Good accuracy of the alpha-defensin lateral flow test for hip periprosthetic joint infection: A pilot study in a retrospective cohort of 52 patients
2020-01-16JesseWPKuiperPieterPanderStanVos
Jesse WP Kuiper, Pieter Pander, Stan J Vos
Jesse WP Kuiper, Stan J Vos, Department of Orthopedic Surgery, Noordwest Ziekenhuisgroep,Alkmaar 1815 JD, Netherlands
Pieter Pander, Centre for Orthopedic Research Alkmaar, Noordwest Ziekenhuisgroep, Alkmaar 1815 JD, Netherlands
Abstract
Key words: Periprosthetic; Arthroplasty; Replacement; Hip; Infection; Periprosthetic joint infection; Alpha-defensin; Synovasure
INTRODUCTION
Periprosthetic joint infection (PJI) is one of the most serious complications of total hip arthroplasty (THA). It generally requires one or more surgeries, weeks of hospitalization and long-term antibiotic treatment. Overall, it is a considerable financial and logistic burden to hospitals and the health care system in general[1,2]. The patients themselves, however, are the ones most afflicted by this complication.Treatment methods range from curative therapy with revision arthroplasty to months of living without a functioning hip articulation (Girdlestone procedure) or to life-long suppressive antibiotic therapy (for inoperable patients with a low grade PJI)[1].
Because treatment of PJI differs from other revision indications, it is important to accurately exclude PJI before revision surgery takes place. PJI can be challenging to diagnose and several definitions have been proposed in the past. The most recent(modified) definition by the Musculoskeletal Infection Society (MSIS) includes various laboratory values and aspiration results[3]. This definition has been used as the gold standard for PJI in the last years. However, in the last years, two new definitions have been suggested: The European Bone and Joint Infection Society (EBJIS) has recently proposed other diagnostic criteria which may have a lower threshold for the detection of PJI, and therefore possibly a higher specificity[4]; the 2018 International Consensus Meeting (ICM) criteria includes the most recent tests into a cumulative score, with substantially higher sensitivity and specificity[5].
None of the criteria are ideal in terms of speed, ease of use, high sensitivity and high specificity. Therefore, new diagnostic tools are constantly being developed. One of the most studied new diagnostic markers of the last few years is the determination of alpha-defensin (AD), a protein released by white blood cells in synovial fluid. Two different versions to test this exist: The AD immunoassay test, which is a laboratory test with a readout within 24 h; and the Synovasure® lateral flow test (Synovasure®,Zimmer Biomet, Warsaw, Indiana). This point-of-care test can show directly whether an arthroplasty might be infected, but may have lower accuracy[6-8].
The aim of this pilot study was to identify a cohort of patients in whom the AD lateral flow (ADLF) test was already performed in the last two years in our hospital,and to assess the accuracy of the ADLF test for this cohort [sensitivity, specificity,positive predictive value (PPV), negative predictive value (NPV)] by comparing it to the current gold standard for the diagnosis of PJI. As a secondary aim, the more recently proposed EBJIS and 2018 ICM definitions were applied to the cohort as well,to investigate the differences between the definitions.
MATERIALS AND METHODS
Since 2015, one of the orthopedic surgeons in our hospital, with a subspecialty in PJI,started using the ADLF test (Synovasure®, Zimmer Biomet, Warsaw, Indiana) for all aspirations of potential hip PJI. This cohort was identified by using our own database and cross-referencing with surgical records. Data were retrospectively collected and analyzed. Patients were included if an ADLF test was performed after aspiration of THA or hemi-arthroplasty (HA) in the study period. Exclusion criteria were:significantly incomplete medical record data (e.g., missing culture results, unavailable data on surgery performed elsewhere), aspiration of other arthroplasty than THA or HA, unavailability of ADLF test (not performed or missing data).
Intervention
All patients underwent sterile aspiration of the hip joint as part of the diagnostic work-up for a painful or poorly functioning hip arthroplasty, between January 2015 and March 2018. This aspiration was performed in the operating room under sterile conditions with the help of fluoroscopy. After aspiration, the ADLF test was performed according to manufacturer guidelines if enough material was available(e.g., no dry tap). A white blood cell count (WBC) and polymorphonuclear neutrophil percentage (PMN%) were performed, and one or two samples were used for culturing in blood culture bottles (aerobic and anaerobic).
Revision surgery
During revision surgery, at least 6 tissue cultures were collected, from joint capsule/synovium, acetabular and femoral interface. Sonication and histopathology were not standardly performed during the study period. Antibiotic treatment was guided by prior cultures results, or vancomycin (1000 milligrams twice daily) was administered until culture results were known, which could take up to 14 d.
Data
After identification of all patients that underwent aspiration, the following data were collected: patient characteristics; arthroplasty details (time after initial surgery, hemior total hip arthroplasty, articulation, use of cement); C-reactive protein (CRP),erythrocyte sedimentation rate (ESR), serum leukocyte count and presence of a sinus tract at presentation; aspiration characteristics (amount, aspect, ADLF test results,WBC and PMN%, number of cultures and culture results); follow-up data (revision performed, intra-operative histology and culture results, diagnosis, PJI criteria met).
PJI definition
Three recent definitions of PJI for calculation of test accuracy were used. The MSIS definition was used as the standard[3]. EBJIS and ICM definitions were also used for comparison[4,5]. See Table 1, Table 2, Table 3, Table 4 and Table 5.
Study parameters
The main aim of this study was to assess sensitivity and specificity with PPV and NPV of the ADLF test, using the MSIS criteria for PJI as mentioned above. The second aim was to compare these criteria with the EBJIS and 2018 ICM criteria.
Statistical analysis
To assess the performance of the ADLF test, the sensitivity, specificity, PPV and NPV were calculated. Except for age, the scale variables were described using the median and the range regarding a non-normal distribution measured by means of the Onesample Kolmogorov Smirnov test. 95%CI were calculated and are described.
RESULTS
Demographics
Between January 2015 and December 2017, 83 hip aspirations were conducted. 31 patients were excluded because the ADLF test was not performed. Therefore, a total of 52 patients (52 aspirations) were included in this pilot study, with a mean age of 72 years. See Table 6 for demographics and comparison with the excluded patients. Themedian time between primary surgery and aspiration was 35 mo (range 3-266 mo)and 46 (88%) patients had a THA. 31 of 46 THA patients had a metal on polyethylene articulation. The median CRP and ESR before aspiration were 6 mg/L (range 1-195 mg/L) and 13 mm/h (range 3-120 mm/h) respectively, and the median WBC in synovial fluid was 800 cells/μL (range 10-264.000 cells/μL).
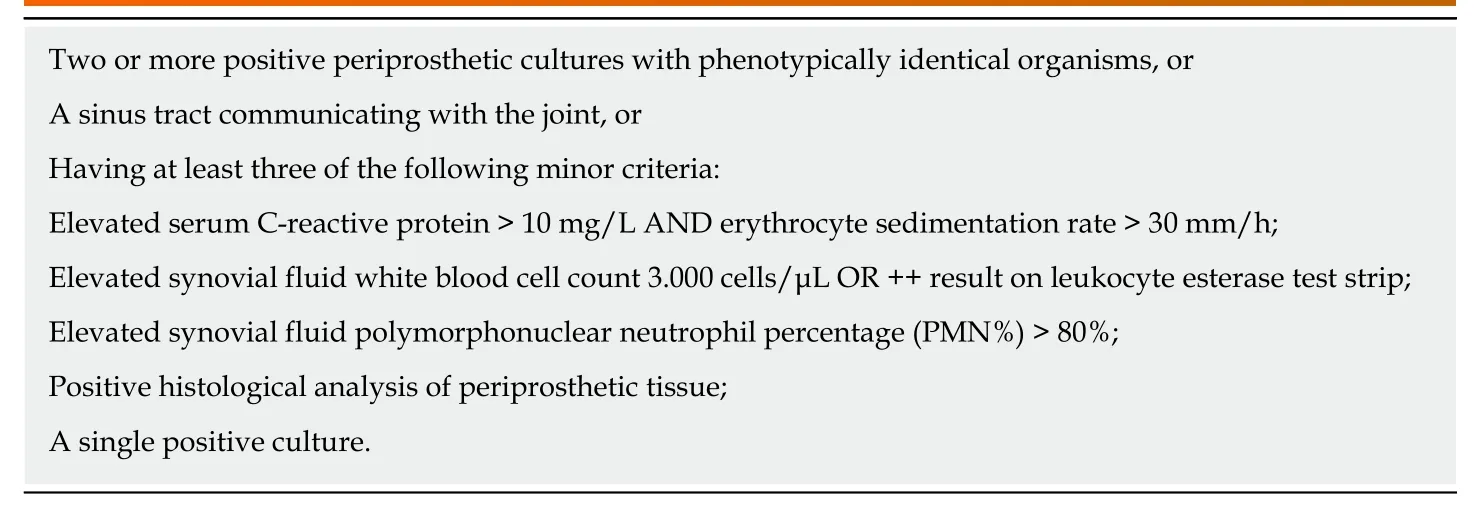
Table 1 Modified Musculoskeletal Infection Society criteria for periprosthetic joint infection definition[3]
ADLF test
In 11 patients (21%) the ADLF test was positive. According to the MSIS criteria, 6 patients had a PJI. Using these criteria, sensitivity was 100% (CI: 54%-100%),specificity was 89% (CI: 76%-96%), PPV was 55% (CI: 34%-73%) and NPV was 100%.The overall accuracy was 90% (CI: 79%-97%). None of the ADLF test results were false negative and 5 were false positive (Figure 1). One of the false positive cases had a metal-on-metal (MoM) articulation. See Table 7 for details on all positive ADLF tests or inconclusive/positive criteria.
Revision surgery
In total, 19 patients underwent revision surgery after aspiration. 10 of these had no PJI suspicion and underwent direct revision. In 8 patients, PJI was suspected because of aspiration results or symptoms, and a two-stage revision was performed. In one patient, debridement, antibiotics and implant retention (DAIR) was performed because PJI was classified as acute hematogenous (symptom duration of 8 d with a prior well-functioning THA).
PJI
Of 6 patients with PJI, 5 patients (83%) underwent revision surgery. One patient was treated with suppressive antibiotics because of extensive co-morbidity, and died 5 mo later, unrelated to PJI. Seven cases (of 19 revisions) had positive cultures (Table 8). In 4 of these 7 patients, the micro-organism found intraoperatively corresponded to aspiration culture results. The other 3 patients had negative preoperative synovial cultures. Two of these three did not meet PJI criteria (both MSIS and EBJIS), as they had only one positive intraoperative culture with a low virulence micro-organism(Cutibacterium acnesandStaphylococcus capitis). Both patients underwent direct revision, without macroscopic suspicion of PJI, and were free of symptoms at the last follow-up. One patient was treated with DAIR, as described above. The other 4 patients with positive cultures underwent two-stage revision. See Table 8 for microbiology characteristics.
MoM
Three patients (6%) had a MoM hip articulation. One patient was not suspected of PJI.The 2 other patients had a positive ADLF test (67%): 1 patient did not meet MSIS PJI criteria, but did have PJI according to EBJIS criteria (elevated WBC count of 5170 cells/μL). The last patient had PJI, according to both MSIS and EBJIS criteria. Due to severe comorbidity, this patient was considered inoperable, as a result of which intraoperative cultures were never obtained.
EBJIS criteria
When adhering to the criteria by the EBJIS, PJI was found in 14 patients and the ADLF test had a sensitivity of 71% (CI: 42%-92%), specificity of 97% (CI: 86%-100%), PPV of 91% (CI: 58%-99%) and NPV of 90% (CI: 80%-96%). The overall accuracy was 90% (CI:79%-97%). Using the EBJIS criteria, 4 ADLF test results were false negative and one was false positive (Figure 1).
2018 ICM criteria
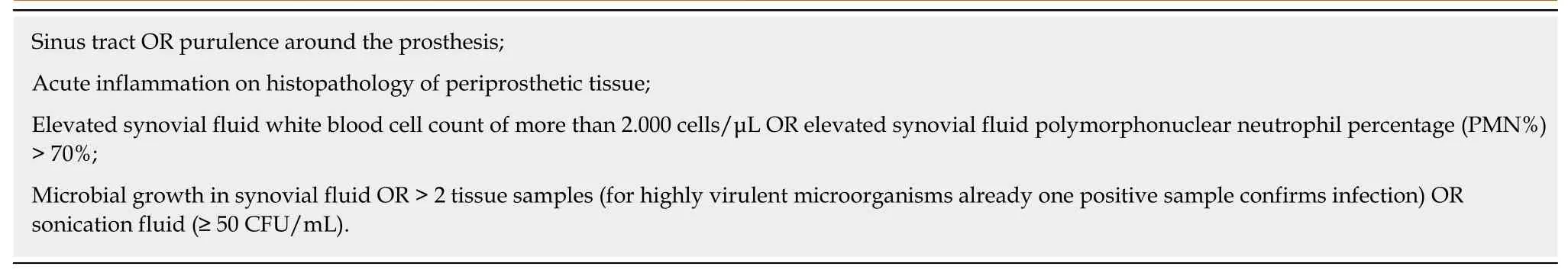
Table 2 European Bone and Joint Infection Society criteria for periprosthetic joint infection definition. One or more criteria fulfilled means positive periprosthetic joint infection diagnosis[4]
Ten patients had PJI according to these criteria, and 40 patients had no PJI. Two cases were inconclusive, 1 with positive and 1 with negative ADLF test. Excluding these cases, no false positives and false negatives were found, and the ADLF test had 100%sensitivity (69%-100%) and specificity (91%-100%). When classifying these cases as infected, as they are likely to be treated as infected cases, sensitivity was 91% (62%-100%), specificity 100% (91%-100%). PPV, NPV and accuracy were 100%, 98% (86%-100%) and 98% (90%-100%), respectively. See Figure 1.
DISCUSSION
In this study the accuracy of the ADLF test was assessed in 52 patients with a suspicion of hip PJI.
The measured sensitivity and specificity of the ADLF test were 100% and 89%respectively, with an overall accuracy of 90%. In comparison, when applying the EBJIS criteria, sensitivity and specificity were 71 and 97% respectively. Overall accuracy was the same, 90%. When using the new 2018 ICM criteria, a sensitivity of 91% and a specificity of 100% were found, with an accuracy of 98%.
The existing literature describes a large range in sensitivity and specificity. This can partly be explained by study-related factors. The results for sensitivity range from 67.0% to 97.1% and for specificity from 82.4% to 100%[4,6,8-11]. The results of the current study are comparable to these studies.
Renzet al[4]also reported results of the ADLF test when using EBJIS criteria, and found a sensitivity of 54.4%, specificity of 99.3%, PPV of 97.7%, and NPV of 78.6% (for MSIS criteria these numbers were 84.4%, 96.4%, 86.4% and 95.8%, respectively). In a cohort of 212 patients, 45 patients had PJI according to MSIS criteria, and 79 with the use of EBJIS criteria. With this lower threshold, the prevalence of PJI is higher and the number of false positives is lower. This is similar for the current study. The only study on the new 2018 ICM criteria[5]is the one in which the definition is proposed, and they described no accuracy of the AD test alone. Since the AD test is used in the criteria,one may argue that it is not a good gold standard to assess the accuracy of the AD test itself.
In previous studies, metallosis was often excluded due to false positive results[6,8,12-14]. It is known that patients with a MoM articulation may develop adverse local tissue reactions (ALTR) due to metal wear debris. Even with other articulations,metal debris can be found (e.g., with taper-cup impingement or other taper related problems)[15]. Differentiating between PJI and ALTR can be challenging as patients may have elevated inflammatory parameters, peri-articular purulent appearance,falsely elevated WBC and a false positive ADLF test[8,15]. Of 5 false-positive ADLF tests, 1 was a case of metallosis. Other studies found even higher rates of metallosis among the false-positive cases, although the numbers are small: 1/3, 2/4 and 3/5[11,16,17]. One study excluded 3 false positive cases because of metallosis[8]. A recent Dutch study described 1 case of metallosis, with a negative ADLF test in a cohort of 37 patients[18]. Okrojet al[15]studied the results of AD testing in 26 cases of metallosis.They found 1 true positive, and 8 false positive results (31%). Therefore, the value of the ADLF test in metallosis cases should be interpreted critically and with caution.
经过长期努力,各地面对城市洪涝灾害时的反应速度不断加快,处理措施更加完善,应急处置能力不断提高。北京市2013年汛期共出动抢险人员50万人次,排除积水30处次,处理塌方和滑坡40点次,转移群众3.7万人次,有力保障了人民生命财产安全。上海市遭遇2013年第23号强台风“菲特”袭击,全市普降大暴雨到特大暴雨,上海各地区、各行业按照防汛责任制和工作预案,迅速形成了较完整的防汛抗灾组织体系,出动抢险、排水、巡查人员2万余人次,出动各类应急抢险车辆1200余台次,动员社会各界力量广泛参与防风抗灾,全力保障城市安全运转。
In this cohort, 6 patients with painful or non-functioning hemiarthroplasty were included. In 2 of 6 cases the ADLF test was positive. According to MSIS criteria, both were false positive. Using EBJIS criteria, 1 true positive, 1 false positive and 1 false negative were found. With the 2018 ICM criteria, 1 true positive and 1 positive in an inconclusive case were found. No other studies described AD testing of hip hemiarthroplasties. Further studies are needed to provide guidance on AD testing for painful hip hemiarthroplasties.
Within the scope of this study, its limitations are acknowledged. The number of patients was relatively small, and due to the retrospective design, not allmeasurements needed for the PJI criteria were performed. Furthermore, ADLF test was not performed in all patients that underwent aspiration, mostly due to insufficient amount of aspiration fluid or bloody fluid aspiration. Therefore, selection bias may have occurred. Although several statistical methods exist to address missing data, we believe these are more useful for big data trials than for this retrospective study[19].

Table 3 New 2018 International Consensus Meeting scoring criteria for periprosthetic joint infectiondefinition[5]: Major criteria (at least one of the following)
Because only hip arthroplasty patients were included in this cohort, comparison with previous studies is more difficult, as most other studies described results of both hip and knee PJI.
Further research is crucial, considering the variety in sensitivity and specificity in different studies. A prospective follow-up study has already been started to evaluate the ADLF test in a larger, prospective cohort, in which a comparison to the leukocyteesterase test will also be made.
In conclusion, in a cohort of 52 patients that underwent aspiration for a painful or poor-functioning hip arthroplasty, the ADLF test had a sensitivity of 100% and specificity of 89% and an overall accuracy of 90%. Other definition criteria showed slightly different test specifics but overall accuracy was high for the EBJIS and 2018 ICM criteria as well. The ADLF test is an easy-to-use point of care test, which requires little material and can provide a quick perioperative result. This can be useful during revision surgery or when aspiration yields almost no synovial fluid. Nevertheless,caution is advised when interpreting the results, in particular when metallosis is present or possible.
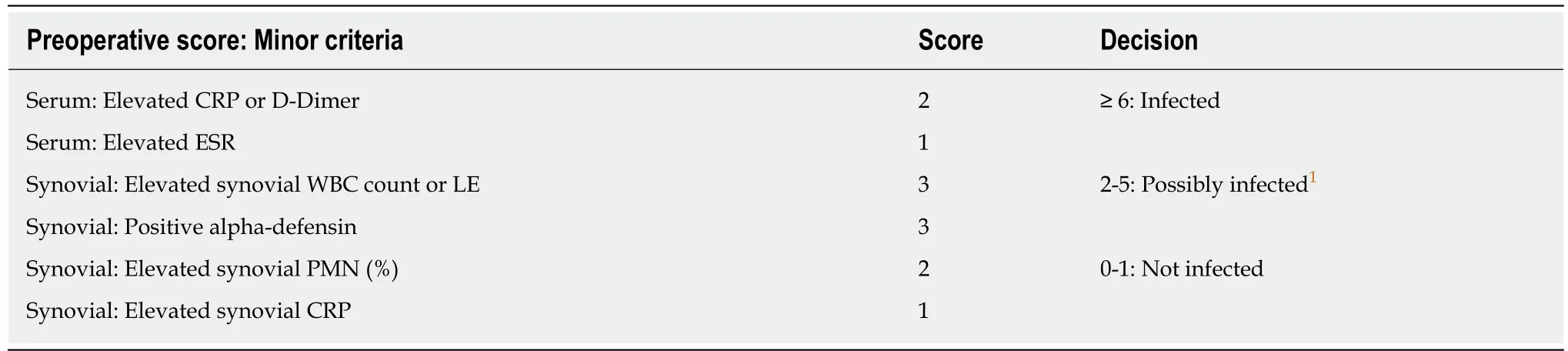
Table 4 New 2018 International Consensus Meeting scoring criteria for periprosthetic joint infection definition[5]: Preoperative diagnosis

Table 5 New 2018 International Consensus Meeting scoring criteria for periprosthetic joint infection definition[5]: Intraoperatieve diagnosis
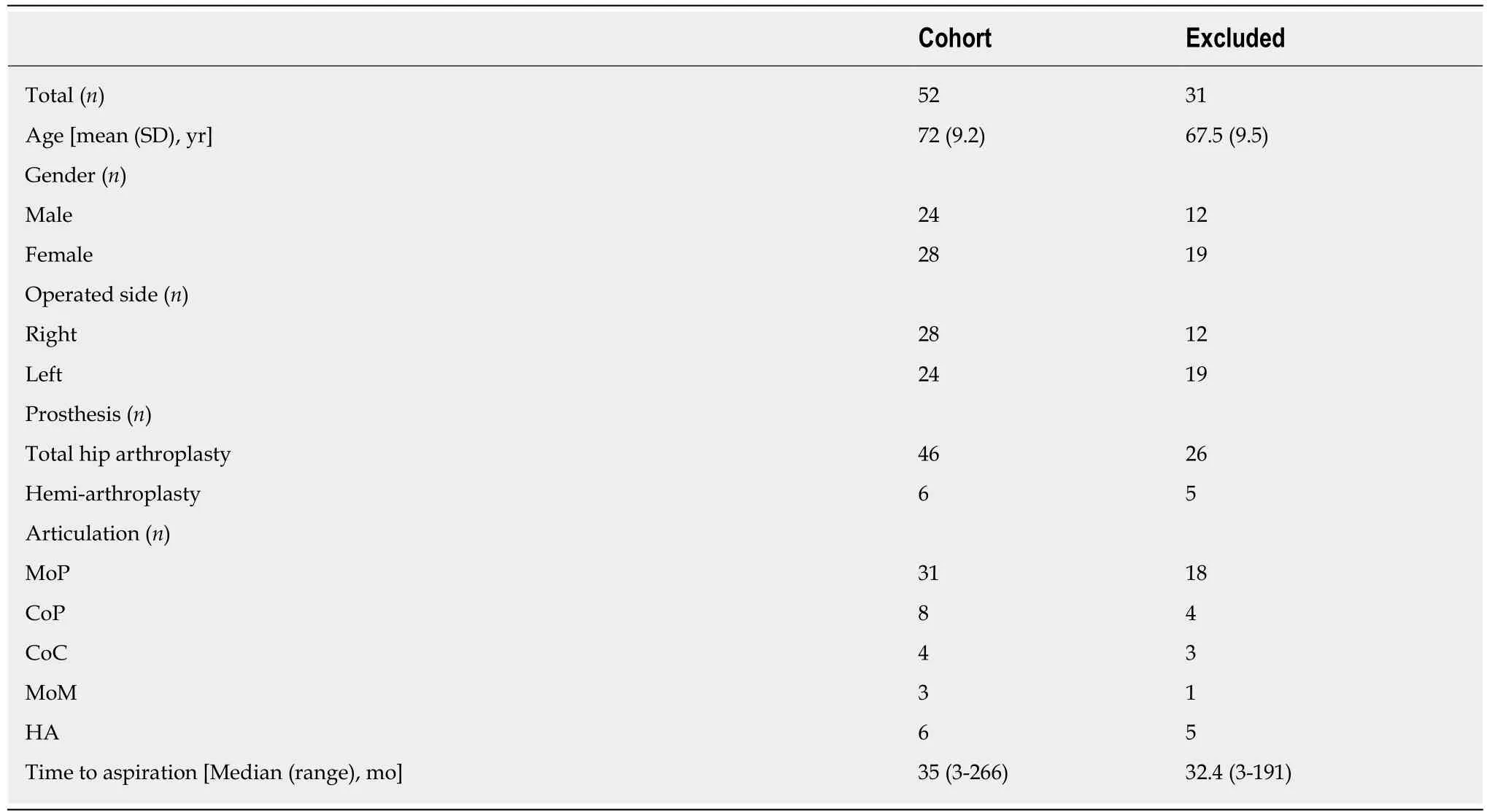
Table 6 Demographics of the described cohort and the group of excluded patients (no alpha-defensin lateral flow test performed)
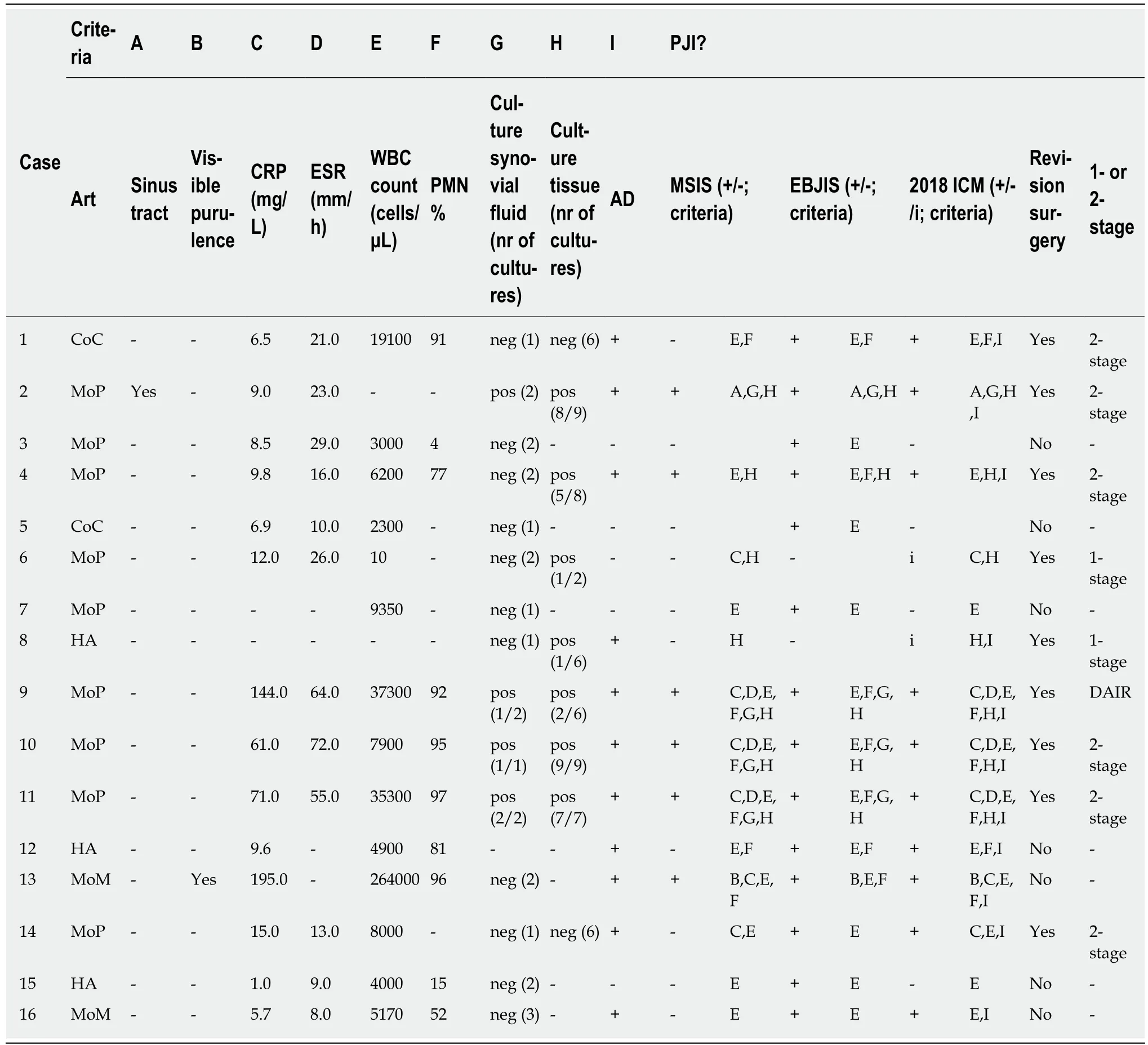
Table 7 Characteristics of all patients with positive alpha-defensin lateral flow test and/or positive or inconclusive criteria
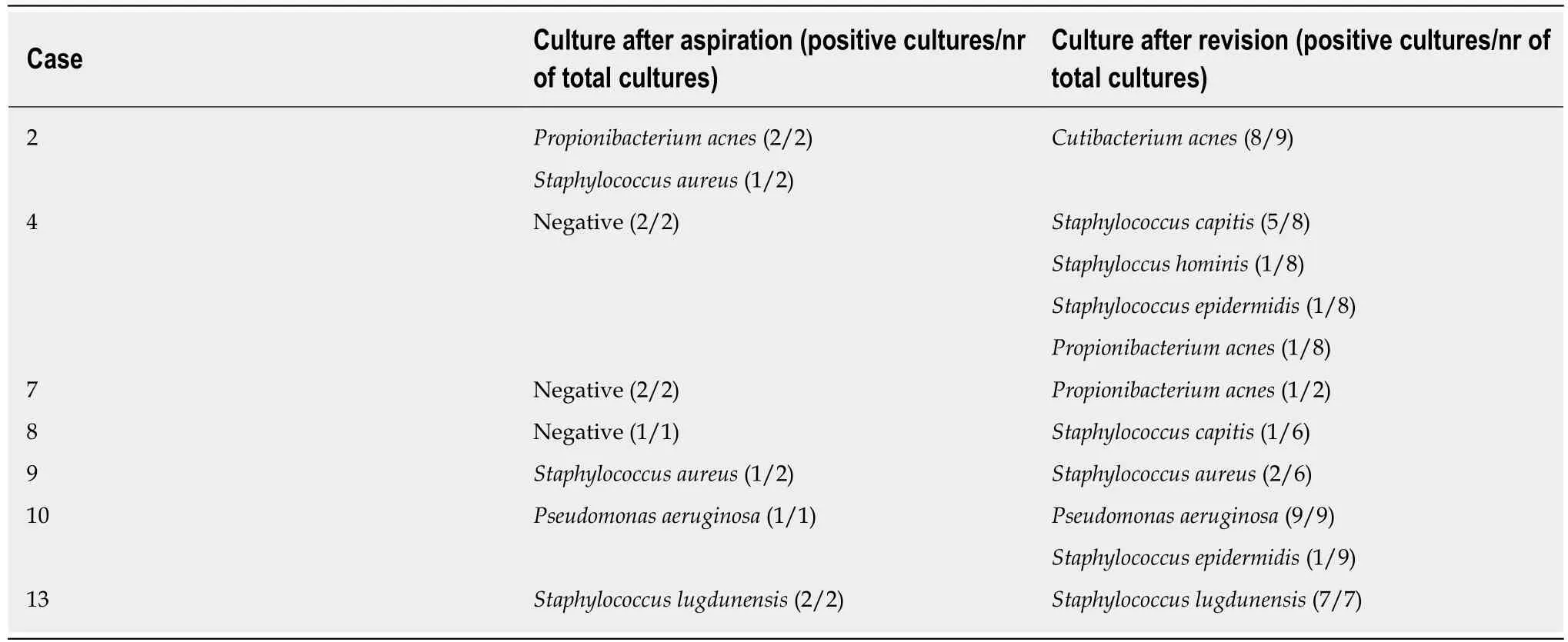
Table 8 All cases of positive cultures in the described cohort
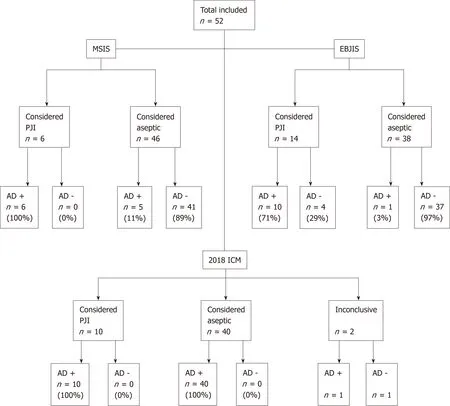
Figure 1 Flowchart of patient selection and prosthetic joint infection diagnosis according to Musculoskeletal Infection Society, European Bone and Joint Infection Society and 2018 International Consensus Meeting criteria.
ARTICLE HIGHLIGHTS
Research background
Periprosthetic joint infection (PJI) is one of the most severe complications after hip arthroplasty.Therefore, it is important to diagnose this problem accurately. Several diagnostic criteria are currently used for PJI diagnosis.
Research motivation
One of the newest additions to the diagnostic options is the determination of alpha-defensin, a protein released by white blood cells in synovial fluid. Two tests are available, the lateral flow test being the fastest (point of care) test. This test of aspirated joint fluid has not yet been extensively studied.
Research objectives
The objective was to identify a cohort of patients after hip arthroplasty in whom the alphadefensin lateral flow (ADLF) test was already performed in the last two years in our hospital,and to assess the accuracy of the ADLF test for this cohort.
Research methods
The database of patients after total hip arthroplasty who underwent aspiration and ADLF testing was checked and data were retrospectively collected and analyzed. All patients underwent sterile aspiration of the hip joint as part of the diagnostic work-up for painful or poor functioning hip arthroplasty, between January 2015 and March 2018. Three recent definitions of PJI for calculation of test accuracy were used. The Musculoskeletal Infection Society (MSIS) definition was used as the standard. European Bone and Joint Infection Society (EBJIS) and International Consensus Meeting (ICM) definitions were also used for comparison.
Research results
A total of 52 patients (52 aspirations) were included in this pilot study. In 11 patients (21%) the ADLF test was positive. According to the MSIS criteria, 6 patients had a PJI. Using these criteria,sensitivity was 100% (CI: 54%-100%), specificity was 89% (CI: 76%-96%), positive predictive value (PPV) was 55% (CI: 34%-73%) and negative predictive value (NPV) was 100%. When adhering to the criteria by the EBJIS, PJI was found in 14 patients and the ADLF test had a sensitivity of 71% (CI: 42%-92%), specificity of 97% (CI: 86%-100%), PPV of 91% (CI: 58%-99%)and NPV of 90% (CI: 80%-96%).
When using the 2018 ICM criteria and classifying inconclusive cases as infected, sensitivity was 91% (62%-100%), specificity 100% (91%-100%). PPV, NPV and accuracy were 100%, 98%(86%-100%) and 98% (90%-100%), respectively.
Research conclusions
The diagnostic accuracy of the ADLF test for hip arthroplasty was high: Sensitivity was 100%,specificity 89%. Using different PJI diagnosis criteria, overall accuracy remained 90% or higher.These results are comparable to prior findings by other authors. Caution should be taken when when interpreting the results of the ADLF test in metallosis cases, as metallosis may cause false positive results.
Research perspectives
This study confirms the good clinical test results for the ADLF test found by others. However,the use of the ADLF test in cases of suspected PJI in hemi-arthroplasty or metal-on-metal has not been studied well, and one should be careful not to rely solely on the ADLF test, especially in those cases.
ACKNOWLEDGEMENTS
Many thanks to Hayko Heres Diddens for his help in editing the manuscript and his continuous support.
猜你喜欢
杂志排行
World Journal of Orthopedics的其它文章
- Patents and intellectual property in orthopaedics and arthroplasty
- Rapid spontaneous resolution of lumbar ganglion cysts: A case report
- Use of three-dimensional printing in preoperative planning in orthopaedic trauma surgery: A systematic review and meta-analysis
- Effect of deep transverse friction massage vs stretching on football players’ performance
- Corrections in alpha angle following two different operative approaches for CAM-type femoral acetabular impingement - Ganz surgical hip dislocation vs anterior mini-open
- National trends in total hip arthroplasty for traumatic hip fractures:An analysis of a nationwide all-payer database