National trends in total hip arthroplasty for traumatic hip fractures:An analysis of a nationwide all-payer database
2020-01-16AnthonyBonielloAlexanderLieberKevinDenehyPriscillaCavanaughYehudaKerbelAndrewStar
Anthony J Boniello, Alexander M Lieber, Kevin Denehy, Priscilla Cavanaugh, Yehuda E Kerbel, Andrew Star
Anthony J Boniello, Priscilla Cavanaugh, Andrew Star, Rothman Orthopaedic Institute, Thomas Jefferson University, Philadelphia, PA 19107, United States
Alexander M Lieber, Drexel University College of Medicine, Philadelphia, PA 19123, United States
Kevin Denehy, Bluegrass Orthopaedics, Lexington, KY 40509, United States
Yehuda E Kerbel, Deparment of Orthopaedics, Hospital of University of Pennsylvania,Philadelphia, PA 19104, United States
Abstract
Key words: Hip fracture; Total hip arthroplasty; Hemiarthroplasty; Cost; Length of stay;National Inpatient Sample
INTRODUCTION
Femoral neck fractures represent a large proportion of orthopedic injuries requiring surgical intervention. It is estimated that by 2050, there will be over 700000 cases annually in North America[1]. Hemiarthroplasty (HA) has become the most common treatment modality for displaced femoral neck fractures[2,3]. Recently, total hip arthroplasty (THA) has gained popularity for treating displaced femoral neck fractures, particularly with active, healthy patients[4]. Over the last 15-20 years, THA as treatment for displaced femoral neck fractures has increased[5].
Independent, ambulatory patients have poor functional results following HA compared to THA, particularly continued hip pain and a higher revision rate[6,7].Several investigators have used large administrative database analyses to track trends in the treatment of femoral neck fractures, with conflicting reports in the arthroplasty and trauma literature. While some studies report no significant change in the utilization of THAvsHA[5,8,9], others report a recent increase in THA usage[10,11].
Our study utilizes the Nationwide Inpatient Sample (NIS) database from 2005-2014 to see trends in THAvsHA for femoral neck fractures. Our goal was not only to calculate the general trend over the past 10 years, but also determine what other factors influence treatment decisions.
MATERIALS AND METHODS
NIS data from 2005 to 2014 was used. The NIS is a large all-payer database of datat from the United States developed as part of the Healthcare Cost and Utilization Project by the Agency for Healthcare Research and Quality. Each NIS file comprises de-identified information from approximately eight million hospital records from about 1000 hospitals in 46 states, representing an approximate 20% sample of hospitals[12]. National estimates may be calculated from the data using available weighting factors. For each patient record, 100 clinical and nonclinical data elements are available including admission and discharge status, patient demographics,insurance type, hospital charges, length of stay (LOS), and hospital type in addition to diagnosis and procedural codes in International Classification of Disease-9thRevision-Clinical Modification (ICD-9-CM)[13]. Recorded patient characteristics include gender,race, comorbidities and age. Given that the NIS database is sufficiently deidentified,this study was not subject to institutional review board review.
For our study, we identified record of patients who had transcervical femoral neck fractures (ICD-9-CM 820.0). We used ICD-9 codes to exclusively look at patients treated with THA (81.51) and HA (81.52). We excluded pathologic fractures due to oncologic etiology. Recorded Hospital characteristics were ownership (public, not-forprofit, or private investor-owned), teaching status, Urban or rural Location, and region (Northeast, Midwest, South, or West). We analyzed patient insurance type(Medicare, Medicaid, private, or self-pay), and charges during the stay.
Statistical analysis
Statistical analysis was performed using SPSS version 23 (IBM Corporation, Armonk,New York), specifically SPSS complex samples procedure to model the strata,clustering (hospitals), and weighting of the NIS sample design. Chi-square tests were utilized for categorical variables andttests were employed for continuous variables.Categorical variables are presented as percentages and continuous variables as means.Yearly trends were analyzed using linear regression modeling.Pvalues of less than 0.05 were interpreted as statistically significant.
RESULTS
Of the total 502060 patients who underwent arthroplasty for a femoral neck fracture,51568 (10.3%) were THA. Between 2005 and 2014, the percentage of femoral neck fractures treated with THA rose from 8.3% to 13.7% (Figure 1). The HA group was generally less healthy, with higher rates of congestive heart failure (16.8%vs11.0%,P< 0.001), chronic lung disease (21.6%vs20.3%,P= 0.004), diabetes (17.0%vs15.3%,P< 0.001), hypertension (69.0%vs62.2%,P< 0.001), and renal failure (13.4%vs9.6%,P< 0.001). (Table 1) Hemiarthroplasty patients were on average older (81.1 yearsvs74.5 years,P< 0.001) (Figure 2). Private insurance accounted for a higher percentage of THA than HA (17.3%vs7.4%,P< 0.001) (Table 2). THA has increased most in urban teaching hospitals (7.9% to 14.7%) relative to urban non-teaching (mean 11.1%vs10.0%, OR = 1.05,P= 0.002) over the ten-year study period (Figure 3). The mean LOS was statistically different but clinically similar for HA (5.6 dvs5.5 d,P< 0.001). While the mean LOS decreased over time for both groups, the rate of decline was significantly greater for the THA cases (decrease of 1.1vs0.7 d,P< 0.0001) (Figure 4).The mean charges (adjusted to 2014 dollars) were less for HA ($49866vs$59826,P<0.0001), however they increased steadily for both groups (Figure 5). Overall, HA had a higher in-hospital mortality rate (2.3%vs1.4%,P< 0.001), however, after adjusting for age and comorbidities HA was not an independent risk factor for in-hospital mortality (OR = 0.998,P= 0.94). Multivariate analysis adjusting for demographics,comorbidities and age found private insurance (vsmedicare) to be an independent predictor of being treated with THA (OR = 1.46,P< 0.0001).
DISCUSSION
In recent years, the incidence of femoral neck fractures has continued to decline,however the associated economic burden remains enormous[14-17]. These fractures can be devastating to the patient and to the health care system because of the associated morbidity, mortality and cost[18]. Displaced femoral neck fractures in the elderly are commonly treated with HA. However, recent studies have demonstrated that THA may have superior post-operative function, pain relief and lower re-operation rates when compared to HA in the setting of displaced femoral neck fractures[6,7,19]. Despite these benefits, concerns for THA include longer operative time, increased surgical complexity, risk of postoperative dislocation, and higher initial cost[18]. THA has become the preferred treatment for the healthier, higher demand elderly patient,meanwhile, HA is reserved for low-demand patients with significant comorbidities.Interestingly, despite increasing evidence in support of THA for geriatric femoral neck fractures, only recently has the literature demonstrated an increasing use of THA over HA[6,7].
The present study found a statistically significant increase in the percentage of femoral neck fractures treated with THA in the United States between 2005 and 2014.These findings support recent registry-based studies from the United States[19,20],Europe and Asia[11,19,21]. We found that patients treated with HA had more comorbidities and were on average older than patients that underwent THA. The greater complexity and longer operative time associated with THA are some of the main reasons why HA is often preferred for sicker patients that may not be able to tolerate THA. Additionally, dislocation risk has been noted as a significant factor influencing the selection of HAvsTHA in the elderly. Bekeromet al[22]conducted a randomized control trial comparing patients aged 70 years and older that underwent HAvsTHA for the treatment of femoral neck fractures and found a higher number of early and late dislocations in the THA group[22]. Overall, with patients above 70 years,the decision to treat with HA is multifactorial and includes severity of comorbidities,surgeon experience and pre-operative level of activity. Unfortunately, these clinical variables cannot be studied using current national databases, thus warranting further investigation.
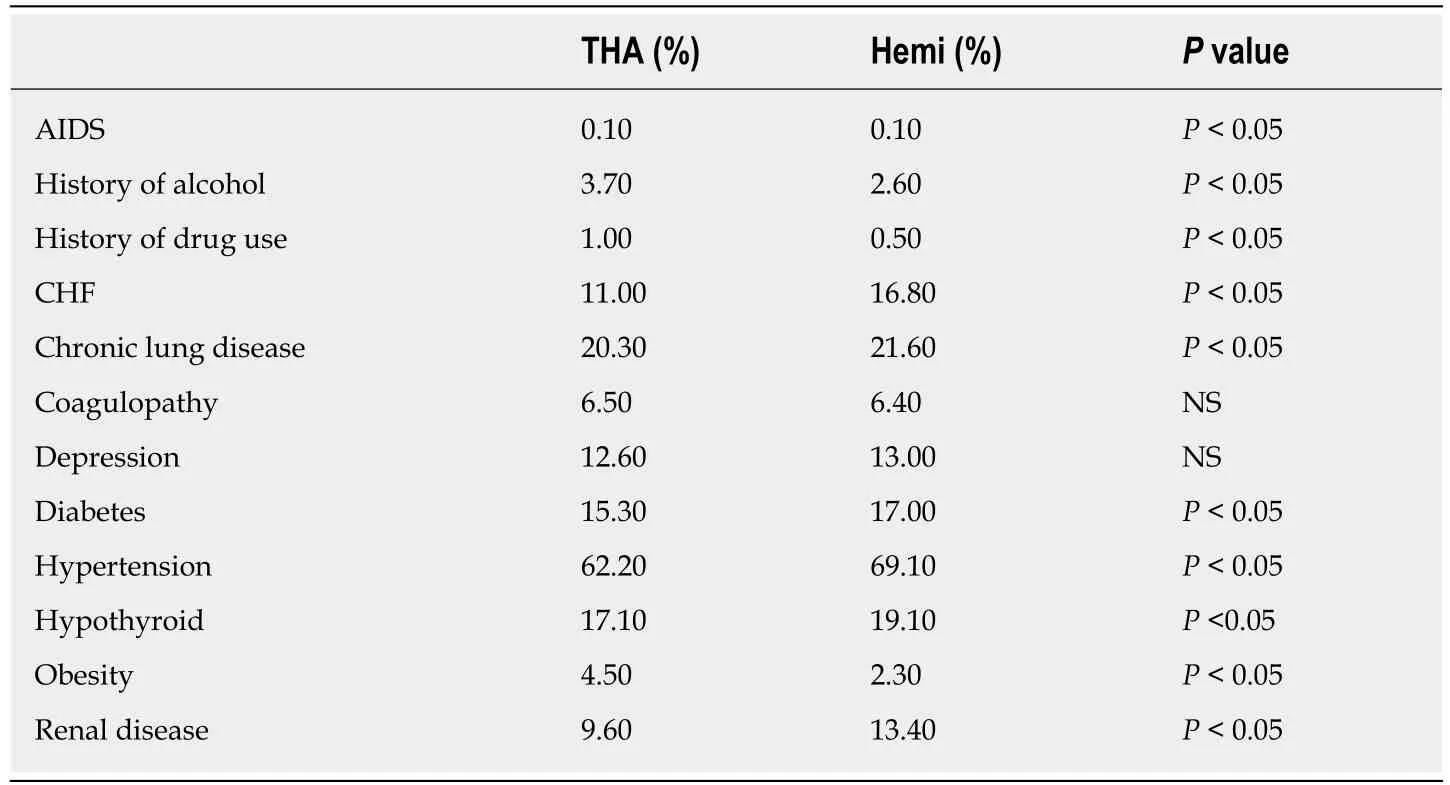
Table 1 Comparison of comorbidities between patients who underwent hemiarthroplasty and total hip arthroplasty for a femoral neck fracture between 2005 and 2014
Interestingly, patients with private insurance were more likely to undergo THA than patients with Medicare even after adjusting for differences in patient demographics and comorbidities. THA may yield better functional results and lower reoperation rates compared to HA[6,7,19]. However, given that THA incurs greater hospital costs than HA, the reasons for disparities between femoral neck fracture treatment options should be carefully examined. Notably, Schaireret al[23]found that patients with private insurance or worker’s compensation were more likely to undergo surgical management of isolated meniscal tears compared to payments with public or no insurance. However, these results contrast the findings of McGlastonet al[24]who found that rates of surgery of the upper extremity did not differ based on privatevspublic insurance. Further research should more clearly define the impact if any of patient insurance type on treatment choice for orthopedic procedures.
With regards to hospital type, the use of THA for femoral neck fractures significantly increased in urban teaching and non-teaching hospitals. The sharpest increase was noted in urban teaching hospitals; meanwhile, rural hospitals showed a more modest increase in THA utilization during the study period. These results may reflect both a higher number of new surgeons willing to change traditional management of elderly femoral neck fractures and an increased exposure to recent literature favoring THA in academic settings. It is plausible that surgeons in academic settings are more familiar with the most current orthopedic research. However, this is not likely to fully explain differences between teaching and non-teaching centers, so further research is warranted. Notably, previous research has indicated that patients undergoing orthopedic procedures at teaching hospitals experience higher hospital costs, rates of complications, mortality, and longer LOS compared to non-teaching hospitals[25,26]. However, Silberet al[27]found that undergoing orthopedic surgery at a teaching hospital was protective for preventing in-hospital mortality.
Length of hospital stay was shorter for the traumatic THA patients compared to HA patients. However, this difference was very small and may not be clinically significant. These findings may be consistent with a study of 82951 patients with femoral neck fractures treated with either THA or HA that found no significant difference in LOS between the two groups[28].
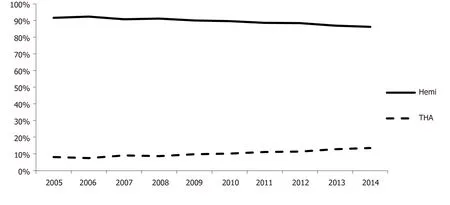
Figure 1 Percentage of hemiarthroplasty and total hip arthroplasty performed for femoral neck fractures between 2005 and 2014.
There is a paucity of literature evaluating the inpatient cost associated with treatment of displaced femoral neck fractures in the United States. Our study is unique in that it uses a large nationally representative database to compare total inpatient charges of femoral neck fractures in patients treated with either THAvsHA over a ten-year period. We found that both THA and HA in the setting of femoral neck fractures have been associated with gradually increasing charges. This is an interesting finding, as there has been a decrease in cost for elective THA noted during the same time period. The rise in the charges for traumatic THA may be secondary to an increase in implant costs and most importantly the inability to preoperatively prepare patients prior to surgery as compared to elective THA patients.Unfortunately, the database does not provide information regarding payments, so we are unable to make statements regarding the actual costs of care. Driving factors that explain the differences in traumatic THAvselective THA costs warrants further investigation.
In-hospital mortality was not significantly higher in patients treated with a HA compared to THA when adjusted for comorbidities. These findings agree with a review article by Guyen[29]that found mortality rates were similar when comparing THA with HA for the treatment of femoral neck fractures. Instead of type of implant,patient comorbidities likely play a much more significant role in mortality risk. The significance of comorbidities in this femoral neck fracture population was highlighted by Macaulayet al[30]that found a 2.4 fold increase in risk of death for each additional comorbid condition. Furthermore, although the incidence of both HA and THA have steadily increased, mortality has not. This may suggest surgeons are successfully risk stratifying these patients, with THA being appropriately reserved for the healthier,lower risk patients.
There were limitations to our study that are inherent to database studies. The NIS is a database that relies on codes intended for billing; therefore, we were unable to obtain data on the severity of comorbidities, prior functional status or extent of fracture displacement. This data as these factors likely play a significant role in a surgeon’s surgical preference independent of age or sex so the findings of our study should be interpreted with caution. Furthermore, the NIS database evaluates a single hospital admission during the index THA or HA surgeries so long-term follow up for complications, mortality, or conversion of THA to HA was not captured.Additionally, the NIS does not allow us to examine solely patients who underwent THA with the minimally invasive approach. Therefore, our patient population likely represents a more heterogeneous group.
Despite these limitations, our study indicated that THA is increasing being utilized in the treatment of displaced femoral neck fractures in the United States. We found that traumatic THA is increasing most notably in urban hospitals, is increasing in charges, and is associated with a shorter LOS. Hemiarthroplasty is associated with older patients with significant comorbidities.

Table 2 Comparison of demographics between patients who underwent hemiarthroplasty and total hip arthroplasty for a femoral neck fracture between 2005 and 2014
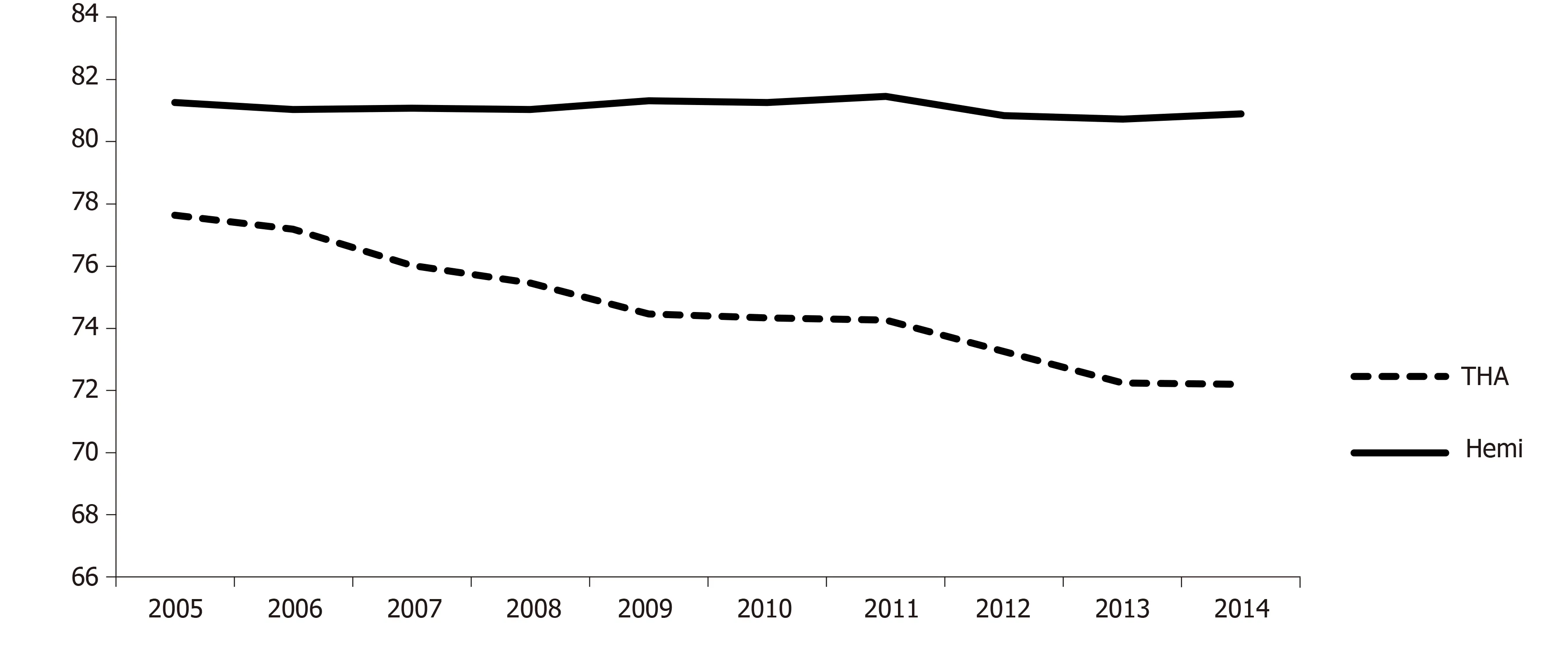
Figure 2 Age in years of hemiarthroplasty and total hip arthroplasty patients between 2005 and 2014.
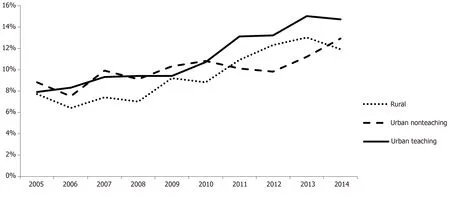
Figure 3 Percentage of total hip arthroplasty procedures performed for femoral neck fractures by hospital type (urban teaching hospitals, urban nonteaching, rural) between 2005 and 2014.

Figure 4 Length of stay in days of hemiarthroplasty and total hip arthroplasty patients between 2005 and 2014.
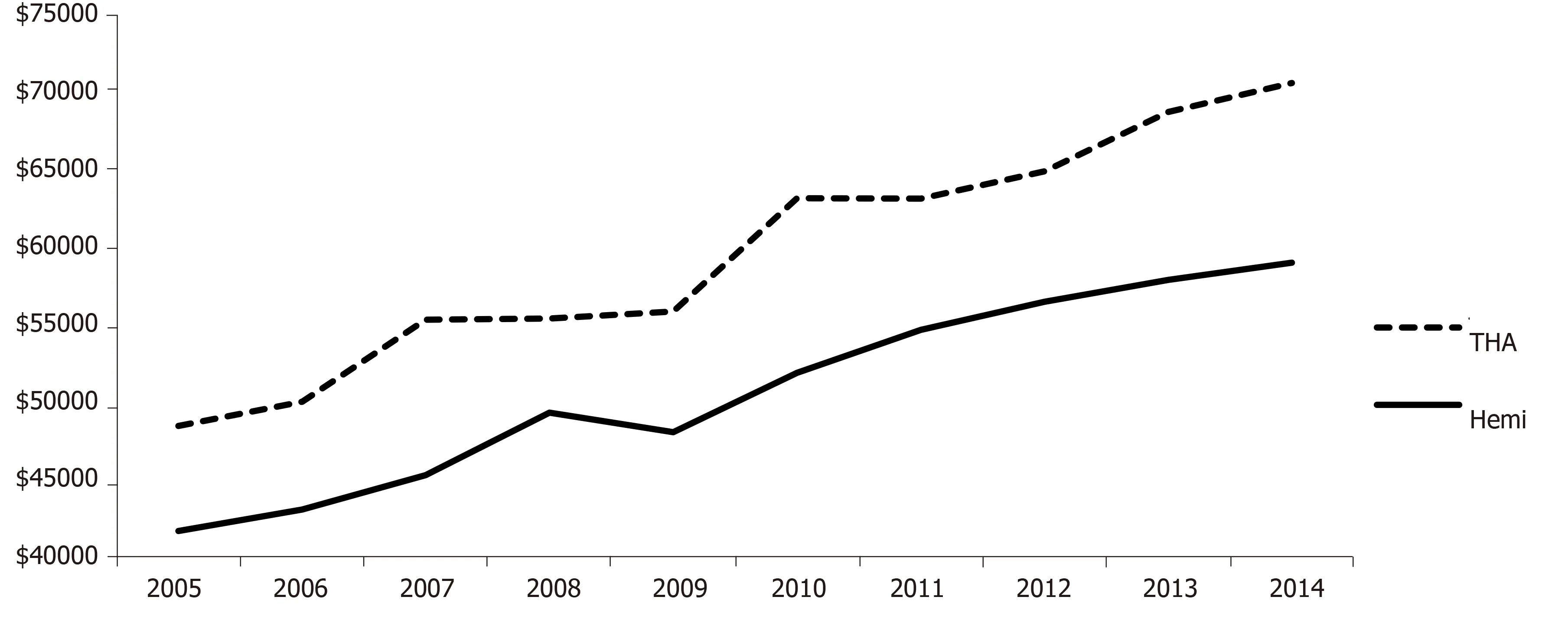
Figure 5 Mean charges (adjusted to 2014 United States dollars) for hemiarthroplasty and total hip arthroplasty patients between 2005 and 2014.
ARTICLE HIGHLIGHTS
Research background
Femoral neck fractures despite decreasing steadily in incidence still represent a tremendous economic burden world-wide. Total hip arthroplasty (THA) is an increasingly utilized treatment for displaced femoral neck fractures especially for younger, healthier, ambulatory patients.Notably, multiple studies have demonstrated that THA has superior functional outcomes and results in less pain postoperative compared to hemiarthroplasty (HA).
Research motivation
The motivation for this research study was to further characterize factors associated with patients undergoing THA or HA following displaced femoral neck fracture. This was done in the hopes of better understanding which patients are more likely to undergo THA and what factors may predict adverse in this patient population.
Research objectives
The research objectives in this study was to assess the incidence of patients undergoing THA and HA after displaced femoral neck fracture in the United States. Furthermore, we explored whether hospital length of stay (LOS), discharge disposition, and cost differed between patients undergoing THA or HA.
Research methods
This was a retrospective study which utilized the Nationwide Inpatient Sample between 2010 and 2014. We identified patients undergoing THA and HA for femoral neck fractures using Ninth Edition diagnosis and procedure codes. Chi-square tests were used to compare categorical variables andttests for continuous variables. Yearly trends were analyzed using linear regression modeling.Pvalues less than 0.05 were considered statistically significant.
Research results
Of the total 502060 patients who were treated for femoral neck fracture in our study, 51568(10.3%) underwent THA and the incidence of THA rose from 8.3% to 13.7%. Private insurance accounted for a higher percentage of THA than hemiarthroplasty. THA increased most in urban teaching hospitals relative to urban non-teaching hospitals. Mean LOS was longer for HA. The mean charges were less for HA, however charges decreased steadily for both groups. HA had a higher mortality rate, however, after adjusting for age and comorbidities HA was not an independent risk factor for mortality.
Research conclusions
Our study was consistent with previous research that the number of patients undergoing THA for femoral neck fractures has increased. Furthermore, we found that THA was more common in urban hospitals and in patients with private insurance. Both of these trends have been reported prior, however further research should better examine the etiology between these associations.We found no difference in mortality between patients undergoing HA and THA reflecting that mortality is more dependent on patient comorbidies than surgical technique.
Research perspectives
Future research most more closely examine the relationship between surgical choice of femoral neck fracture fixation and insurance type especially since we found increased cost for patients undergoing THA. Prospective studies are needed to effectively examine this research question.Additionally, randomized controlled studies are needed to better develop treatment algorithms to guide orthopedic surgeons on which patients may benefit most from THA compared to HA.
杂志排行
World Journal of Orthopedics的其它文章
- Patents and intellectual property in orthopaedics and arthroplasty
- Rapid spontaneous resolution of lumbar ganglion cysts: A case report
- Use of three-dimensional printing in preoperative planning in orthopaedic trauma surgery: A systematic review and meta-analysis
- Effect of deep transverse friction massage vs stretching on football players’ performance
- Good accuracy of the alpha-defensin lateral flow test for hip periprosthetic joint infection: A pilot study in a retrospective cohort of 52 patients
- Corrections in alpha angle following two different operative approaches for CAM-type femoral acetabular impingement - Ganz surgical hip dislocation vs anterior mini-open