Efficacy of hybrid minimally invasive esophagectomy vs open esophagectomy for esophageal cancer:A meta-analysis
2019-12-14JiaoYangLingChenKeGeJianLeYang
Jiao Yang,Ling Chen,Ke Ge,Jian-Le Yang
Jiao Yang,Ling Chen,Ke Ge,Jian-Le Yang,Department of Infectious Diseases,Zhejiang Hospital,12 Lingyin Road,Hangzhou 310013,Zhejiang Province,China
Abstract
Key words: Hybrid minimally invasive esophagectomy; Open esophagectomy;Esophageal cancer
INTRODUCTION
Esophageal cancer is the eighth most common cancer worldwide,with nearly 17000 newly diagnosed cases and 15910 deaths recorded annually in the United States alone[1].Despite early diagnosis and advanced therapeutic modalities,including surgical resection,radiotherapy,and chemotherapy,the 5-year overall survival rate is a dismal 15% to 20%[2].Esophageal resection remains the major curative and palliative option for dysphagia.For middle- and lower-third esophageal cancer,the abdominal and right thoracic approach is selected due to good loco-regional control.However,post-esophagectomy morbidity and mortality rates are 30%-50% and 2%-10%,respectively[3],mainly due to endocrinal and metabolic changes.The most frequent complications of esophagectomy are the major pulmonary complications (MPPCs),such as pneumonia and acute respiratory distress syndrome.Almost 50% of the postoperative deaths are attributed to MPPCs,which are indicative of poor prognosis.
Cuschieriet al[4]introduced endoscopic esophagectomy in 1992,which was followed by the development of minimally invasive esophagectomy (MIE),which uses a thoraco-abdominal approach and a combination of laparoscopy,thoracoscopy,and transhiatal laparoscopy.MIE can reduce surgical stress response,decrease blood loss,shorten hospital stay,and lower the incidence of complications[5-7].However,only a few randomized controlled trials (RCTs) and low-quality meta-analysis have evaluated its clinical outcomes,in terms of tumor and lymph node clearance,and the safety profile.Hybrid MIE (HMIE) is performed using an Ivor-Lewis procedure,viaa thoracoscopic-laparotomy and laparoscopic gastric mobilization-thoracotomy,for tumors of the mid-lower esophagus.A three stage McKeown’s procedure,with an additional left cervical incision,has been developed for the upper third of the esophagus.Open esophagectomy is performed by starting with an open right thoracotomy to mobilize the esophagus,followed by an open laparotomy to mobilize and pull the stomach to the neck for anastomosis.Therefore,HMIE may improve perioperative outcomes.The aim of this study was to compare the efficacy of open esophagectomy (OE) and HMIE in esophageal cancer patients.
MATERIALS AND METHODS
Literature search
PubMed,EMBASE,and Cochrane Library database s were searched for studies published till February 1,2019 using the followingKey words:Open esophagectomy,Hybrid minimally invasive esophagectomy,minimally invasive esophagectomy,and esophageal cancer.In addition,the reference lists of the eligible studies were manually searched to include additional studies.
Study selection
The inclusion criteria for the studies were as follows:(1) RCTs and non-RCTs; (2)Including patients with esophageal cancer; (3) Comparing the outcomes of OE and HMIE; and (4) Evaluating intraoperative outcomes and postoperative outcomes of both modalities.The exclusion criteria were:(1) In languages other than English; (2)Lacking comparison of OE and HMIE; and (3) Case reports and duplicate publications.
Data extraction
Two authors (Jiao Yang and Ling Chen) evaluated the titles,abstracts,and the reference lists of the publications,and independently extracted the data of intraoperative outcomes (lymph node yield,blood loss,and operative time) and postoperative outcomes (the rates of total complications,pulmonary complications,cardiac complications,and anastomotic leak,the duration of intensive care unit (ICU)stay and hospital stay,and total 30-d and 90-d mortality).Any disagreements were resolved by discussion with a third investigator (Ke Ge).For case-control studies,the Newcastle-Ottawa Quality Assessment Scale was used to assess the quality of the eligible studies,and those with a score ≥ 6 were included.Quality of RCTs was evaluated using the risk bias of Cochrane Collaboration tool.
Statistical analysis
All analyses were performed with the RveMan5.3 tool (Nordic Cochrane Centre,Cochrane Collaboration).Study heterogeneity was assessed usingχ2and I2tests.A fixed-effects model was used whenI2was < 50% orP> 0.1,indicating no significant heterogeneity amongst the studies,and a random-effects model was used when I2was> 50% orP< 0.1.Odds ratio (OR),standard mean difference (SMD),and 95%confidence interval (CI) were used as effect measurements,andP< 0.05 was considered statistically significant.Publication bias was evaluated by funnel plots and sensitivity analysis was applied to assess the stability of results.
RESULTS
Characteristics of selected studies
A total of 17 studies,including 2 RCTs[8,9]and 15 case-control studies[10-24],were eligible for the meta-analysis.The studies included 2397 esophageal carcinoma patients,of which 1170 received HMIE and 1227 underwent OE.The detailed search strategy is shown in Figure1.The baseline characteristics and quality of the included studies are summarized in Table1,Table2,Table3,and Table4.
Intraoperative outcomes
Lymph node yield:Nine studies reported the lymph node yield,with no significant difference between the HMIE with different approaches and OE groups (SMD = 0.11;95%CI:-0.08,0.30;P= 0.26; Table5).Since significant heterogeneity (I2= 65% andP=0.004) was observed amongst the studies,a random-effects model was utilized.Then,subgroup analysis was used to compare HMIE with laparoscopy and thoracotomy and OE.Patients with laparoscopy and thoracotomy (HMIE) presented no more lymph node yield compared to those with OE (SMD = 0.19; 95%CI:-0.00,0.37;P=0.05; Table5).
Blood loss:Six trials evaluated blood loss,which was also analyzed using the random-effects model due to significant heterogeneity (I2= 58% andP= 0.04).HMIE with different strategies resulted in significantly lower blood loss compared to OE(SMD = -0.43; 95%CI:-0.66,-0.20;P= 0.0002; Table5).In the subgroup analysis,HMIE using laparoscopy and thoracotomy showed priority to OE in decreasing the blood loss (SMD = -0.51; 95%CI:-0.74,-0.27;P< 0.0001; Table5)
Operative time:Twelve studies involving 1630 patients recorded the operative time,and displayed significant heterogeneity in the outcome (I2= 92% andP< 0.00001).However,HMIE with different approaches or HMIE with laparoscopy and thoracotomy did not significantly decrease the duration of operation (SMD = 0.24;95%CI:-0.14,0.61;P= 0.22 and SMD = 0.10; 95%CI:-0.33,0.52;P= 0.65,respectively;Table5).
Postoperative outcomes
Complications:Fourteen trials provided data of the total complications,and showed no significant differences between the HMIE with different approaches group and OE group (OR = 0.68; 95%CI:0.46,0.99;P= 0.05; Table6).However,patients with HMIE using laparoscopy and thoracotomy presented less total complications than those with OE (OR = 0.62; 95%CI:0.41,0.94;P= 0.02; Table6).Total HMIE and HMIE with laparoscopy and thoracotomy were associated with less pulmonary complications than OE (OR = 0.72; 95%CI:0.57,0.90;P= 0.004 and OR = 0.69; 95%CI:0.53,0.90;P=0.005,respectively; Table6),whereas the incidences of cardiac complications (OR =0.91; 95%CI:0.62,1.34;P= 0.64 and OR = 0.97; 95%CI:0.65,1.43;P= 0.86,respectively;Table6) and anastomotic leak (OR = 0.95; 95%CI:0.67,1.35;P= 0.78 and OR = 0.99;95%CI:0.67,1.46;P= 0.96,respectively; Table6) were similar.
Hospital and ICU stays:Thirteen studies reported duration of hospital stay with significant heterogeneity (I2= 57% andP= 0.006),and total HMIE was not associated with significantly reduced duration of hospital stay (SMD = -0.13; 95%CI:-0.28,0.01;P= 0.08; Table6).However,shorter hospital stay showed in patients with HMIE using laparoscopy and thoracotomy than those with OE (SMD = -0.37; 95%CI:-0.64,-0.09;P= 0.009; Table6).
In addition,the duration of ICU stay was similar in total HMIE or HMIE with laparoscopy and thoracotomy group and OE group (SMD = -0.01; 95%CI:-0.21,0.19;P= 0.93 and SMD = -0.05; 95%CI:-0.37,0.27;P= 0.76,respectively; Table6).
Mortality:No significant heterogeneity was detected amongst the studies reporting the total,30-d,and 90-d mortality rates,which were similar in total HMIE or HMIE with laparoscopy and thoracotomy group and OE group (total mortality:OR = 0.70,95%CI:0.47,1.06,P= 0.09 and OR = 0.65,95%CI:0.4,1.07,P= 0.09,respectively; 30-d mortality:OR = 1.00,95%CI:0.45,2.23,P= 0.99 and OR = 1.10,95%CI:0.47,2.59,P=0.82,respectively; 90-d mortality:OR = 0.80,95%CI:0.43,1.48,P= 0.47 and OR = 0.80,95%CI:0.43,1.48,P= 0.47,respectively; Table6).
Publication bias:Publication bias was evaluated for the outcomes of pulmonary complications,cardiac complications,anastomotic leak,and total mortality and none was detected (Figure2).
Sensitivity analysis
We removed any single trial,chose different effect models,and conducted subgroup analysis,and the outcomes presented no significant changes,suggesting that the results were stable.
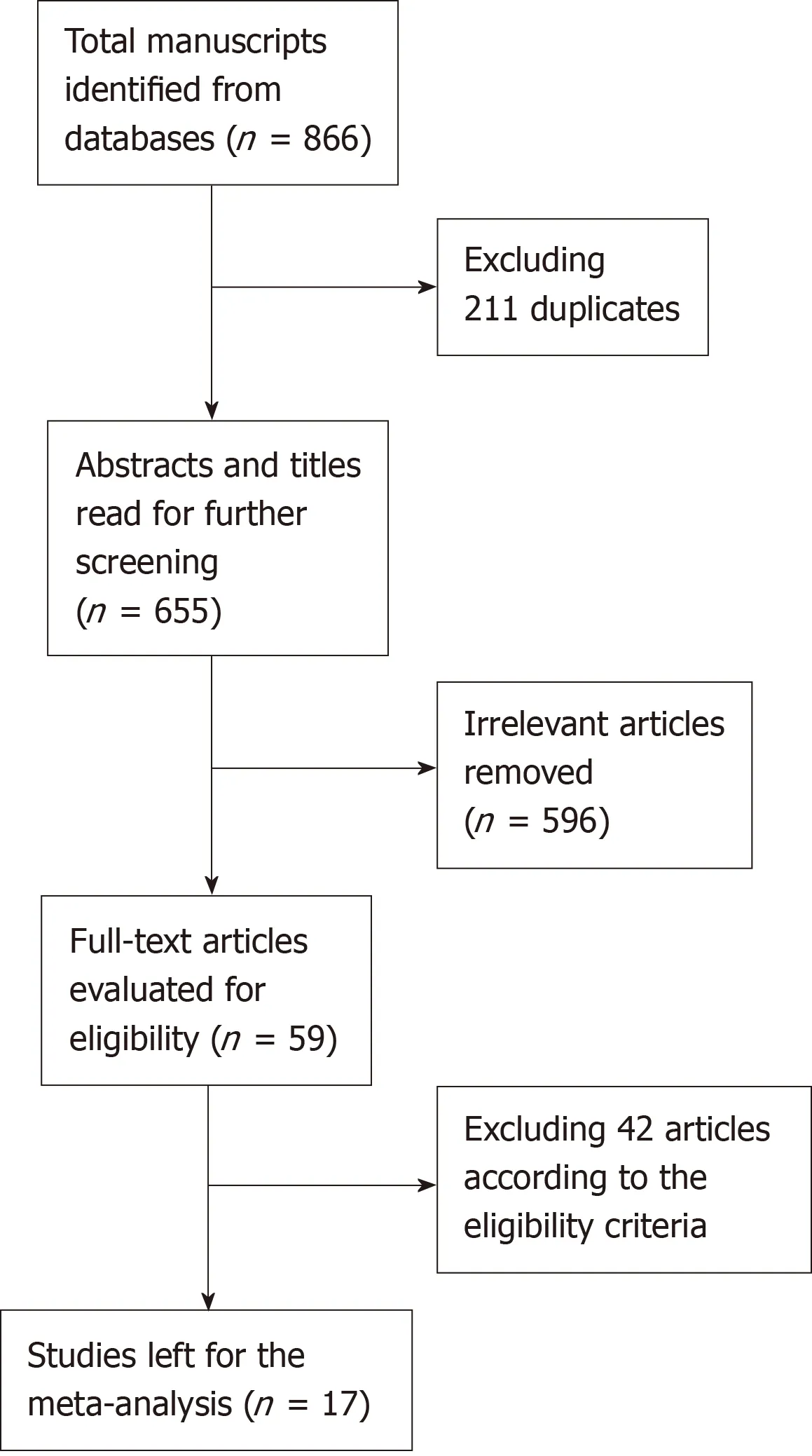
Figure1 Flow diagram showing the selection process of relevant literature.
DISCUSSION
Esophageal cancer is the sixth leading cause of cancer-related deaths worldwide.Surgical resection is the first line of treatment,and includes OE,total MIE,and HMIE.Depending on the surgeon and the hospital,the choice and sequence of surgical approaches differ significantly (transthoracicvstranshiatal,intrathoracicvscervical anastomosis,and the degree of lymphadenectomy).OE is associated with a significantly higher risk of surgical trauma,as well as higher morbidity and mortality compared to other surgeries[25].Sunpaweravonget al[25]conducted a meta-analysis to compare the efficacy of OE and MIE,and found that MIE resulted in fewer perioperative complications and less mortality.In addition,patients with MIE had better quality of life scores compared to those with OE in the global health,pain,and physical activity domains[26].Therefore,total MIE would be the ideal choice.But the technical difficulties,the long learning curve,and low reproducibility of the anastomosis limit its use.HMIE has a shorter learning curve while sharing the advantages of MIE.The transition from OE to HMIE may be acceptable.The above information of MIE does not distinguish between the total MIE and HMIE approaches,so whether HMIE is prior to OE is still controversial.In this metaanalysis,we first compared the intraoperative and postoperative outcomes of HMIE and OE in patients with esophageal cancer.
Many studies show that radical lymph node resection and greater extent of lymphadenectomy are closely associated with higher survival rates[27-30].In this study,there was no significant difference in terms of the number of harvested lymph nodes between total HMIE and OE groups,which is consistent with a previous RCT[8].But there was a trend for patients with HMIE using laparoscopy and thoracotomy with a high rate of lymphadenectomy.Some studies once reported a higher or lower number of lymph nodes harvested in MIE group[31,32].Those discrepancies may be explained by the inconsistency of Current Procedure Terminology codes reported by the operating surgeons.
Smitherset al[12]reported that patients who underwent HMIE had less blood loss than those undergoing OE,while Yanasootet al[24]showed no significant difference.In our meta-analysis also,the total HMIE group and the HMIE with laparoscopy and thoracotomy group had less blood loss,which could be attributed to the relatively minimal trauma in HMIE.
Studies also report a longer operative duration of MIE compared to OE[33-35],whichcan result in atelectasis and pneumonia.In our meta-analysis,the operative time was similar for both surgeries.
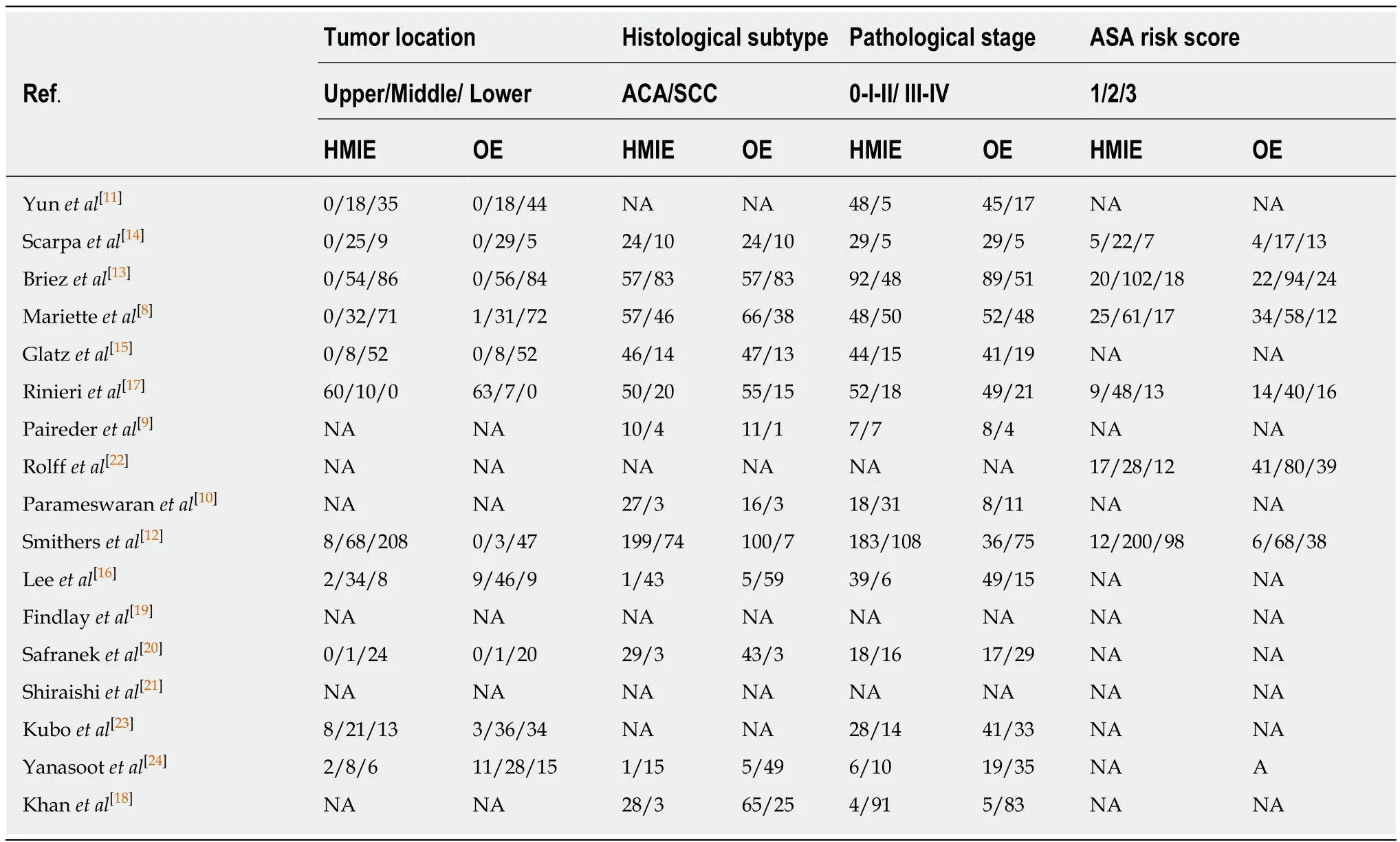
Table2 Baseline characteristics
Postoperative complications,especially pulmonary complications,significantly influence the survival of esophageal cancer patients.The incidences of total complications in patients with total HMIE and OE were 50.2% and 60.1%,respectively,although the lower occurrence after HMIE was not statistically significant.In the subgroup analysis,HMIE with laparoscopy and thoracotomy could largely lower the incidence of total complications than OE (46.55%vs57.74%).The TIME trial showed that MIE resulted in a 70% lower incidence of pneumonia at 2 weeks post-surgery compared to OE[36],which is consistent with our slightly higher incidence of pulmonary complications in OE compared to total HMIE or HMIE with laparoscopy and thoracotomy (25.37%vs32.08% or 24.59%vs31.23%).In contrast,the incidence of cardiac complications and anastomotic leak was not affected by the type of surgery.
Less pulmonary complications in the total HMIE group did not translate into a significant reduction in the duration of ICU and hospital stay.But HMIE with laparoscopy and thoracotomy presented a more reduction in the duration of hospital stay on the basis of its lower total complications and pulmonary complications.
Some studies indicate that the prolonged survival associated with HMIE is due to the lower incidence of postoperative complications[37-39].In our meta-analysis,the overall,30-d,and 90-d mortality rates in the total HMIE group were 4.16%,2.52%,and 4.00%,respectivelyvs6.02%,2.40%,and 4.70% in the OE group,indicating a lack of short-term survival benefit with total HMIE.Patients with HMIE using laparoscopy and thoracotomy presented no priority in short-term survival compared to those with OE.Wanget alreported that 6-year overall survival and disease-free survival were 44.7% and 46.1%,respectively,for MIE,indicating that MIE is safe[40].A score-matched study showed that the 2-year overall survival rates based on same pathologic stage were similar between MIE and OE[41].But further studies are still needed to clarify the long-term survival outcomes.
Our study has several limitations that need to be addressed.First,only two out of the 17 studies were RCTs and the remaining were case-control studies which might have influenced the reliability of the results,although they were consistent with that of one eligible RCT.Second,the studies had variable follow-up duration,neoadjuvant chemoradiotherapy,operating surgeons,pathological stages,histological types and

Table3 Quality assessment of the eligible studies:Newcastle-Ottawa Scale for case control studies
location of the tumor,and baseline characteristics of the recruited population.Third,the meta-analysis did not compare the long-term oncological outcomes between HMIE and OE.Last but not the least,we made subgroup analysis between HMIE with laparoscopy and thoracotomy and OE group.But the information associated with HMIE using thoracoscopic-laparotomy approach is little and ambiguous.Therefore,the real impact of laparoscopy compared to thoracoscopy is unclear,and data that can confirm which part of esophagectomy would play an important role in MIE is lacking.
Taken together,HMIE,especially HMIE with laparoscopy and thoracotomy,has the advantages of reduced blood loss and lower incidence of pulmonary complications compared to OE for patients with esophageal cancer.However,there is no significant difference in overall survival in the two groups.These findings should be explained with caution because our study doesn’t provide the data associated with cancer-specific survival and recurrence.
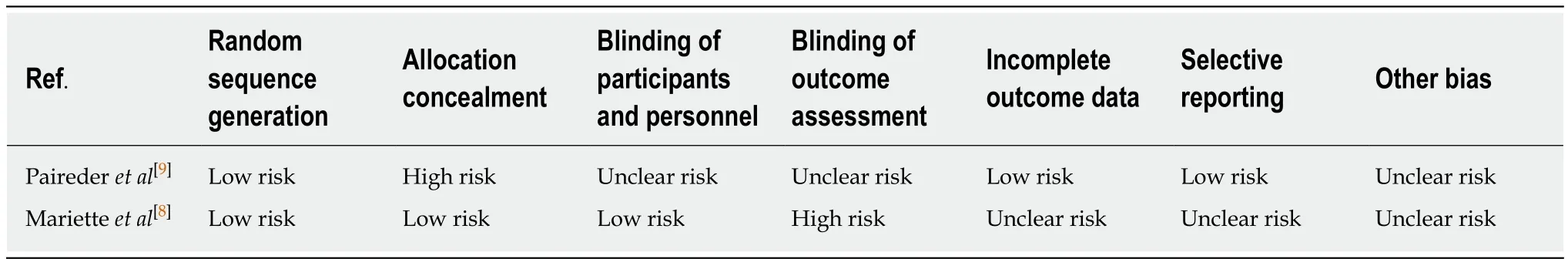
Table4 Quality assessment of the eligible studies:Risk bias of Cochrane Collaboration tool for randomized controlled trials
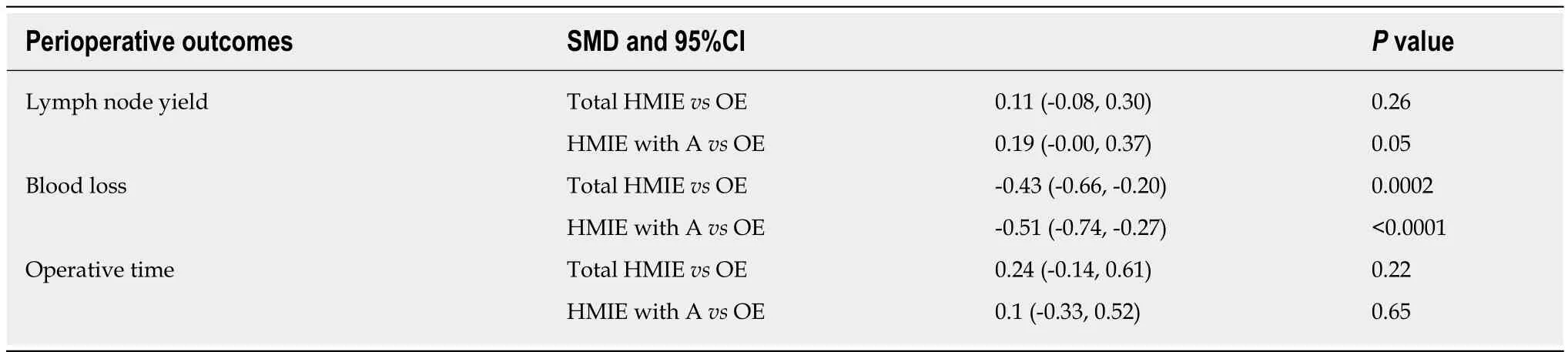
Table5 Comparison of perioperative outcomes between hybrid minimally invasive esophagectomy and open esophagectomy groups
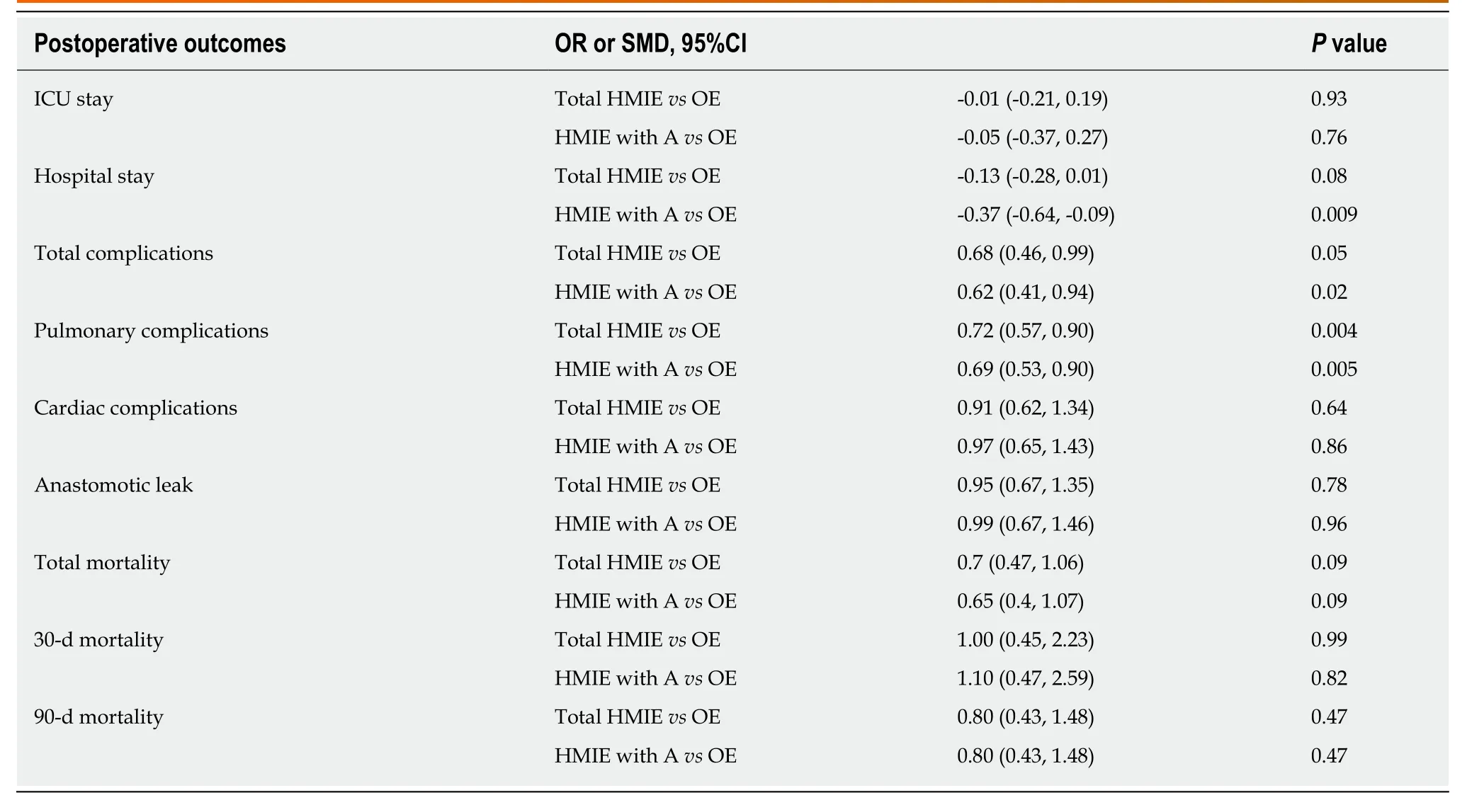
Table6 Postoperative outcomes between hybrid minimally invasive esophagectomy group and open esophagectomy groups
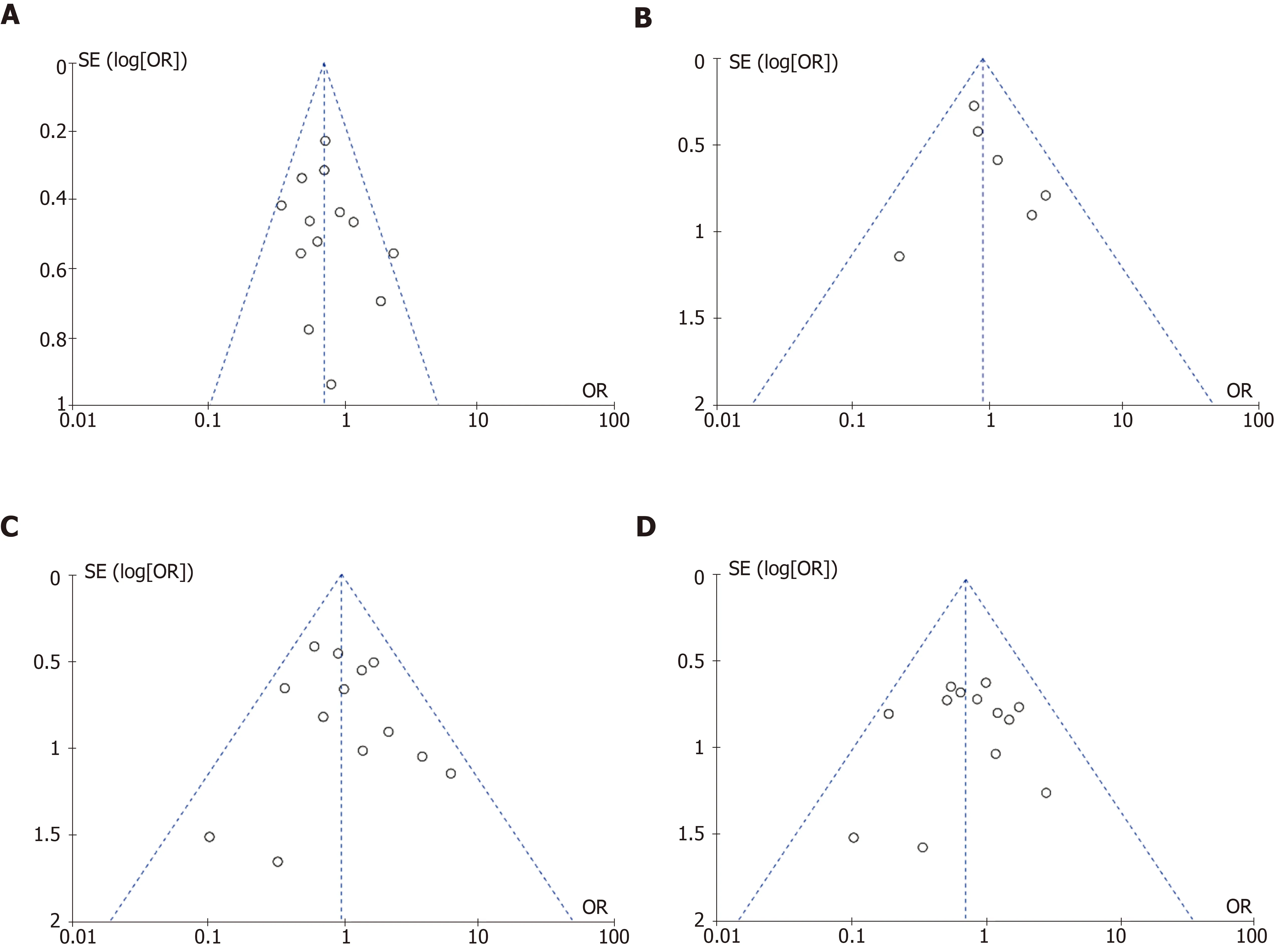
Figure2 Funnel plots of eligible studies.A:Incidence of pulmonary complications; B:Incidence of cardiac complications; C:Incidence of anastomotic leak; D:Total mortality.
ARTICLE HIGHLIGHTS
Research background
The first line treatment regimen for esophageal cancer is still surgical resection and the choice of surgical scheme depends on the surgeon.
Research motivation
Now the efficacy comparison of hybrid minimally invasive esophagectomy (HMIE) and open esophagectomy (OE) is still controversial.
To compare the perioperative and postoperative outcomes of HMIE and OE in patients with esophageal cancer.
Research objectives
Research methods
PubMed,EMBASE,and Cochrane Library databases were searched for related articles.
Research results
Seventeen studies including a total of 2397 patients were selected.HMIE was significantly associated with less blood loss (SMD = -0.43,95%CI:-0.66,-0.20; P = 0.0002) and lower incidence of pulmonary complications (OR = 0.72,95%CI:0.57,0.90; P = 0.004).
Research conclusions
Compared with OE,HMIE shows less blood loss and pulmonary complications.
Research perspectives
Further studies are necessary to evaluate the long-term oncologic outcomes of HMIE.
杂志排行
World Journal of Gastrointestinal Oncology的其它文章
- New era for pancreatic endoscopic ultrasound:From imaging to molecular pathology of pancreatic cancer
- Endothelial cells in colorectal cancer
- Non-coding RNA in drug resistance of gastric cancer
- Calponin 3 promotes invasion and drug resistance of colon cancer cells
- Eight key long non-coding RNAs predict hepatitis virus positive hepatocellular carcinoma as prognostic targets
- Toll-like receptor 9 polymorphisms and Helicobacter pylori influence gene expression and risk of gastric carcinogenesis in the Brazilian population.