Application of hypotonic riboflavin in corneal crosslinking in patients with keratoconus
2020-02-08
Department of Ophthalmology, Hospital Professor Doutor Fernando Fonseca EPE (Amadora-Sintra), Lisbon 2720276, Portugal
Abstract
•KEYWORDS:keratoconus; cross-linking; riboflavin, thin cornea
INTRODUCTION
Keratoconus is a disorder that is characterized by conical shape ectasia and progressive thinning of the cornea, which cause irregular astigmatism and myopia, resulting in a significant decrease in visual acuity[1-3]. Its pathophysiology is not completely known, but seems to consist mainly of a reduced number of connections between collagen fibres and increased activity of proteolytic stroma enzymes, compared to normal corneas. These changes result in greater biochemical and biomechanical fragility of the corneal stroma with keratoconus[1-3].
Currently, corneal cross-linking (CXL) is the only treatment option that allows for the stabilisation or even decrease of keratoconus progression, as it acts precisely on the biochemical and biomechanical characteristics of the stroma, attenuating or reverting the aforementioned changes and strengthening the corneas with keratoconus (action mainly evident in the previous 300 μm of the stroma)[4-8]. With the application of ultraviolet A (UV-A, 370 nm) and riboflavin (photosensitiser) in the presence of oxygen, an oxidative photopolymerization reaction occurs, resulting in the creation of new covalent bonds between collagen fibrils[5-8]. Riboflavin also has a "buffering" effect that protects the incidence of UV-A radiation in deeper ocular structures, such as the corneal endothelium, lens, and retina[5-9]. Therefore, the main limitation of the application of CXL in thinner corneas is that their reduced thickness increases the risk of absorption of UV-A by the endothelium, with subsequent injury of same, as demonstrated in the study by Kymionisetal[5-9]. In this context, Wollensaketal[11], pioneers in 2003 of CXL treatment to halt the progression of keratoconus, have demonstrated that the application of the parameters of the conventional protocol (Dresden protocol, epithelium-off, with isotonic riboflavin, IR-0.1% riboflavin in 20% dextran-and 3 mW/cm2of UV-A for 30min) in corneas with a central thickness of < 400 μm achieved the cytotoxicity limit of 0.35 mW/cm2for endothelial cell damage. This is why 400 μm was the central corneal thickness limit identified for the application of the conventional CXL protocol[9-12].
However, because, in practice, this aspect limits the application of CXL in more advanced cases of keratoconus, Hafezietal[13]created a modified CXL technique in 2009 in order to increase the safety of the procedure. His technique involves the use of hypotonic riboflavin (HR, 0.1% riboflavin in 0.9% sodium chloride instead of dextran), replacing the isotonic solution. HR is applied after corneal de-epithelialization and until its saturation reaches 400 μm of central thickness. Thus, the CXL procedure in thinner corneas acquires greater safety by reducing the referred risk[13]. This effect of the HR solution is due to its lower oncotic pressure due to the absence of dextran in its constitution (relative to the IR solution), causing corneal intumescence associated with the hydrophilic properties of the stromal proteoglycans and, consequently, a transient increase of its thickness[14-18]. Despite the study by Hafezietal[13]and others that have subsequently demonstrated safety and efficacy of the procedure, its effectiveness compared with the use of IR is not yet clear. This fact is related to its possible lower biomechanical effect, as its lower oncotic pressure can result in a lower concentration and a greater distance from the collagen fibres, making it difficult to establish connections between them[14-18]. On the other hand, the same authors suggested a central corneal thickness limit of 330 μm for CXL with HR, to allow an effective CXL procedure and prevent UV-A toxicity to the endothelium[14-18].
Although promising, the various modified CXL techniques are relatively recent, and only a few studies on them have been conducted to date, which mainly include a relatively small sample, a short follow-up, and some documented limitations and/or disadvantages.
SUBJECTS AND METHODS
Retrospective study of 29 eyes of 29 patients with keratoconus from the Cornea Clinic of the Ophthalmology Department at the Hospital Professor Doutor Fernando Fonseca EPE (HFF, Lisbon, Portugal), submitted to CXL between 2012 and 2018, 15 eyes with IR application (IR group) and 14 eyes with HR application (HR group). Inclusion criteria consisted of: keratoconus in stages 1 to 3, according to Amsler-Krumeich classification; keratoconus with documented progression in the 12mo prior to the start of treatment, through refraction and/or corneal topography. Exclusion criteria consisted of: previous corneal surgery; history of herpetic keratitis; recurrent corneal infections; severe dry eye, and stable keratoconus in stage 4. All consecutive patients meeting the criteria during the period considered were included. The study followed the principles of the Helsinki Declaration and was approved by the Hospital Ethical Committee. Data was collected for the study through consultation of patients’ clinical processes and topographic parameters obtained by Pentacam©. The clinical parameters studied were: best corrected visual acuity (BCVA, in logarithm of the minimal angle of resolution scale-LogMAR), manifest value of the sphere and cylinder (in dioptres-D), and complications. The topographic parameters of Pentacam© studied were: central and thinner pachymetry (in μm) and mean (Km) and maximum (Kmax) keratometry parameters in D. Clinical (BCVA and cylinder value) and topographic parameters (Kmax) were used to identify the presence of progression, this being defined in previous studies as the loss of ≥2 lines of the BCVA or an increase of ≥1 D in the manifested cylinder or in the Kmax, in the 1y[1-4]. The aforementioned parameters were analysed during a 1-year follow-up: prior to the CXL and, in the 1 and 6mo and in the 1y, after the CXL. The results of the study parameters were compared between the 2 groups.
The division of eyes/patients between the IR and HR groups was based on the value of the central corneal thickness as measured by ultrasonic pachymetry following the de-epithelialization procedure: IR group if ≥400 μm and HR group if <400 μm. The CXL technique applied to corneas with a central thickness of ≥400 μm followed the Dresden protocol and the technique applied to corneas with a central thickness of <400 μm followed the modified technique described by Hafezietal[13]. The procedure commenced with pachymetry corneal ultrasonography, followed by corneal de-epithelialization in the central 7 mm, using a scalpel and methylcellulose sponge, and subsequent repeated determination of pachymetry. One drop of the riboflavin solution was applied every 3min for 30min: isotonic solution of 0.1% riboflavin-5-phosphate with 20% dextran if pachymetry was ≥400 μm, and hypotonic solution of 0.1% riboflavin-5-phosphate without dextran if pachymetry was <400 μm. In the cases with pachymetry >400 μm, the irradiation of the cornea with the source of UV-A radiation (370 nm) was initiated, whereas in the cases with pachymetry <400 μm, distilled water was applied before a corneal thickness ≥400 μm. Irradiation of the cornea was carried out for 30min, with the source of UV-A radiation placed at 45 mm from same, with a power of 3 mW/cm2, maintaining the application of riboflavin solution every 3min, interspersed with the application of distilled water. To ensure the safety of the technique in the HR group, the pachymetry was repeated intraoperatively after application of riboflavin. At the end of the procedure, a silicone-hydrogel contact lens was placed in each patient’s eye for better pain relief, to aid in the epithelial healing and to accelerate recovery in the eyes with corneal haze. Patients were medicated with ofloxacin and dexamethasone/neomycin eye drops.
A statistical analysis was performed with the SPSS program (Statistical Package for Social Sciences, Version 22.0), involving descriptive statistical measures; Chi-square and Fisher tests to analyse the differences between groups in qualitative variables and the Student’st-test to test the differences in quantitative variables; the assumptions of normal distribution and variance homogeneity were analysed with the Kolmogorov-Smirnov tests and Levene’s test, and in those cases where these assumptions were not satisfied, the aforementioned tests were replaced by the Mann-Whitney test. The results were considered statistically significant whenPvalue was less than 0.05 (power of the study: 95%).
RESULTS
The study sample included 29 eyes from 29 CXL-treated keratoconus patients (16 males and 13 females), with an average age of 21.4±6.0 (20.1±4.0 in the IR group and 21.3±5.0 in the HR group) years old. CXL was performed with the application of IR on 15 of the 29 eyes and with HR on the remaining 14. The results are expressed as mean±standard deviation, in absolute values, and are shown in Tables 1 and 2 and in Figures (graphics) 1 to 7. Those tables also include the statistical significance (Pvalue) of the differences between the two groups. For each group, the statistical significance difference (Pvalue) of all the parameters between the preoperative evaluation and each moment of the follow-up (Table 3).
Table1ComparisonofBCVAandrefractionbetweengroups
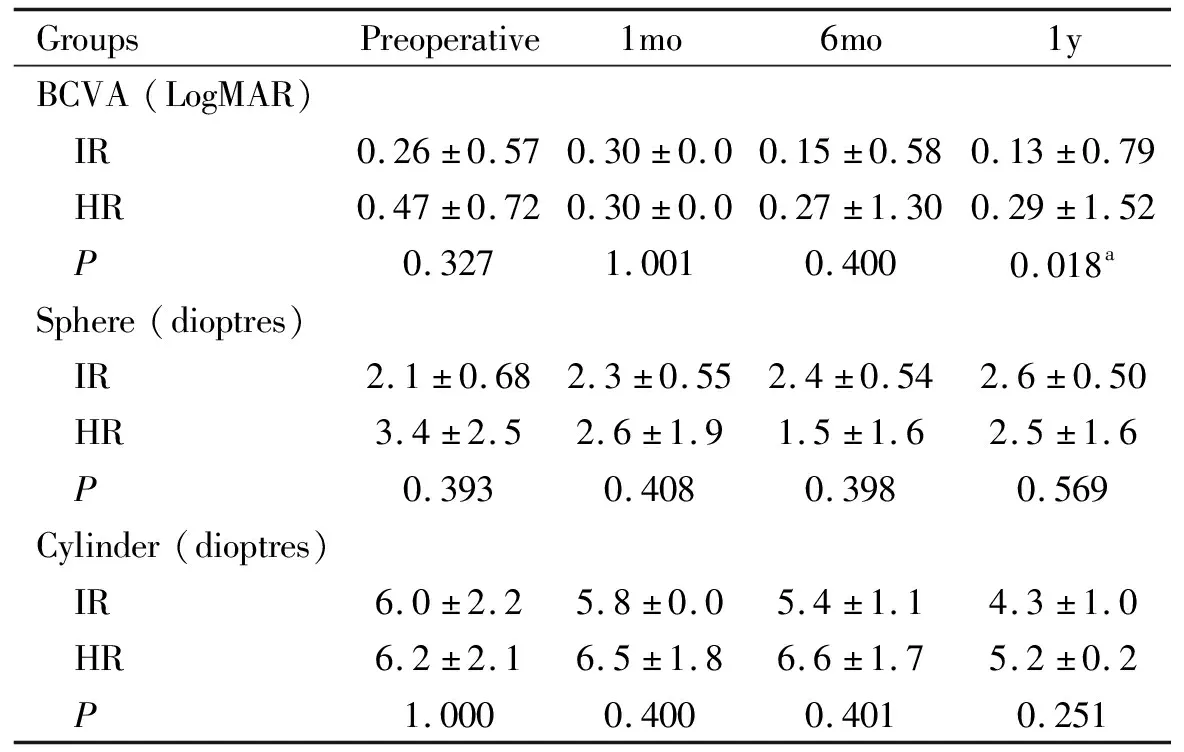
GroupsPreoperative1mo6mo1yBCVA(LogMAR) IR0.26±0.570.30±0.00.15±0.580.13±0.79 HR0.47±0.720.30±0.00.27±1.300.29±1.52 P0.3271.0010.4000.018aSphere(dioptres) IR2.1±0.682.3±0.552.4±0.542.6±0.50 HR3.4±2.52.6±1.91.5±1.62.5±1.6 P0.3930.4080.3980.569Cylinder(dioptres) IR6.0±2.25.8±0.05.4±1.14.3±1.0 HR6.2±2.16.5±1.86.6±1.75.2±0.2 P1.0000.4000.4010.251
BCVA: Best corrected visual acuity.aPvalue <0.05.
1)BCVA: there was an improvement in BCVA in both groups, without satistical significance between the preoperative evaluation and each moment of the follow-up. In the first year alone, the difference between groups was statistically significant (P=0.019), with the IR group showing a better BCVA.
2)Manifest value of the sphere and the cylinder: the sphere increased slightly in the IR group, while in the HR group it decreased. The cylinder decreased in both groups. In each group, the results were not statistically significant between the preoperative evaluation and each moment of the follow-up. Both parameters did not present statistically significant differences between the groups during follow-up.
3)Central and thinner pachymetry: a reduction in central pachymetry was observed at the 1stmonth, with a progressive increase up to the 1styear of follow-up in both groups (IR group with higher values). In the IR group, both central and thinner pachymetry showed statistically significant differences at all the follow-up moments, while in the HR group only the thinner pachymetry showed a statistically significant difference between the preoperative evaluation and the evaluations of the 1stand the 6thmonth. Differences between the groups were statistically significant in all follow-up moments except for the 1stmonth.
4)Km and Kmax: a Km reduction was observed throughout the follow-up in both groups, with only the IR group showing a statistically significant result between the preoperative evaluation and the 1styear evaluation. There were no statistically significant differences between the groups.
5)Complications: 6 eyes of each group (total of 12 eyes) presented a transient haze, with spontaneous resolution until the 3rdweek after treatment. All epithelial defects were resolved within 1wk after treatment and no cases of corneal or permanent stromal scarring were observed.
6)Progression: no eye presented progression in the 1styear in either group, according to the criteria used to define progression.
Table 2 Comparison of queratometry and pachymetry between groups
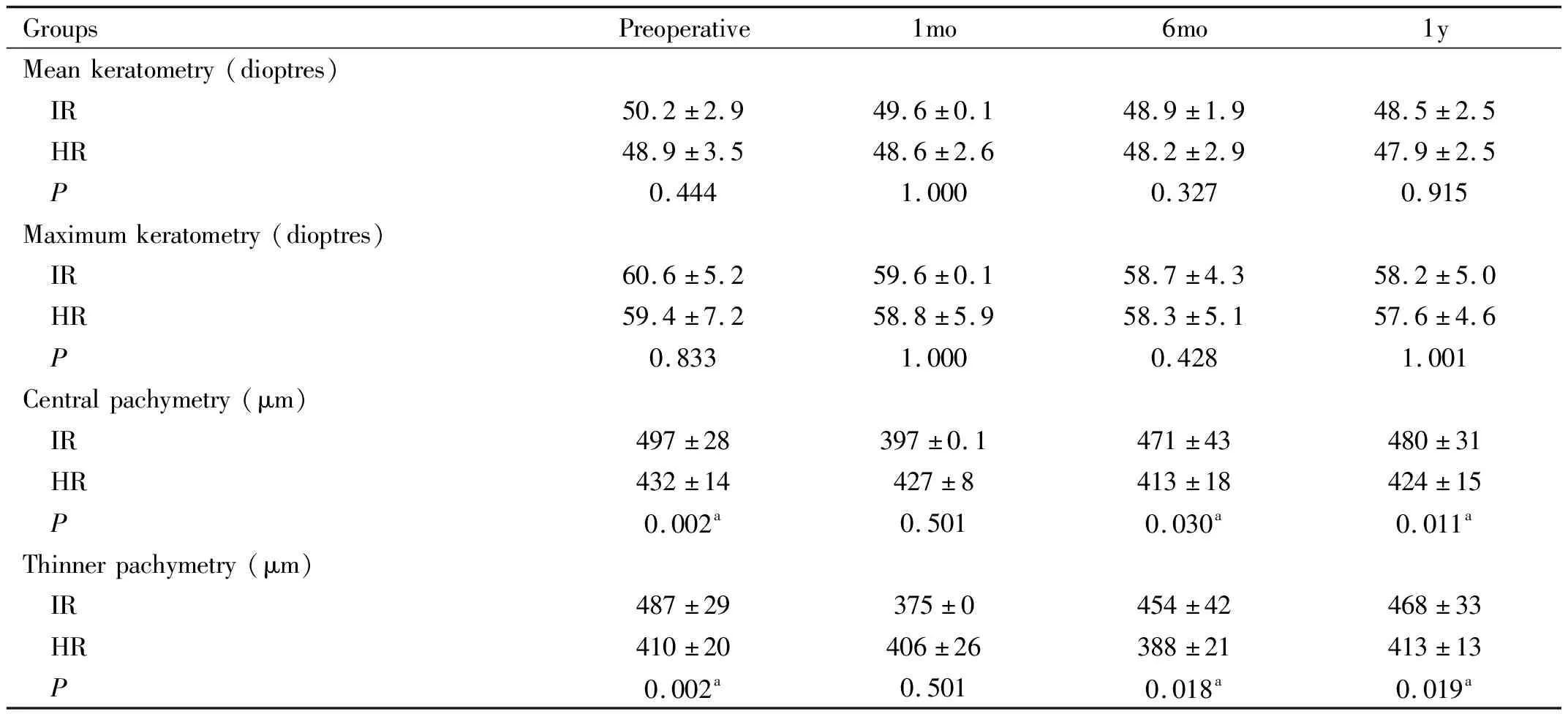
GroupsPreoperative1mo6mo1yMeankeratometry(dioptres) IR50.2±2.949.6±0.148.9±1.948.5±2.5 HR48.9±3.548.6±2.648.2±2.947.9±2.5 P0.4441.0000.3270.915Maximumkeratometry(dioptres) IR60.6±5.259.6±0.158.7±4.358.2±5.0 HR59.4±7.258.8±5.958.3±5.157.6±4.6 P0.8331.0000.4281.001Centralpachymetry(μm) IR497±28397±0.1471±43480±31 HR432±14427±8413±18424±15 P0.002a0.5010.030a0.011aThinnerpachymetry(μm) IR487±29375±0454±42468±33 HR410±20406±26388±21413±13 P0.002a0.5010.018a0.019a
aPvalue <0.05.
Table 3 Statistical significance between the preoperative evaluation and each moment of the follow-up, for each group
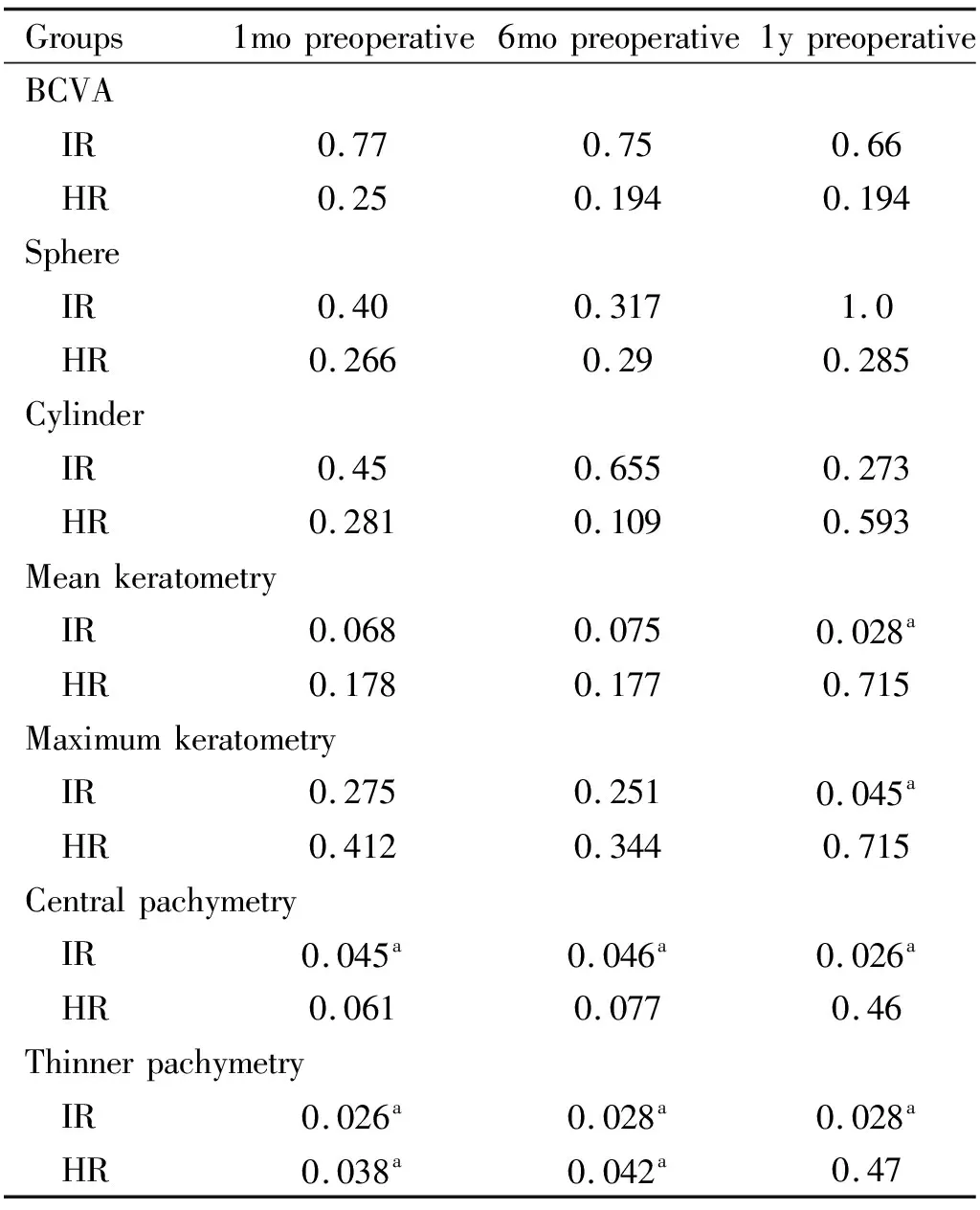
Groups1mopreoperative6mopreoperative1ypreoperativeBCVA IR0.770.750.66 HR0.250.1940.194Sphere IR0.400.3171.0 HR0.2660.290.285Cylinder IR0.450.6550.273 HR0.2810.1090.593Meankeratometry IR0.0680.0750.028a HR0.1780.1770.715Maximumkeratometry IR0.2750.2510.045a HR0.4120.3440.715Centralpachymetry IR0.045a0.046a0.026a HR0.0610.0770.46Thinnerpachymetry IR0.026a0.028a0.028a HR0.038a0.042a0.47
aPvalue <0.05.
DISCUSSION
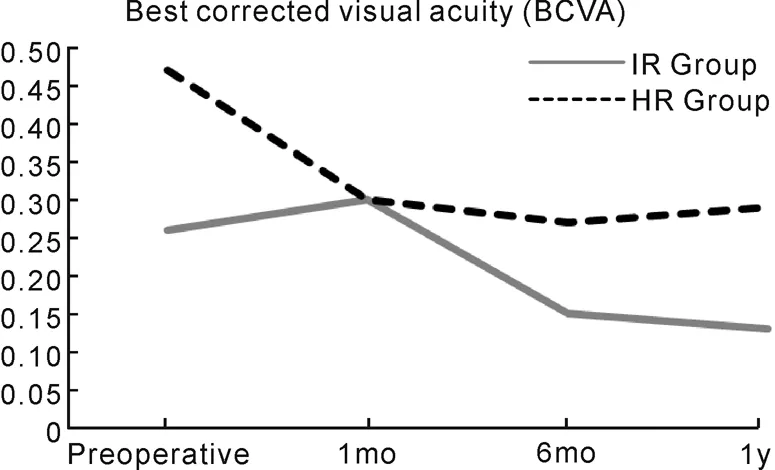
Figure 1 Best corrected visual acuity throughout follow-up.
The study showed an improvement in the studied parameters (BCVA, refraction, Km and Kmax), without relevant complications and without progression, in both groups, which is in agreement with the literature and other studies[4,16]. These results in both groups corroborate the objectives of the CXL itself, culminating in the stability or even reduction of the progression of keratoconus by strengthening the covalent bonds between the collagen fibres of the cornea. Thus, the primary objective of CXL was achieved through the application of both IR and HR.
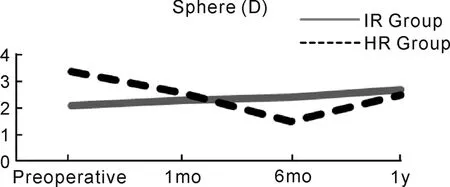
Figure 2 Value of the sphere (in dioptres)throughout follow-up.
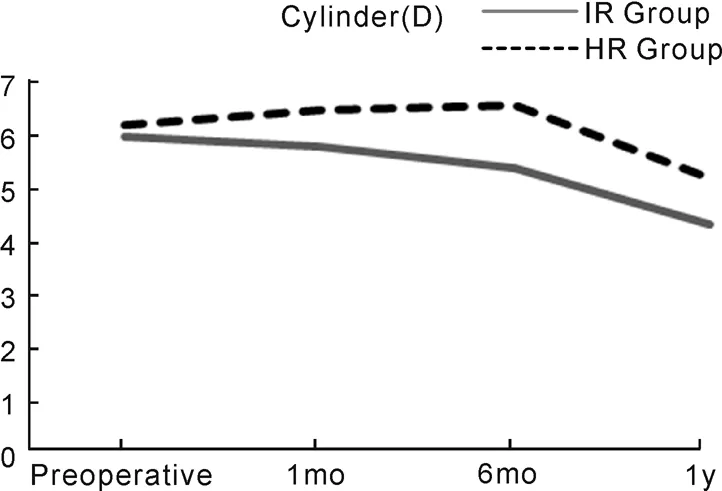
Figure 3 Value of the cylinder (in dioptres)throughout follow-up.
According to the results obtained, the application of HR seems to be an option to consider in thinner corneas. Its effect can be explained by its lower oncotic pressure, leading to an increase in corneal swelling until the corneal thickness threshold of 400 μm is reached for the procedure showing a lower risk of endothelial toxicity associated with UV-A radiation. The study by Nassarallaetal[16]confirmed the efficacy of HR application in corneas of <400 μm, with a statistically significant reduction of keratometry and BCVA in the first year of follow-up. The study by Raiskupetal[15]demonstrated no statistically significant stabilization of keratometry and of BCVA with the same follow-up period.
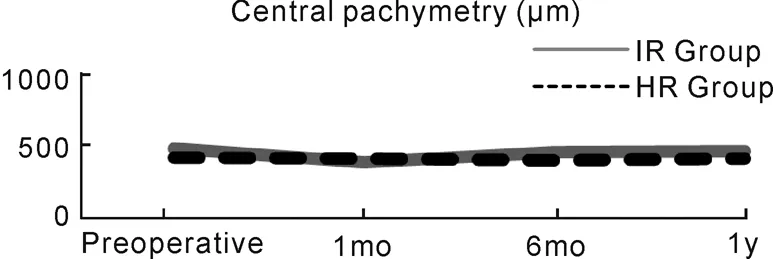
Figure 4 Central pachymetry (μm) throughout follow-up.
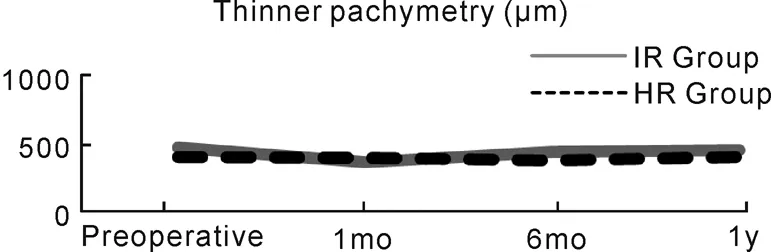
Figure 5 Thinner pachymetry (μm) throughout follow-up.

Figure 6 Central keratometry (Km) through the follow-up.

Figure 7 Maximum keratometry (Kmax) throughout follow-up.
Although our results are consistent with the literature available, there are still few comparative studies between CXL with IR and HR. Similar to our study, those conducted by Raiskupetal[15]and Nassarallaetal[16], mentioned above, also revealed more discrete results with HR, contrary to previous studies with corneas of ≥400 μm treated with IR[4,10-12]. On the other hand, the study by Rosenblatetal[14], showed that there were no statistically significant differences between IR and HR groups regarding improvement of Kmax, uncorrected visual acuity and the thickness of the cornea. The study by Chenetal[19]also showed the absence of a statistically significant difference between the IR and HR groups in relation to keratometry, BCVA and a spherical equivalent.
A theory discussed regarding the possible lower efficacy of HR is the eventual lower biomechanical effect with greater difficulty in establishing connections between collagen fibres, due to the lower oncotic pressure associated with corneal intumescence, resulting in lower concentration and greater distance from collagen fibres[14-18]. However, even if HR is not as effective as IR, showing no statistically significant change in the parameters under study, and/or showing stabilization of parameters rather than improvement, its application is still promising because by stabilizing the parameters, it is already delaying progression without any apparent increased risk for the endothelium.
Regarding the modifications in BCVA, cylinder and sphere, some studies demonstrate results similar to those obtained in our study, with varying significance; others show no relevant changes in these parameters[15-16]. The study conducted by Hashemietal[4]indicates as a possible justification the differences in sample size and base refractive error.
The changes in pachymetry in our study, with a decrease in the comparison between the initial value and the first month and with a later increase up to the first year, are in agreement with other studies[11,17-18,20-21]. Guetal[17]Hassanetal[20]suggest that the initial change is due to measurement errors due to the initial swelling of the cornea caused by the procedure. Also Wollensaketal[11]demonstrated that the swelling of the cornea depended on the degree of CXL: the higher the CXL, the smaller the swelling, and vice versa. On the other hand, de-epithelialization was initially performed, which alone can increase the rate of evaporation of stromal water and, as it is not resistant to dehydration, makes the cornea vulnerable to a reduction in its thickness, as indicated by Nassarallaetal[16]Furthermore, the effect of CXL may probably decrease corneal thickness due to the increase in endothelial cell activity caused by the initial exposure to UV-A radiation, as indicated by several authors, such as Holopainenetal[21], with subsequent stabilization and increased thickness. Still in relation to pachymetry, we can highlight the study of the recent study by Hanetal[18]on the comparison of CXL results in 4 groups of patients with different corneal thicknesses (including one group with a corneal thickness of < 400 μm submitted to HR, as opposed to another 3 groups with a corneal thickness of ≥ 400 μm submitted to IR)[18]. In this study, the authors not only confirm the success of CXL in delaying the progression of keratoconus but also emphasize the existence of a negative linear correlation between corneal thickness and Kmax, meaning that more advanced cases of keratoconus (therefore with thinner corneas) seem to obtain a greater benefit from the flatting effect of CXL[18].
Regarding complications, the results are also in agreement with the literature and other studies, including the presence of corneal haze[21]. In our study, the absence of complications affecting the final outcome of CXL supports the safety of applying HR. This is also a controversial topic given that some studies, as one study of Kymionisetal[23], documented no complications after standard CXL with the standard IR in patients with corneal thickness < 400 μm. In that study, the author showed that the corneal endothelium (evaluated postoperatively by corneal confocal microscopy) did not undergo any significant changes.
The limitations included the retrospective profile of the study, a small sample and a short follow-up. These limitations are considered relative, since they are resolved with the continuity of the study. It is a type of study that may have an impact on clinical practice, as it allows more effective and safer treatment of more advanced cases of keratoconus, associated with thinner corneas, where current treatment options are still limited.
To conclude, the application of HR is promising in the treatment of thinner corneas, stopping the progression of keratoconus without seeming to compromise the safety of the procedure. Further studies on this type of procedure, including an increase in the number of cases and greater follow-up, will contribute to a greater and better knowledge of its long-term efficacy and safety in clinical practice.
