed into various abnormalities including nodules, pustules, ulcers, and crusts on both lower limbs.
The patient’s general condition was normal. No signs of mobile lymph node enlargement or mucosal ulcers were found. No other system diseases were detected.Laboratory examination revealed normal results of blood cell count, erythrocyte sedimentation rate, and liver and renal functions.The patient showed an elevated level of immunoglobulin G(IgG)at 1,960g/L(reference range,751-1,560g/L),but the levels of IgA,IgE,IgM,C3,and C4 were normal. The T lymphocyte subpopulation was not detected. No immunological exponents of hepatitis B or C virus were found.Test results for human immunodeficiency virus and Treponema pallidum were negative. X-ray examination of the chest, B-mode ultrasound of the abdomen, and electrocardiography were all within normal limits.
Dermatological examination showed several areas of erythema and atrophic scars that varied in size.They were localized on both legs and ankles and had irregular margins, and some of them had ulcers in the center with slight drainage. Nodules and pustules of 1-2cm in diameter were present on both lower limbs. The sole of the foot contained a large ulcer with a diameter of 2cm,and hemorrhagic crusts covered the surface. No other lesions were detected during the dermatological examination (Fig. 1A).
Histological examination with hematoxylin-eosin staining showed proliferation of the epidermis and edema between the prickle cells. Increased numbers of neutrophils,histiocytes,and lymphocytes were distributed in the middle and lower parts of the dermis.At the periphery of the capillary vessel, the area of inflammation mainly consisted of lymphocytes. Neutrophilic microabscesses with foam cells or necrotic histiocytes were also present(Fig. 1B and 1C). Acid-fast staining revealed no findings consistent with Mycobacterium spp.
The purulent material from the ulcer on the ankle was cultured at 37 °C for 24hours.The results revealed rough floral round colonies on the agar medium. Humoral specimens from positive cultures of acid-fast bacilli within 2 months reported M.chelonae/abscessus complex growth were distinguished by gene chips. The in vitro antibiotic susceptibility of the microorganism was tested using the microdilution minimum inhibitory concentration method,and the results were shown in Table 1.
The diagnosis of M.chelonae/abscessus co-infection was established based on the clinical presentation, dermatological examination, histopathological results, and especially the specimen culture and gene chips. The patient refused to undergo intravenous injection of amikacin;therefore,based on the antibiotic susceptibility report,she was initially treated with oral clarithromycin (500mg twice a day).At a 2 months of follow-up,part of the ulcers and pustules had been scabby(Fig.1D).At the time of this writing, the patient had undergone more than 10 months of follow-up with no evidence of relapse.
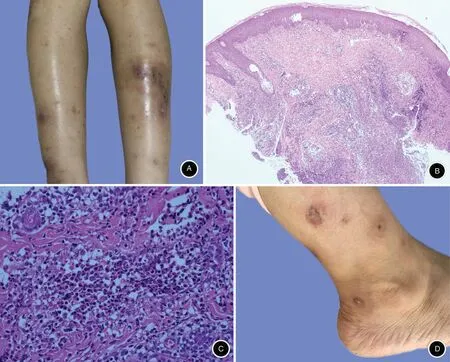
Figure 1. Clinical presentation and histopathological results of the lesions.A:Several areas of erythema were localized on both legs,and some on the left side contained ulcers in the center.The left sole contained a large ulcer with crusts measuring 2cm in diameter.B and C:Increased numbers of neutrophils, histiocytes, and lymphocytes were distributed in the middle and lower parts of the dermis. B: Hematoxylin-eosin staining, ×4. C: Hematoxylin-eosin staining, ×20. D: The initial erythema, papules, and ulcers changed to crusts and scars after treatment.

Table 1Susceptibility report of ankle drainage culture
Discussion
We have herein described a patient co-infected with M. chelonae/abscessus following surgical drainage of abscesses.
M. chelonae is included in group IV of the Runyon classification, and widely distributed throughout the environment.4It has been included within the Mycobacterium fortuitum complex, and three subspecies have been described:M.chelonei,M.abscessus,and M.chelonae-like(unnamed).However,only two subspecies are recognized:M. abscessus and M. chelonae.5Recently paper has been made to elevate the subspecies abscessus to species status.
Disseminated RGM infection often occurs in immunosuppressed patients,such as patients undergo solid organs or bone marrow transplantation,6whereas localized infections such as cellulitis and abscesses commonly present in immunocompetent patients.7In disseminated disease,the limbs are predominantly involved and more than five types of lesions are usually present(pustules,nodules,abscesses,or ulcers).8-9Although we did not have evidence to prove that the patient had disseminated diseases or was with immunodeficiency or immunosuppression, multiple kinds of lesions were present on both lower limbs.
Most standard antimycobacterials such as ethambutol,pyrazinamide,and isoniazid show little or no effect against RGM.Local susceptibility surveillance reports are required for different RGM species to guide effective therapy.6Of the parenteral antibiotics, amikacin is an important and effective agent against M.chelonae/abscessus.9Of the oral antibiotics,clarithromycin is the cornerstone of therapy for M.abscessus.9Our patient refused to undergo intravenous injection; therefore, clarithromycin was administered and was shown to be an adequate treatment. Other newer antibiotics have been successful in treating M. chelonae infections, such as faropenem and roxithromycin. At the time of this writing,the patient had shown neither evidence of drug resistance as the lesions changed to crusts nor evidence of new infection.
In conclusion, we have reported this M. chelonae/abscessus co-infection case because it has an unusual clinical presentation and was effective with the standard treatment of non-tuberculous mycobacterial infection based on time diagnosis. The key laboratory evidence is the tissue or drainage culture followed by gene chips.And antibiogramic analysis should be performed to confirm susceptibility of antibiotics and guide the treatment.
杂志排行
国际皮肤性病学杂志的其它文章
- Instructions for Authors
- Bowenoid Papulosis
- Co-Infection of Chlamydia trachomatis and Neisseria gonorrhoeae on Adult Conjunctivitis:A Case Report
- Norwegian Scabies Mimicking Seborrheic Scalp Dermatitis in a Patient with Chronic Hepatitis C
- Lipoid Proteinosis Due to Homozygous Deletion Mutation (c.735delTG) in the ECM1 Gene Presents with Seizures and Hoarseness but No Skin Involvement
- Pathogenesis of Photoaging in Human Dermal Fibroblasts