Comparison of fibrin glue and sutureless autologous conjunctival flap fixation in the treatment of pterygium
2019-11-12
Manipur Raviraj Sahana, Chikkanayakanahalli Venugopal Kavitha, Acharya Pavana, Bomalapura Ramamurthy Lakshmi
Abstract
INTRODUCTION
Pterygium is a common conjunctival degenerative disorder. It is an abnormal growth of wing shaped fold of conjunctiva and fibrovascular tissue encroaching on to superficial cornea always in the palpebral fissure, more often nasally than temporally[1-2]. The term derives from the Greek word pterygium that means wing, since it is a winged shaped tissue with its base located on the periphery and the apex invading the cornea[3].
The prevalence rate of primary pterygium varies from 0.7%-31% in various populations around the world. Occurs more frequently in countries close to the Equator with warm weather and working populations exposed to the sunlight[4]. Hence risk factors include Ultraviolet radiation and hot, dusty, windy, dry, smoky environments[5-6]. Ultraviolet light may induce chronic inflammatory cells in the conjunctiva or damage limbal stem cells[7]. Development of majority of pterygium on the nasal limbus is attributable to reflected sunlight being preferentially focused on this point. The way of interaction of ultraviolet light with the limbus and cornea to produce a pterygium is unknown.
Genetic factors also play important role since some racial groups are affected more than others and pterygium has tendency to occur in families[8]. Based on a study of one or two families, Autosomal dominant mode of inheritance has been reported however, a large sample is necessary to increase credibility[9].
Pterygia warrant treatment when they encroach upon cornea (3-4 mm), induce significant astigmatism, or become cosmetically bothersome, recurrent inflammation and restricted ocular motility[1-2].
Since medical treatments are unsatisfactory, surgical removal is the treatment of choice. A variety of surgical techniques have been developed in pterygium management[1].
Very high recurrence rate of 30%-70% is associated with bare sclera excision alone. Adjunctive postoperative therapies like beta-irradiation or topical thiothepa, 5-fluorouracil and mitomycin C will reduce the recurrence rate to 4%-43% but are associated with complications. Autologous conjunctival grafting is the best method with recurrence rate as low as 2% and fewer side effects[10].
The conjunctivolimbal autograft can be secured to the bare sclera by sutures, fibrin glue or by suture less glue free methods. Suturing is associated with prolonged operating time, postoperative discomfort, and suture-related complications whereas tissue adhesives will shorten operating time, improve postoperative comfort, and avoid suture-related complications[11]. Suture less and glue free limbal conjunctival autograft is found to be safe, effective, and economical with lower postoperative suture related complications, less patient discomfort and greater patient satisfaction[12].
Many clinical studies have been carried on suturing, fibrin glue or suture less glue free methods for fixation of conjunctivolimbal autograft but very few clinical studies on size of conjunctivolimbal autograft are there at present. As suture less and glue free methods are very economical, we wanted to know the outcome in this method as it could be very effective in treating patients attending our institute outpatient department. The graft stability would be better in the last two techniques, if the graft is of adequate size preferably 0.5-1 mm larger than bare sclera area. So an effort has been made to find out the outcome among fibrin glue and suture less glue free methods of securing the two different sizes of conjunctivolimbal autograft for primary pterygium surgery.
The aim was to compare the outcome in terms of patient comfort, graft stability, graft inflammation, recurrence and other postoperative complications between the two sizes of conjunctivolimbal autograft used: a) Same as bare sclera area; b) 1 mm larger than bare sclera area and tucking it under the margins of conjunctival edge. In fibrin glue and suture less glue free methods of conjunctivolimbal autograft fixation for primary pterygium surgery.
SUBJECTS AND METHODS
InstitutionalEthicalClearancewasTakenfortheStudyIECNO:8/2014A prospective interventional comparative study was conducted on 80 consecutive eyes of 80 patients with primary pterygium who fullfil inclusion and exclusion criteria. Simple Random Sampling of all the patients diagnosed with primary pterygium attending the outpatient Department of Ophthalmology at Sri Chamarajendra Hospital, HIMS, Hassan from December 2014 to August 2016 was done. Patients with nasal or temporal pterygium consenting for surgery, patients above 18 years in different sex, patients with primary pterygium were included in the study. This study also followed the terets of the Declaration of Helsinki.
Patients not willing for the surgery, recurrent pterygium, patients less than 18 years of age, atrophic pterygium, patients on anticoagulants, patients with pre-existing glaucoma, patients with immune system disease, eyelid or ocular surface diseasese.g. blepharitis, sjogrens syndrome and dry eye, history of previous ocular surgery or trauma were excluded from study.
A total of 80 patients with primary pterygium were enrolled into the study after taking informed and written consenti.e. after informing the study subjects the details of the procedure and probable complications in their local language.
After taking necessary history regarding medical history, drug history, history of previous surgery, each patient underwent comprehensive ophthalmic examination using slit lamp biomicroscopy and grading of pterygium was done based thickness and vascularity using Tan grading system.
The study subjects were randomly selected and were divided into 2 groups. Group 1, (subjects were underwent fibrin glue) and group 2, (subjects were underwent suture less glue free methods of conjunctivolimbal autograft fixation). For each group equal numbers of subjects were enrolled and further each group was divided into 2 more groups by random selection. Group A (size of autograft same as bare sclera), group B (size 1 mm larger than bare sclera) among group receiving fibrin glue technique and group C (size of autograft same as bare sclera), group D (size 1 mm larger than bare sclera) among group receiving suture less glue free technique of conjunctival autograft fixation.
After all necessary investigations, physician fitness and consent for surgery, they were posted for pterygium surgery.
Each patient underwent pterygium excision with or without fibrin glue with size of conjunctivolimbal autograft used as per the respective group.
FibrinGluePreparationIn group 1, fibrin glue (Tisseel fibrin sealant Baxter) was used. The mixing of the component was done as per the manufacturer’s directions. The procedure requires the addition of the fibrinolysis inhibitor, Aprotinin (small blue bottle) to the sealer protein concentrate vial (large blue bottle) followed by warming. The thrombin component is prepared by injecting the contents of calcium chloride vial (small black bottle) into the thrombin vial (large black bottle/white bottle). Large black bottle causes rapid clot formation while with white bottle rate of clot formation is slow. In our technique, the white bottle was used always so that slow clotting will give enough time to the surgeon to align the graft while attaching. The vials are then warmed for several minutes. When solutions are prepared they are drawn into two different syringes. These syringes are then placed into the duploject injector (Figure 1) which is specially designed so that depressing the common plunger exerts simultaneous and equal pressure on both the syringes. A mixer nosecone, topped by a blunt applicator needle, is attached to the nozzle to facilitate the mixing of the two syringe components.
SurgicalTechniqueUnder aseptic precautions, peribulbar anesthesia was given to all cases. Ocular surface and the surrounding area were disinfected with 5% povidone-iodine and the surgical area was covered with a sterile drape. After insertion of a lid speculum, the pterygium was incised along the limbus down to the bare sclera and the head of the pterygium was removed by blunt dissection from the base to the apex. The head of the pterygium was then avulsed from its corneal attachment by reverse stripping using slow, firm and deliberate traction by holding it at its base parallel to the cornea. The conjunctiva was reflected backward and fibrovascular tissue underneath the cut end of the conjunctiva was dissected as far as possible on the canthus side and excised, leaving the sclera and the muscle free from episcleral tissue. Tenon’s tissue was carefully removed from the region of the conjunctival defect and from under the surrounding conjunctiva and bleeding allowed to achieve natural hemostasis. Excessive hemorrhage in the graft bed was tamponaded. Cautery was avoided on the bare sclera, except in few cases with brisk bleeding points. The dimensions of the resulting conjunctival defect were measured using a caliper. The donor tissue was harvested from the same eye. An area of conjunctiva at the superotemporal area, same as bare sclera or 1mm larger than the size of the bare sclera, depending on group allotted, was measured with a caliper and marked. Conjunctiva was elevated by subconjunctival injection of normal saline. Sharp dissection was used to make two parallel radial incisions along the marked lines and conjunctival scissors to undermine the conjunctiva from the lateral borders taking care to avoid inclusion of the Tenon’s tissue beneath it. Non-toothed conjunctival forceps was used to handle the graft tissue to avoid any injury to the edges and button-holing. When the posterior and lateral ends of the graft were free, conjunctiva was cut along the posterior border. The free conjunctiva, still attached anteriorly, was reflected upon the cornea and blunt dissection was continued anteriorly till the limbus. Westcott scissor was used to dissect towards the peripheral cornea for about 1 mm beyond the vascular arcade to include limbal stem cells in the graft. The conjunctival graft was then excised. The graft was placed on the bare sclera, with epithelial side up in such a way as to maintain the original orientation of the juxtalimbal border towards the cornea. In the fibrin glue group (groups A and B), each syringe of fibrin glue, which is filled with clottable protein with aprotinin or thrombin with calcium chloride solution respectively, was prepared. These two components were mixed in appropriate proportions during application using dual injection (duploject) system and were applied to the exposed sclera, using as little as possible, by pushing the double syringe device at the same time. Thrombin solution quickly sets to form white, elastic mass which firmly adheres the tissue. Both wound margins were held together with tooth forceps to ensure adhesion. In the suture less glue free group (groups C and D) Autologous fibrin rich serum was allowed to glue the graft to the bed and the scleral bed was viewed through the transparent conjunctiva to ensure that residual bleeding did not lift the graft. The free graft was placed over scleral bed and allowed to dry in position for 5min. Then, the lid retractors were removed after ensuring graft adherence. All the groups received subconjunctival injection of antibiotic and corticosteroid at the end of the procedure away from the site of the graft and the eye was bandaged for 24h. The donor site was allowed to heal leaving it bare. Duration of surgery was measured starting from the placement of the lid speculum to its removal at the end of the surgery.

Figure 1 Duploject injector.
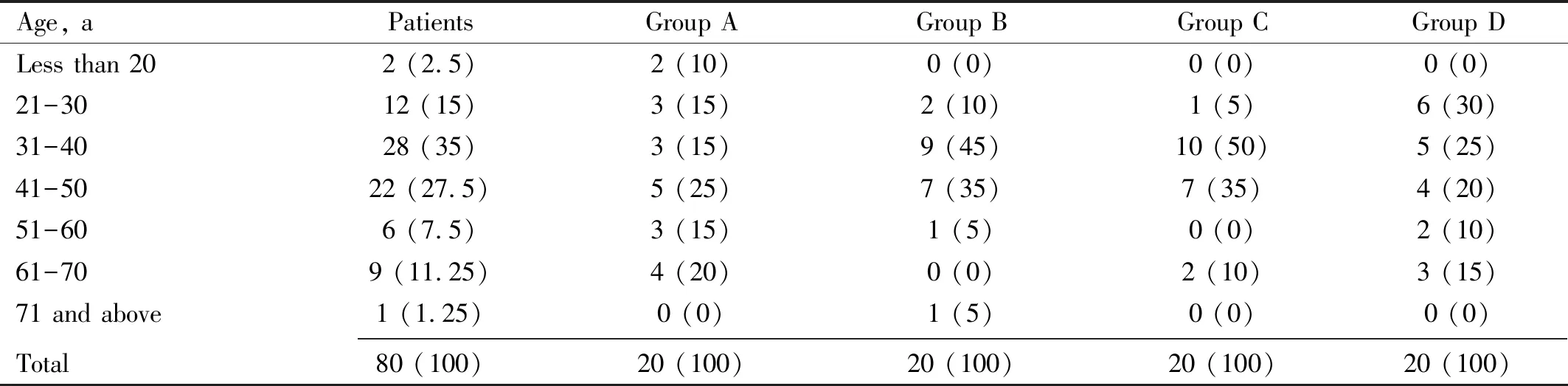
Table 1 Distribution of patients according to age n (%)
Follow-upPatients were followed-up postoperatively on 1d, 1wk, 6wk, 6mo and after 1y and in each visit patients underwent slit lamp examination and examined for graft stability, graft inflammation, graft edema, recurrence and other complications and patient comfort will be analyzed on the basis of visual analogue scale (Figure 2)
Postoperatively patients were treated with antibiotic-steroid combination eye drops 10 times a day for 1wk and tapered up to 6wk, NSAID eye drops and artificial tears 4 times a day for 6wk.
Pterygium recurrence was defined as any fibrovascular growth that has passed the limbus by more than 1 mm. Graft success was defined as an intact graft by the 6wk after surgery and graft failure was defined as absence of the graft by the 6wk. Subjective sensation of pain, foreign body sensation, tearing, and discomfort were analyzed using visual analogue scale. Postoperative grading of inflammation was done as follows[3]: Grade 0- no dilated corkscrew vessel in the graft; Grade 1-1 bright red, dilated corkscrew vessel crossing the graft bed margin; Grade 2-2 bright red dilated corkscrew vessels crossing the graft bed margin; Grade 3-3 bright red dilated corkscrew vessels crossing the graft bed margin; Grade 4- ≥3 bright red dilated corkscrew vessels crossing the graft bed margin.
Graft edema is graded as Grade 0 (nil): graft is tightly attached to the sclera and there is no graft edema; Grade 1 (mild): graft is attached to the limbus but there is mild graft edema; Grade 2 (moderate): graft is moderately edematous at the limbal level; Grade 3 (serious): heavy graft edema[13].
Subconjunctival hemorrhage is graded as: Grade 0- none; Grade 1 -≤25% of size of the graft; Grade 2-≤50% of size of the graft; Grade 3 -≤75% of size of graft; Grade 4-hemorrhage involving the entire graft[3].
Majority of the grafts were stable and assessment for graft stability is graded as Grade 0:all four sides of the graft margin are well apposed; Grade 1: gaping/displacement of one side of the graft-bed junction; Grade 2: gaping/displacement of two sides of the graft-bed junction; Grade 3: gaping/displacement of three sides of the graft-bed junction; Grade 4: graft completely displaced from the bed[3].
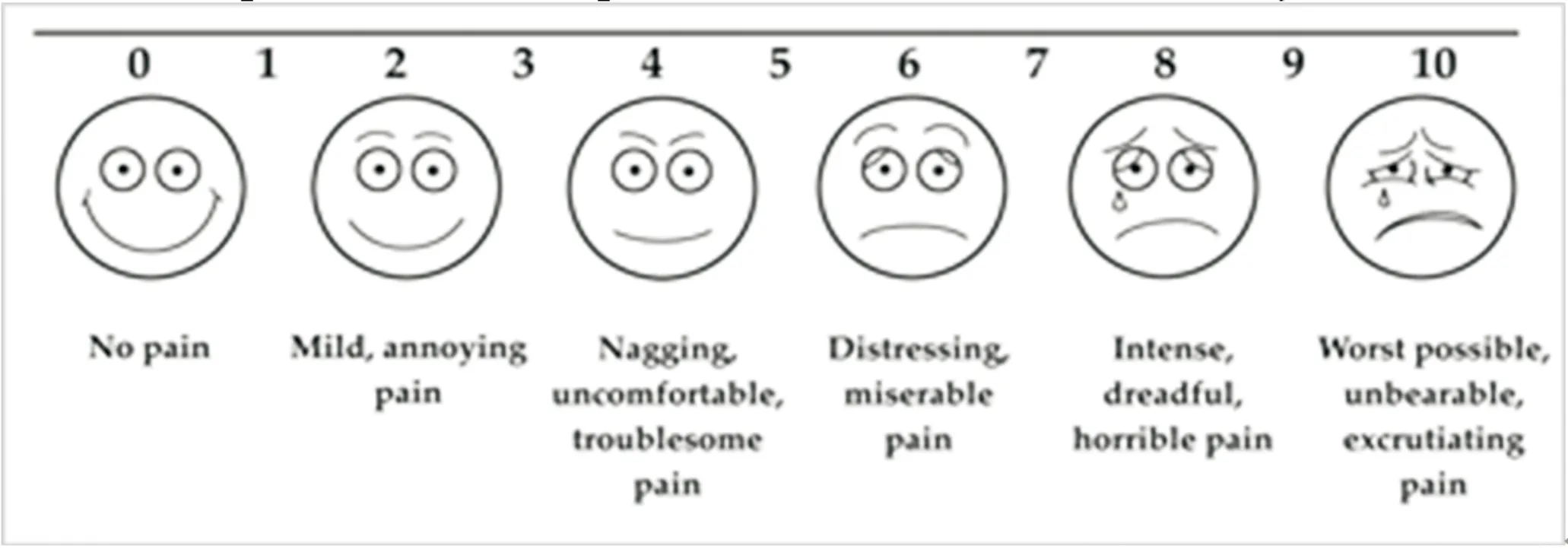
Figure 2 Visual analogue scale.
StatisticalAnalysisData was entered in Microsoft Excel and analyzed using SPSS version 21 software. Descriptive statistical analysis was done. The results were expressed in frequencies, percentage, means, and standard deviations.
Tests of significance such as Chi-square test and Fisher exact test were used for categorical variables and ANOVA was applied for continuous variables. Results withPvalue < 0.05 were considered as significant.
RESULTS
Mean age of the patients in group 1 was 43.525 years and in group 2 was 42.2 years (Table 1). Females were 60 and males were 20 (Table 2). All 37 patients had pterygium in RE (Figure 3). Majority of the patients were of Tan Grade 3 in all the groups (Figure 4). Distribution of patients according to the extent of pterygium in all the groups was comparable (Figure 5). Average surgical time was similar in all the four groups (Figure 6). Postoperative parameters like patient comfort, graft retraction, graft inflammation and graft edema were similar in all the four groups during every postoperative follow-up visits except for subconjunctival haemorrhage which was significantly more in fibrin glue group until first postoperative week (P<0.0001). Grade 4 graft retraction/displacement was observed in only three patients from sutureless glue free group. At 1wk postoperative, graft cyst was observed in two patients (one in Group A and one in group D). Recurrence was observed in two patients (in group D) at 6mo follow-up (Table 3, Figure 7). Other postoperative complications observed were dellen, donor site tenon’s inflammation and donor site granuloma in group A, group D and group B respectively. Resolved with topical steroids, need not required further surgery (Table 4). No serious, eye-threatening infection, corneal or scleral melting, neovascularization, conjunctivalization at the superior limbus occurred.

Table 2 Distribution of patients according to sex n (%)
Table 3 Distribution according to postoperative parameters
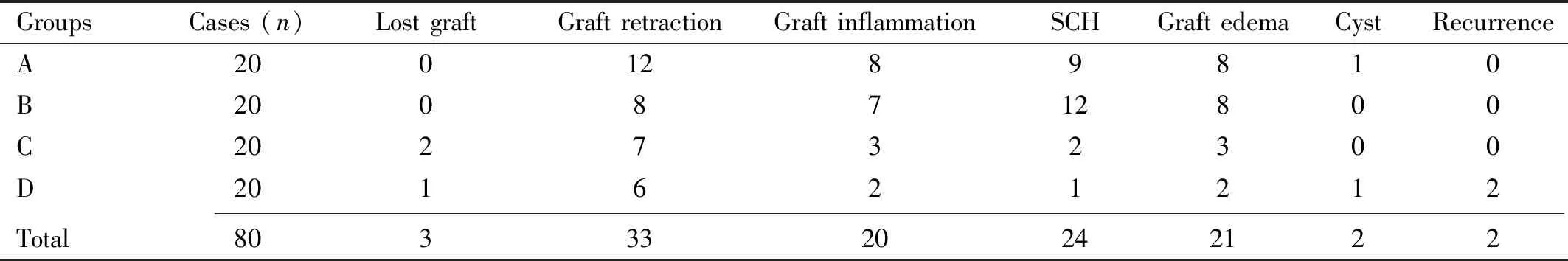
GroupsCases (n)Lost graftGraft retractionGraft inflammationSCHGraft edemaCystRecurrenceA2001289810B2008712800C202732300D201621212 Total8033320242122
SCH: Subconjunctival haemorrhage.
Table 4 Distribution according to other postoperative complications
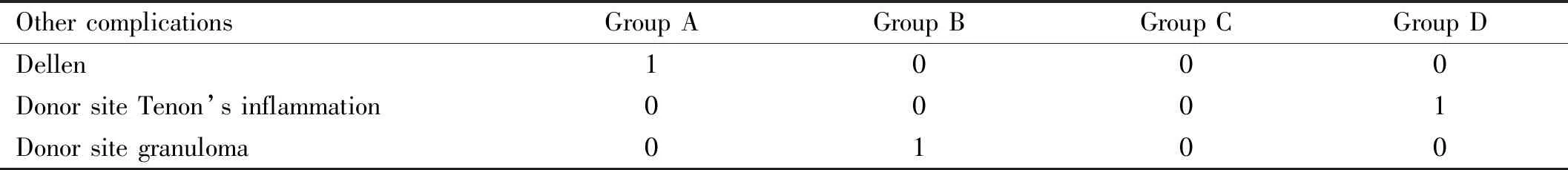
Other complicationsGroup AGroup BGroup CGroup DDellen1000Donor site Tenon’s inflammation0001Donor site granuloma0100
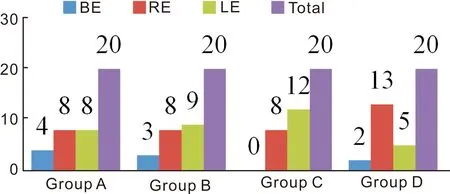
Figure 3 Distribution of patients according to laterality of pterygium.

Figure 4 Distribution of patients according to tan grading of pterygium.
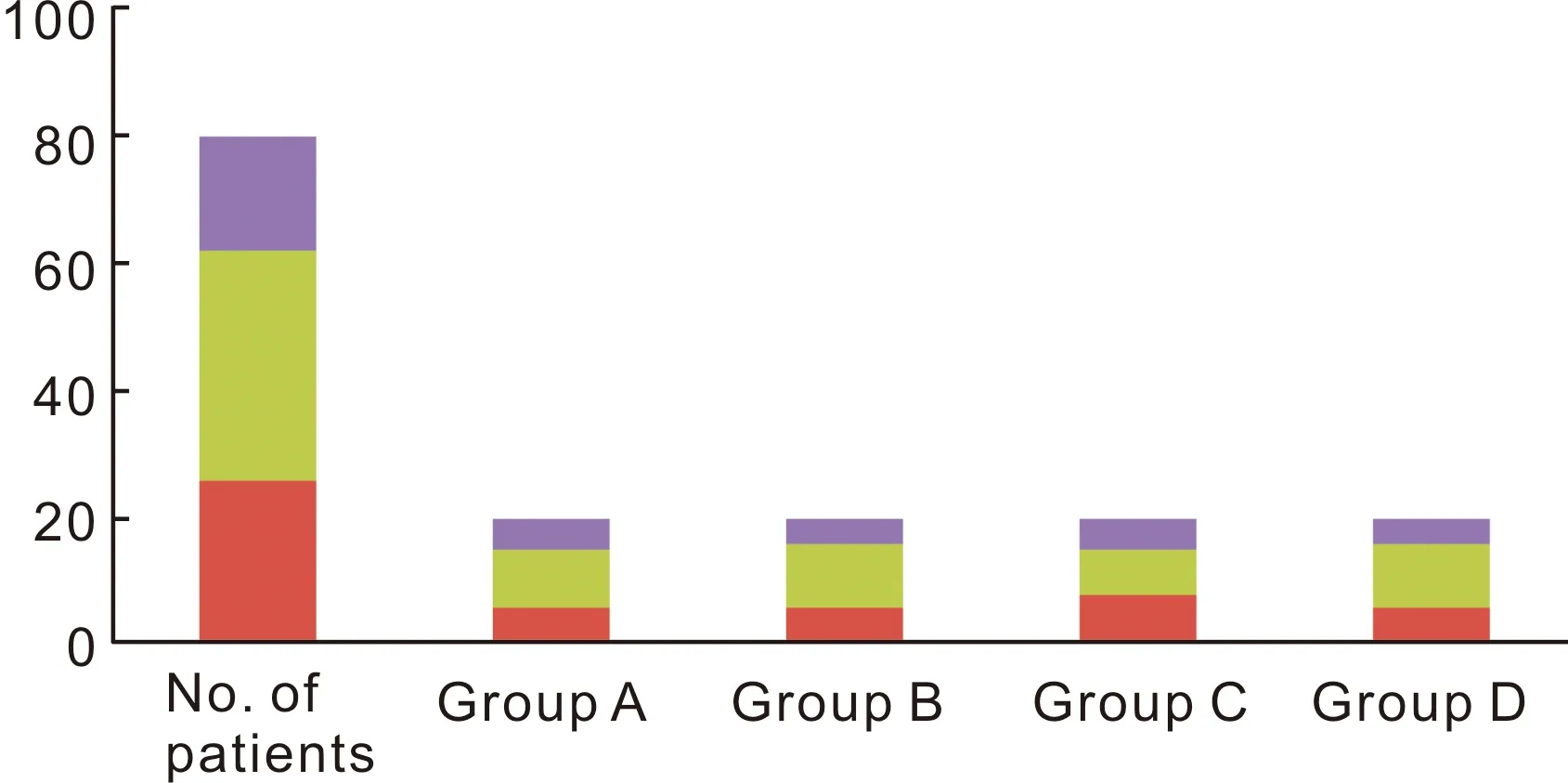
Figure 5 Distribution of patients according to extent of pterygium.
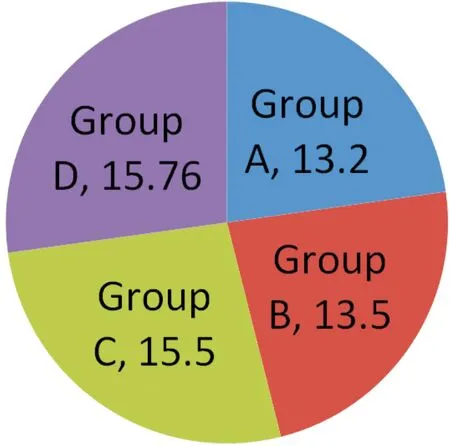
Figure 6 Durations of surgery (min) in all groups.
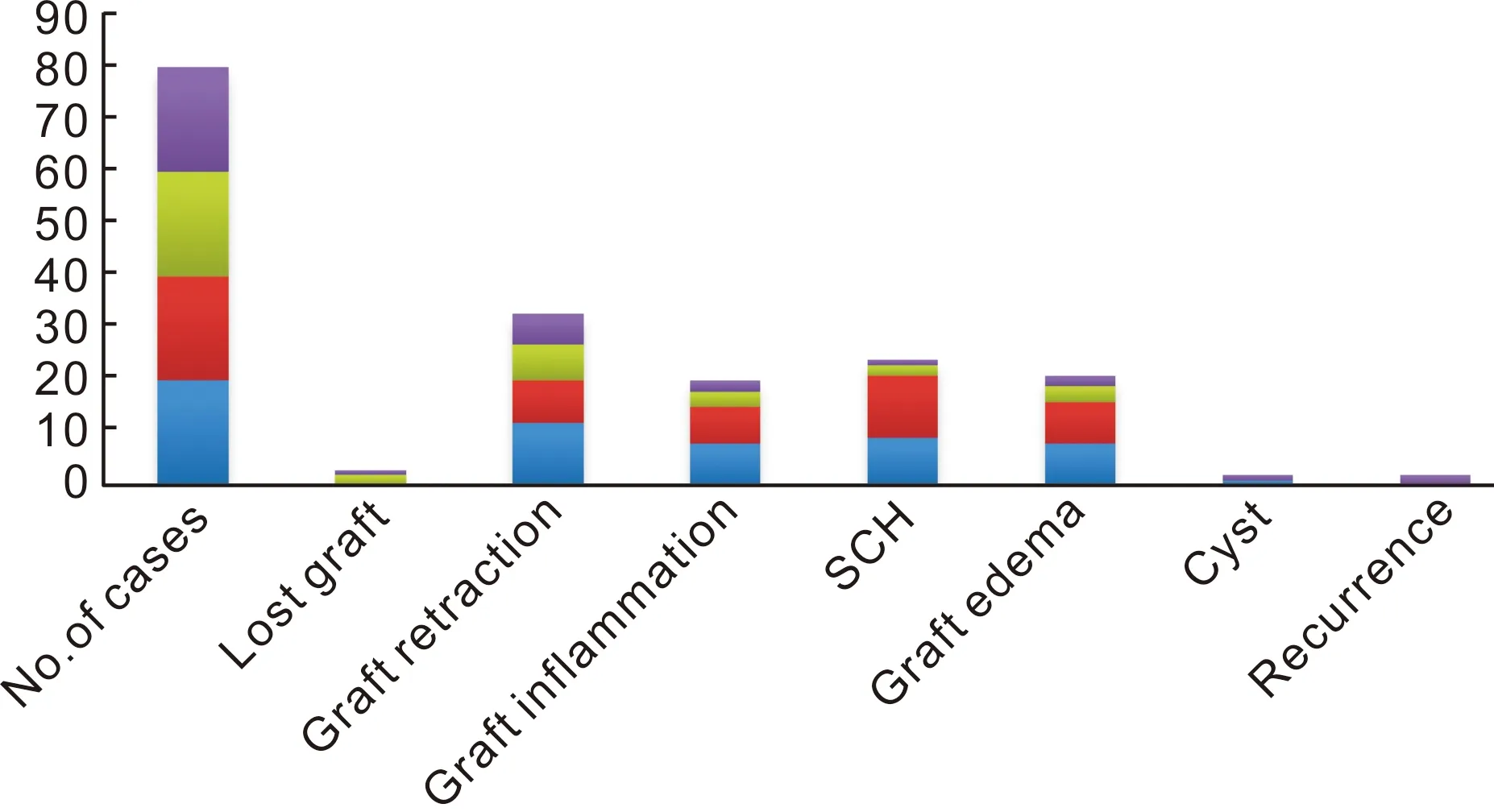
Figure 7 Distribution according to postoperative parameters.
DISCUSSION
A pterygium is a relatively common conjunctival degenerative condition. Amongst the various risk factors, UV exposure is the most common. Simple excision of pterygium is associated with a high recurrence rate ranging from 30%-70%. To reduce this high recurrence rate, different methods like application of adjuvant therapies, Amniotic membrane graft, conjunctival autografts with sutures, glue, suture less glue free methods have been employed.
Each has its benefits, but none is without drawbacks. Complications with mitomycin-C include persistent epithelial defects of the cornea, corneal melting, endophthalmitis, infectious scleritis, perforation scleral necrosis, cataract and glaucoma[14-15]. The use of 5-FU as an adjunct to pterygium surgery has so far been associated with only minor and transient complications[15]. Current surgical methods to prevent pterygium recurrence include conjunctival autograft, limbal and limbal-conjunctival transplant, conjunctival flap and conjunctival rotation autograft surgery, amniotic membrane transplant, cultivated conjunctival transplant, lamellar keratoplasty, and the use of fibrin glue. All of these techniques involve the use of sutures or fibrin glue and are therefore vulnerable to associated complications[16]. Sutures do not actively participate in wound healing and may cause additional trauma to the injury site and adjacent tissue. Also, infectious agents might enter along the suture tract, or the sutures might act as the nidus of the inflammation itself. Loose or broken sutures require removal and, hence, additional working time[17]. Koranyi and associates were the first to report the use of fibrin glue for CAG in pterygium surgery. They observed that CAG tends to vascularise during the first postoperative week from the underlying episcleral vascular bed and that the use of fibrin glue provided better contact with underlying tissue resulting in its immediate adhesion and vascularisation of graft thus preventing recurrence. Reduction in surgical time and postoperative pain was also reported by the authors[10]. Since fibrin adhesives are prepared from pooled donor sources, there is a small but finite risk of infection, such as hepatitis and HIV, as well as of anaphylactic reaction. The infection risk is reduced by testing donors for viral markers, at the time of donation and 6mo later and also by sterilization of the products by gamma irradiation and treatment with detergents or solvents[15].
Interestingly, a recent study suggested autologous fibrin in blood as a useful alternative to fibrin glue for pterygium surgery, though preparation can be laborious, requiring special equipment not available to most surgeons[18].
Suture less and glue-free conjunctival autograft is a new, easy and cheaper technique for the management of pterygium. de Wit Detal[16]conducted a cross sectional study in which all records of patients undergoing pterygium surgery with conjunctival autografting in 1y period were reviewed. A total of 15 eyes in 12 patients (mean age: 73.7±11.2) years underwent suture less glue free autologous conjunctival graft after pterygium excision. There were eight female and four male patients. All patients had primary nasal pterygium. Mean follow-up time was 9.2±2.2mo. Mean graft area was 24±1.5 mm. The mean surgical time was 14±1.4min. There were no transplant dislocations or failures. There were no intra- or postoperative complications requiring further treatment. Visual acuities were not affected in the majority of patients. Patients rated their cosmesis as excellent in all cases and photographic comparison of nasal to temporal conjunctiva at last review revealed no obvious cosmetic defects or recurrences. Postoperative pain on 1d after surgery was consistently rated as less than or equal to 2 out of 10 on a visual analogue score. Pain did not increase after the first postoperative day. The operating time, postoperative symptoms, recurrence, and complication rate appears to be equivalent to conventional suture and glue techniques of a similar follow-up duration. Specifically, the risk of graft retraction as appears to be no greater without suturing or fibrin glue as long as meticulous dissection of the subepithelial graft tissue is respected and also postulated that as there is an even tension across the whole of the graft interface and no direct tension on the free graft edges, there is reduced stimulus for subconjunctival scar tissue formation.
A prospective randomized controlled trial is required to investigate the long-term efficacy of this SGF grafting technique in reducing recurrences. Rathietal[19]concluded in their study that blood oozed during pterygium excision may provide novel approach for securing conjunctival autograft.
This study was conducted on 80 eyes of 80 patients with pterygium. The study groups were randomly selected and were divided into 2 groupsi.e. group of people undergoing fibrin glue and those underwent suture less glue free methods of autograft fixation. For each group equal numbers of subjects were enrolled and further each group was divided into 2 more groups by random selection. Group A (size of autograft same as bare sclera) group B (size 1 mm larger than bare sclera) among group receiving fibrin glue technique and group C (size of autograft same as bare sclera) group D (size 1 mm larger than bare sclera) among group receiving suture less glue free technique of conjunctival autograft fixation. All underwent elective pterygium surgery. Two patients from group C and 1 patient from group D had total dislocation of the graft on the first postoperative day and hence were not included in further study for assessing other parameters. These parameters were studied in the remaining 77 patients. At 6mo follow-up 2 patients were excluded due to recurrence and parameters were studied in remaining 75 patients during further follow-up.
Distribution of patients according to age was similar in all the four groups. Mean age of the patients in Group 1 was 43.525 years and in Group 2 was 42.2 years. Group A was 44.4 years, Group B was 42.65 years, Group C was 42.35 years and in Group D was 42.05 years. There was no statistically significant difference between the groups in terms of mean age (P=0.945).
All patients were having nasal pterygium. Elwanetal[12]reported that the pterygia were located nasally in all eyes and patient age was ranged from 24-74 (mean: 4±12) years. Females in group A and group B were 13 each, in group C were 19 and in group D were 15. Males in group A and group B were 7 each, 1 in group C and in group D were 5 and were comparable. Females accepted the surgery earlier than males, probably because of cosmetic reason. There was no statistically significant difference between the two groups in terms of sex (P=0.0707).

Figure 8 Fibrin glue group patients on 1d and 1wkA: Graft oedema; B: Graft inflammation; C: Mild nasal graft retraction; D: Subconjunctival haemorrhage.
In a study conducted by Chaetal[5]there were 7 males and 13 females in the fibrin glue group and 4 males and 22 females in the suture group. Females were more. Number of patients with pterygium in both eyes in group A were 4, in group B were 3, in group D were 2; patients with pterygium in the right eye in groups A, B and C were 8 each, in group D were 13; patients with pterygium in the left eye in group A were 8, in group B were 9, in group C were 12 and in group D were 5. Majority of the patients had pterygium in right eye.
Distribution of patients according to the Tan grading of pterygium in all the groups was comparable (numbers of patients with Grade 2 pterygium in Group A were 7, in group B and group D were 6 each, in group C were 8; with Grade 3 pterygium in group A were 13, in group B and group D were 14 each, in group C were 12). Majority of the patients were of Grade 3 in all the groups, probably because the patients with an early grade did not accept surgery. None had grade 1 since they were excluded from the study.
Distribution of patients according to the extent of pterygium in all the groups was comparable (number of patients with Grade 2 pterygium in groups A, B and D were 6 each, in group C were 8; with Grade 3 pterygium group A were 9, group B and D were 10 each, in group C were 7; with Grade 4 pterygium in groups A and C were 5 each, in groups B and D were 4 each) however patients with Grade 3 pterygium were more.
Average duration of surgery in group A was 13.2min, in group B was 13.5min, in group C was 15.5min and in group D was 15.76min. Slightly prolonged duration in group C and D is due to time taken for allowing autogenous fibrin rich serum to glue the graft to the bed.
Koranyietal[6]in their study mentioned median surgery time was 10 (range 6-13) min in the glue group and 17 minutes (range 12-30) in the suture group (P<0.001). In a study conducted by Chaetal[5]the surgery duration was 27.71 (5.22) min in the fibrin glue group, which was remarkably shorter than that in the suture group 43.30 (8.18) min.
On 1d postoperative, pain was more in Group B than in other groups, however the difference was not found to be statistically significant between groups 1 and 2 (P=0.5027), groups A and B (P=0.7616) and the groups C and D (P=0.5307). Graft inflammation between groups 1 and 2 (P=0.1892), groups A and B (P=0.8954) and the groups C and D are not significantly different (P=0.8025). Graft edema between groups 1 and 2 (P=0.1781). The groups A and B (P=0.9506) and the groups C and D are not significantly different (P=0.8025) (Figure 8).
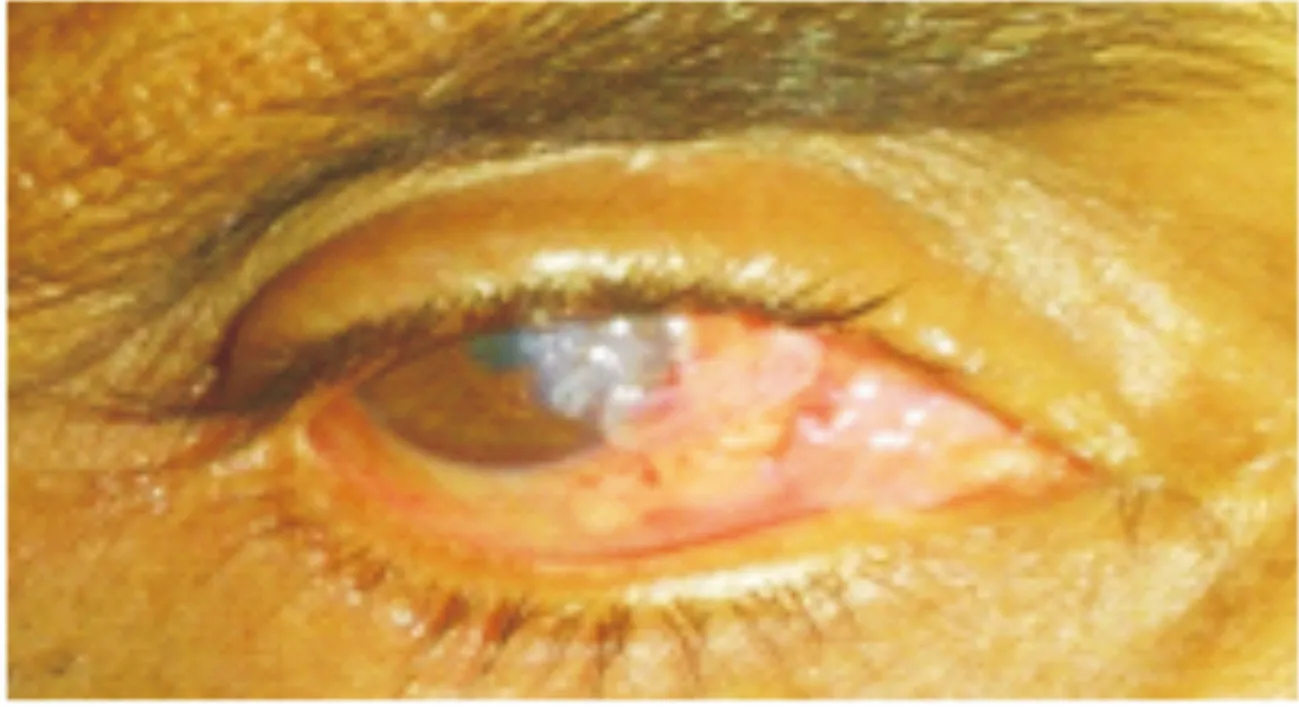
Figure 9 Case 19: grade 4 graft displacement (irretrievably) at 1d postoperative.

Figure 10 Case 30: grade 4 graft displacement (irretrievably) at 1d postoperative.

Figure 11 Displaced graft.
In group A, twelve patients had grade 1, in Group B seven had grade 1 and one patient had grade 3 graft retraction (graft was repositioned under aseptic precautions), in group C four patients had grade 1, 1 patient had grade 3 (graft was repositioned under aseptic precautions), two had grade 4 graft retraction (in these two cases the graft was found to be displaced irretrievably, Figures 9-11), in group D, three patients had grade 1, two patients had grade 3 and one patient had grade 4 graft retraction (in this case the graft was found to be displaced irretrievably). The groups 1 and 2 (P=0.066), groups A and B (P=0.4) and the groups C and D are not significantly different (P=0.3759). In two cases of group C and one case of group D, the graft was displaced irretrievably; hence they were excluded from further study.
Subconjunctival haemorrhage was found to be statistically significant difference between groups 1 and 2. SCH was more in fibrin glue group.
At 1wk postoperative follow-up, patient comfort in the groups 1 and 2 (P=0.2644), groups A and B (P>0.9999) and the groups C and D are not significantly different (P=0.6599). Graft retraction in the groups 1 and 2 (P=0.0834), groups A and B (P=0.228) and the groups C and D are not significantly different (P>0.9999). Graft inflammation in the groups 1 and 2 (P=0.0604), groups A and B (P=0.7572) and the groups C and D are not significantly different (P=0.6599).Graft edema in the groups 1 and 2 (P=0.0524), groups A and B (P=0.9506) and the groups C and D are not significantly different (P=0.7959). There is a statistically significant difference in terms of Subconjunctival haemorrhage between groups 1 and 2 (P<0.0001) whereas no such difference between groups A and B (P=0.3809) and groups C and D (P=0.7359) (Figures 8 and 12).
Cyst was seen in one patient each in group A and group D but groups 1 and 2 (P>0.9999), groups A and B (P=0.5) and the groups C and D are not significantly different (P>0.9999) (Figures 13 and 14). Cyst excision was done in group A patients.
Chaetal[5]found at 1wk after the operation, 9 out of 22 eyes (40.9%) showed moderate to severe conjunctival inflammation in the fibrin glue group and almost subsided after 3wk. Sub-graft hemorrhage, dislodgement, and contracture, did not significantly differ between the fibrin glue and suture group.
Srinivasanetal[3]found no significant difference in the degree of SCH between the fibrin group and suture group at any point during the follow-up period (P=0.417,P=1 andP=1, at 1wk, 1mo and 3mo, respectively).
Elwanetal[12]found early graft retraction with exposure of scleral bed in 6 eyes (12%) in suture less glue free group and conjunctival edema occurred in 8 eyes (16%).
At postoperative week 6, patient comfort, graft inflammation and graft edema between groups 1 and 2 (P>0.9999), groups A and B (P>0.9999) and the groups C and D are not significantly different (P>0.9999). Graft retraction between the groups 1 and 2 (P=0.0504), groups A and B (P=0.5404) and the groups C and D are not significantly different (P>0.9999) (Figure 15). Subconjunctival haemorrhage seen in only one patient in group C and the groups 1 and 2 (P=0.4805), groups A and B (P>0.9999) and the groups C and D are not significantly different (P=0.4865).
At 6mo and 1y postoperative follow-up, patient comfort, graft retraction, graft inflammation, subconjunctival haemorrhage and graft edema between groups 1 and 2 (P>0.9999), groups A and B (P>0.9999) and the groups C and D are not significantly different (P>0.9999).

Figure 12 Case 5: grade 1 inflammation and graft oedema.
At 6mo postoperative, 2 patients in group D showed recurrence and recurrence between groups 1 and 2 (P=0.2276), groups A and B (P>0.9999) and the groups C and D are not significantly different (P=0.4865) (Figures 16 and 17). Hence recurrence occurred in two patients with tan grade 3 and grade 4 extent of pterygium who were treated with suture less glue free method of conjunctival autograft fixation using graft size 1mm more than bare sclera. Recurrent pterygium was excised and re-graft was done in both the cases.
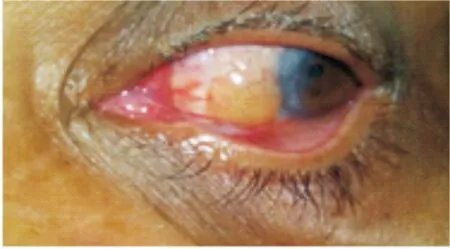
Figure 13 Case 9: postoperative cyst formation at 1wk.
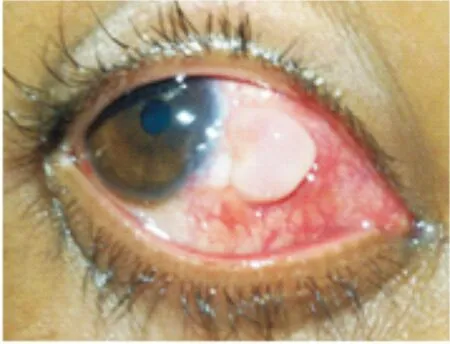
Figure 14 Case 76: cyst formation at 1wk postoperative.

Figure 15 Case 27: grade 1 graft retraction at 6wk.
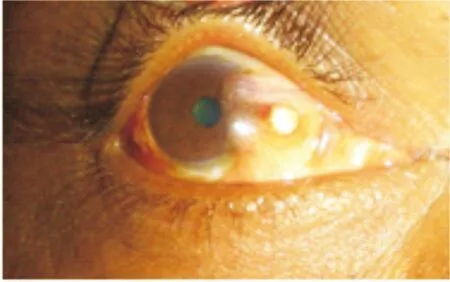
Figure 16 Case 10: recurrence at 6mo follow-up.

Figure 17 Case 12: recurrence at 6mo follow-up.
Chaetal[5]reported the recurrence rate of corneal pterygium within three months of the surgery was 4.55% (1 of 22 eyes) in the fibrin glue group and Koranyietal[6]reported two recurrences in the glue group (8%) and were seen within 6mo follow-up. The immediate adhesion of the whole graft may inhibit the fibroblasts of the nasal Tenon’s tissue from proliferating towards the cornea, keeping recurrence rate low.
Elwanetal[12]reported recurrence rate of 6% (3 eyes) in suture less glue free group. All cases of recurrences occurred after 3mo. Bhatiaetal[20]reported recurrence in 6.8% of cases (14 cases).
Other postoperative complications observed were dellen, donor site Tenon’s inflammation and donor site granuloma In group A, group D and group B respectively which resolved with topical steroids.
Koranyietal[6]stated that the cost of one double syringe of Tisseel Duo Quick (0.5 mL fibrin glue) is about equal to the cost of five sutures and can operate on six to seven patients on one day with the same Tisseel syringes, although those would be enough for eight to nine patients. Thus, the material cost of the cut and paste method became somewhat lower than that of the sutures. In addition, the time cost is about the half of that with sutures[6].
In our study, we found cost of 1 mL fibrin glue is about 8, 200 INR compared to suture less glue free method which we can do free of cost.
And also it is clear from the results that, there was no statistically significant difference in any of the parameters (except subconjunctival haemorrhage which was more in fibrin glue group till 1wk postoperative follow-up) between fibrin glue and suture less glue free methods.
Pterygium is a common conjunctival disorder which predominates in country like India with warm and dry climate. Treatment is often a great challenge because of high recurrence rate. Both the procedures (conjunctivolimbal autograft fixation with fibrin glue and suture less glue free methods) are less traumatic, safe and effective methods for graft adhesion during pterygium surgery. Postoperative discomfort and complications are also less. Compared to fibrin glue method, suture less and glue free method is very economical and outcome in this method compare to fibrin glue group. Outcome is same in both graft sizes in fibrin glue and in suture less glue free methods. Since this procedure is cost effective and also have all the advantages of fibrin glue, suture less glue free method can be considered as very effective method in treating patients attending our institute outpatient department.