Cryptococcal meningitis with pulmonary cryptococcoma in an immunocompetent patient: A case report
2020-02-27KeeTatLeeKarYingYongHockHinChua
Kee Tat Lee, Kar Ying Yong, Hock Hin Chua
1Department of Medicine, Miri General Hospital, Sarawak, Malaysia
2Infectious Disease Unit, Department of Medicine, Sarawak General Hospital, Sarawak, Malaysia
ABSTRACT Rationale: Cryptococcal infections commonly occur in immunosuppressed patients and are uncommon in immunocompetent persons.Patient concerns: A 32 year old lady, active smoker presented with right chest pain, dry cough and loss of weight. Initial chest radiograph showed a lobulated lung mass in the right lower lobe. She developed headache and right cranial nerve palsy during admission. Various investigations were done including lumbar puncture, brain and chest imaging.Diagnosis: Cryptococcal meningitis with pulmonary cryptococcoma.Interventions: She received five months of effective antifungal treatment; however, the patient did not respond well. Subsequently, removal of pulmonary cryptococcoma was done. Outcomes: Her condition improved and she no longer had any headache.Lessons: Disseminated cryptococcosis is rare in immunocompetent patient. Our case highlights the importance of high index of suspicion and we postulate that lobectomy helped in reducing the cryptococcal burden in her body, thus facilitating better response to antifungal therapy.
KEYWORDS: Cryptococcoma; Meningitis; Immunocompetent; Antifungal; Lobectomy
1. Introduction
Cryptococcosis is an invasive fungal infection caused by encapsulated yeast, either Cryptococcus (C.) neoformans or C. gatii, which is more common in immunocompromised patients. It leads to significant morbidity and mortality among people with human immunodeficiency virus (HIV)/acquired immune deficiency syndrome (AIDS). Estimated of 223 000 cases of cryptococcal meningitis occur among people with HIV/AIDS globally each year, resulting annual fatalities of 181 000 deaths[1]. Clinical presentations of cryptococcosis differ between immunocompromised and immunocompetent person in which meningoencephalitis are predominant in HIV/AIDS positive patients, whereas in immunocompetent patients generally are asymptomatic or present with pulmonary disease[2]. We report a case of cryptococcal meningitis secondary to pulmonary cryptococcoma in an afebrile and immunocompetent patient which did not respond well to antifungal therapy alone.
2. Case report
This is a 32-year-old lady, an active smoker, presented with right-sided pleuritic chest pain, dry cough, loss of weight and appetite for one month duration. She has neither fever nor any high risk behaviour. Clinical examination revealed no abnormality. Laboratory workup was normal and serology for HIV was negative. Chest X-ray and computed tomography (CT) showed right lower lobe lobulated lung mass measuring 5.4 cm × 8.2 cm × 5.5 cm (Figures 1 and 2). She was initially treated with antibiotic; however, symptoms were not improved. Subsequently she was admitted and CT guided lung biopsy was done showing necrotic tissue. During admission, she had severe headache with blurring of vision and examination showed right sixth cranial nerve palsy. No other cranial nerves involvement and cerebellar signs were negative. CT brain contrast was done and the result was normal, subsequently proceeded with magnetic resonance imaging of the brain which demonstrated juxtacortical hyperintensities with leptomeningeal enhancement. Lumbar puncture was performed and she was diagnosed to have cryptococcal meningitis as evidence by high opening pressure and positive Indian ink in the cerebrospinal fluid. She was started on intravenous amphotericin B and tablet flucytosine and completed four weeks of induction therapy, subsequently was discharged with tablet fluconazole (400 mg/day). Unfortunately, her condition did not improve despite on antifungal therapy for five months. She had few admission in which presented with recurrent headache and required lumbar puncture for symptomatic relieve. Chest X-ray was repeated and there was no improvement of lung lesion compared to pre-treatment. She was subsequently referred to cardiothoracic team and right lung lobectomy was performed to remove the pulmonary cryptococcoma. Histopathological examination showed evidence of granulomatous inflammation in hematoxylin and eosin stain and presence of rounded organism with surrounding thick capsule (Figure 3). Post-operatively, her condition improved and she no longer had any headache requiring admission for lumbar puncture.
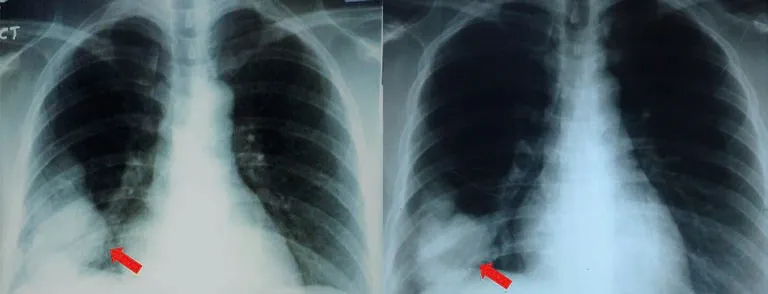
Figure 1. A 32 year old lady, active smoker presented with right-sided chest pain, dry cough and loss of weight. Chest X-ray shows a lobulated mass (red arrow) in the lower lobe of the right lung. (A) before treatment; (B) after 5 months of antifungal therapy.
This care report was approved by author’s national institute of health (NMRR-19-3396-52148) and written permission for publication has been obtained from the patient.

Figure 2. A 32 year old lady, active smoker presented with right-sided chest pain, dry cough and loss of weight. CT Thorax demonstrates a lobuted mass (red arrow) at the posterobasal segment of the right lower lobe and abutting on the dome of the right hemidiaphragm.
3. Discussion
C. neoformans meningoencephalitis is the most frequently encountered manifestation of cryptococcosis. Cryptococcus can invade numerous parts of human body including the lung, central nervous system, skin, gastrointestinal tract and skeletal system[3].
Pulmonary cryptococcosis is an uncommon infection found worldwide. Delays in diagnosis lead to increase in morbidity and mortality among patients with cryptococcosis. Majority of patients with pulmonary cryptococcosis, cough was the only symptom present and one-quarter had no respiratory symptoms[4]. Radiographic features of pulmonary cryptococcosis are nonspecific. It could appear as mass lesion, consolidation or lung cavity on chest radiograph[5]. However, the findings are different in immunocompromised host as these patients usually have more severe infection and disseminated disease. In our case, patient presented with lower lobe lobulated lung mass which can mimic lung cancer. Our patient probably acquired C. neoformans infection via inhalation into her lungs resulting in pulmonary cryptococcoma, and then disseminated to her brain, which lead to symptoms of headache and blurring of vision.
The choice of treatment for cryptococcosis depends on both the host’s immune status and anatomic sites of involvement. For asymptomatic pulmonary cryptococcosis in immunocompetent hosts, several studies have suggested that careful observation may be warranted[6]. In the case of symptomatic infection, indicated treatment is fluconazole, 400 mg/day for 6 to 12 months[6]. However, no guidelines describe the management of pulmonary cryptococcoma in the presence of cryptococcal meningitis.
We searched the studies pertaining to cryptococcal meningitis with pulmonary cryptococcoma in PubMed. We found 21 published articles. However, we identified only four articles describing treatment for patients with concurrent cryptococcal meningitis and pulmonary cryptococcoma, in which four cases underwent surgical resection of pulmonary cryptococcoma[7-10] (Table 1). All of them were male immunocompetent patients. Duration of antifungal therapy prior to surgery ranged from 1 to 5 months and all had good outcomes after surgery.

Figure 3. Photomicrographs showed (A) cavitatory destruction of lung parenchyma with numerous epitheloid granulomas (arrow) (H&E, ×40). (B) epithelioid granuloma with central encapsulated yeast (arrow). (C) innumerable encapsulated yeast (arrow) consistent with cryptococcus spp. (H&E, ×400). (D) mucicarmine stain highlights the the yeast capsule of cryptococcus in red (arrow).
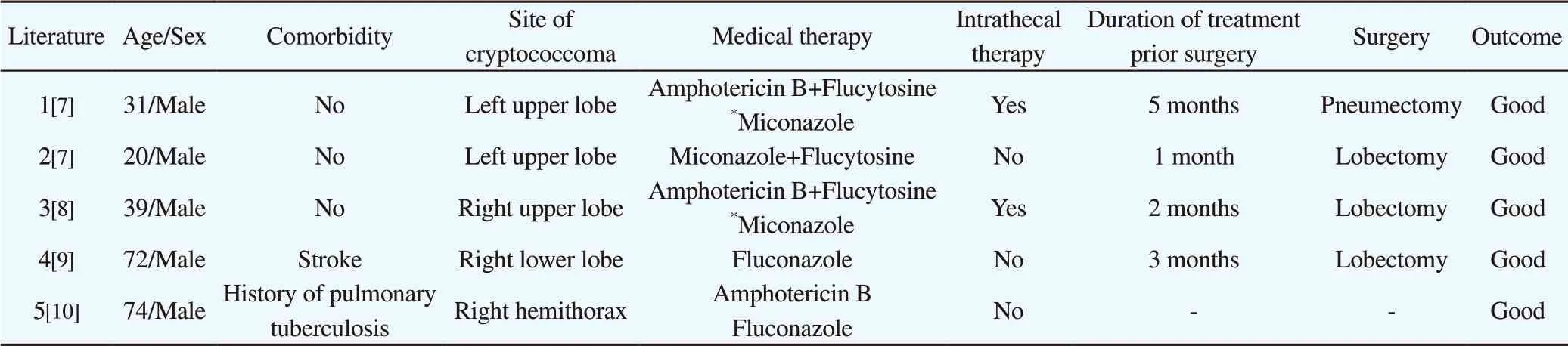
Table 1. Demographic, clinical characteristics, treatment and prognosis of the 4 cases with pulmonary cryptococcoma and cryptococcal meningitis.
Our patient was presented with disseminated cryptococcosis which manifested as cryptococcal meningitis and pulmonary cryptococcosis. Therefore, induction therapy with amphotericin B with flucytosine was indicated. She did not respond well to antifungal therapy alone. Removal of cryptococcoma in the lung as in this case, helped her response to antifungal therapy and prevented further hospitalization. Our postulation was that the lobectomy helped in reducing the cryptococcal burden in her body thus facilitating better response to antifungal therapy.
Conflicts of interest statement
The authors declare that there are no conflicts of interest.
Acknowledgments
The authors acknowledge Dr. Suhashini, pathologist from Sarawak General Hospital for providing figures of histopathological examination. We thank the Director-General of Health Malaysia for the permission to present these findings.
Authors’ contributions
KTL and KYY were involved in conception of study and drafting of manuscript. KTL, KYY and HHC contributed in data analysis, critical revision of the manuscript and also final approval of manuscript.
杂志排行
Asian Pacific Journal of Tropical Medicine的其它文章
- The phytochemical and pharmacological properties of artocarpin from Artocarpus heterophyllus
- Prevalence and genotype distribution of hepatitis B virus among migrant workers in Lombok Island, Indonesia
- Salivary gland antigens of laboratory-bred Phlebotomus sergenti and their immunogenicity in human volunteers in laboratory condition
- Indoor spray and windows screens effects on dengue vector density after space spraying in a field trial
- Sandfly fauna and ecological analysis of Phlebotomus orientalis and Phlebotomus martini in the lowland foci of visceral leishmaniasis in Somali Regional State, southeast Ethiopia
- Orostachys japonicus ethyl acetate fraction suppresses MRSA biofilm formation
