Value of CT-Angiography in the Emergency Management of Severe Hemoptysis
2019-10-15YingChenKefeiWangZhiweiWangChangzhuLiuZhengyuJin
Ying Chen, Kefei Wang, Zhiwei Wang*, Changzhu Liu, Zhengyu Jin
1Department of Radiology, Peking the 6th Hospital, Beijing 100007, China
2Department of Radiology, Peking Union Medical College Hospital, Chinese Academy of Medical Science & Peking Union Medical College, Beijing 100730, China
Key words: hemoptysis; multidetector CT-angiography; endovascular embolization
Objective To depict imaging anatomy of bronchial artery (BA) using multidetector CT-angiography (MDCTA)and evaluate the value of MDCTA for management of hemoptysis patients requiring admission to emergency room.Methods We retrospectively studied the clinical and radiological data of patients with severe hemoptysis(≥100 ml of expectorated blood in a 24-hour period) requiring admission to emergency room from Jan 1, 2013 to Dec 31, 2015. Patients’ images of MDCTA, treatment modalities, and outcome were discussed.Results A total of 108 patients underwent MDCTA scans. Etiology of hemoptysis was mainly bronchiectasis(44%), tuberculosis sequelae (26%) and tumor (18%). MDCTA visualized 197 traceable BAs and also suggested the involvement of 35 nonbronchial systemic arteries. The mean diameter of BAs, measured at the level of the bronchial bifurcation in the mediastinum, was 2.8±1.2 mm. The mean diameter of BAs, for 52 patients who only received conservative treatment, was 2.9±1.1 mm, and was not significantly larger than that of BAs for 56 patients who underwent bronchial artery embolization (BAE) for continued bleeding which did not resolve after conservative treatment (2.7±1.1 mm, P = 0.94). The technical success rate of embolization was 95% (53/56). Clinical success rate during follow-up was achieved in 50 (94%) of 53 patients who had undergone embolization.Conclusions MDCTA provides useful information for identifying the anatomical characteristics of bleedingrelated BAs and nonbronchial systemic arteries for the management of patients with severe hemoptysis. However,MDCTA could not determine the individuals who need BAE through measuring diameter of BAs.
HEMOPTYSIS is bleeding originating from the lower airways and represents a life-threatening emergency situation requiring immediate diagnosis and therapy.This situation occurs frequently in clinical practice and requires a rapid therapeutic response. Despite substantial advances in intensive care in recent decades,massive hemoptysis remains a clinical challenge for its high mortality.[1,2]
Recently, multidetector CT-angiography (MDCTA)has been an important potential diagnostic modality for the accurate and prompt diagnosis of the underlying vascular disorder because it provides a map of the thoracic vasculature, which should be helpful for the management of this disease in emergency setting.[3-5]
Currently, the patients admitted for hemoptysis undergo MDCTA as a standard examination for the initial evaluation of hemoptysis. This study aimed to retrospectively assess the characteristics of bronchial artery (BA) using MDCTA and evaluate the role of MDCTA for management of hemoptysis cases requiring admission to emergency room.
PATIENTS AND METHODS
Patients
We retrospectively analyzed the clinical and radiological records of all patients with massive hemoptysis(≥100 ml of expectorated blood in a 24-hour period)[5]requiring admission to emergency room from Jan 1,2013 to Dec 31, 2015 in our hospitals. Patients who presented with massive hemoptysis requiring emergency bronchial artery embolization (BAE) and did not receive MDCTA prior to BAE, were excluded from the study. Bleeding status of each patient was evaluated before therapy.
MDCTA scan protocol
All CTs was performed using a 128-slice DSCT system (Somatom Definition Flash, Siemens Healthcare,Forchheim, Germany). Detector collimation was 2×64×0.6 mm. A z-axis flying focal spot was applied with an acquisition of 128 slices per rotation. Both tubes were operated at 120 kV. Scout-based automatic tube current modulation (CareDose 4D, Siemens healthcare)was used with the reference tube current-time product set at 320 mAs per rotation. Forty-five milliliters of contrast media (Ultravist 370 mgI/ml, Bayer Schering)followed by a 50 ml saline chaser were administered at 5 ml/s using a dual-head power injector (Empower,ACIST) into an antecubital vein. Scans were begun 6 s after the bolus-tracking program and detected an increase in 100 Hounsfield units (HU) in the CT value in the aorta. Axial sections for the entire dataset (1.0 mm, increment 0.6 mm) were reconstructed using a medium-soft convolution kernel. All CTA data were transferred to a workstation (Syngo.Via CTA; Siemens healthcare) for post-processing.
BA diameter was measured and MDCTA images were evaluated by 2 radiologists blinded to the patients’ clinical information. The site of origin was analyzed on transverse CT and maximum intensity projection images. BA diameters were measured at the level of the bronchial bifurcation in the mediastinum.
BAE
For patients who underwent angiography and endovascular embolization, informed consent for the embolization procedure was obtained. Vital signs were monitored with pulse oximeter, blood pressure monitor and electrocardiography. Angiography was performed under local anaesthesia with a common femoral artery approachviaa 5-Fr vascular sheath (Cordis Europa N.V.,Neth) using the Seldinger technique. Due to the BA anatomy obtained by the MDCTA, aortography was not required and selective catheterization of the BAs could be performed immediately without any searching. Microcatheters (2.7/2.9 Fr. Progreat, TERUMO, Japan)were used coaxially through the guiding catheters. The embolization was accomplished with gelatin (Gelfoam,Hangzhou Alicon Pharm Sci & Tec Co., Ltd, China) and coils (Cook, USA). Technical successful embolization was defined as no residual opacification of BAs after procedure.
Clinical outcome
All patients were followed up with clinical examination and CT examination for a mean period of 4.4 months,ranging from 1 to 14 months. Clinical success was defined as control of bleeding without repeated embolization or surgical intervention.
Statistical analyses
Statistical analyses were performed using SPSS statistical software (SPSS, version 13.0, Chicago, IL, USA).Continuous variables were expressed as mean value± SD. Inter-group differences were compared using a Kruskal-Wallis test for non parametric data and Fisher’s exactttest for parametric data. APvalue less than 0.05 was considered statistically significant.
RESULTS
General characteristics
Finally, 108 patients, including 71 men and 37 women,who underwent MDCTA scan examinations as part of the pre-therapeutic evaluation, were enrolled in this study. The cause of hemoptysis identified were bronchiectasis (44%), tuberculosis (26%), malignancy(18%) and cryptogenic hemoptysis (12%).
They were divided into two groups: hemoptysis resolved after conservative therapeutic management(Group 1) and hemoptysis did not resolve or recurred,further BAE was performed (Group 2). There was no significant difference in general characteristics between the two groups (Table 1).
CTA findings
MDCTA visualized 197 traceable BAs and also suggested the involvement of 35 nonbronchial systemic arteries. The mean diameter of BAs which was measured at the level of the bronchial bifurcation in the mediastinum was 2.8±1.2 mm. The mean diameter of BAs(2.9±1.2 mm) in Group 2 was not significant larger than that in Group 1 ( 2.7±1.1 mm,t= 0.53,P= 0.94).
MDCTA detected 104 origin sites of BAs (Figure 1) and 24 nonbronchial systemic arteries for patients in Group 2, which were also successfully discovered during BAE. Systemic artery-pulmonary artery fistulas were found in 54 patients during angiography.
Outcomes
Microcatheters failed to insert into BAs superselectively for 3 patients, so the embolization was not accomplished. The technical success rate of BAE was 95%(53/56). Patients were followed up for 1 to 14 months,and the clinical success rate was achieved in 50 (94%)of 53 patients who had successfully undergone embolization. No major complications related to the procedure occurred.
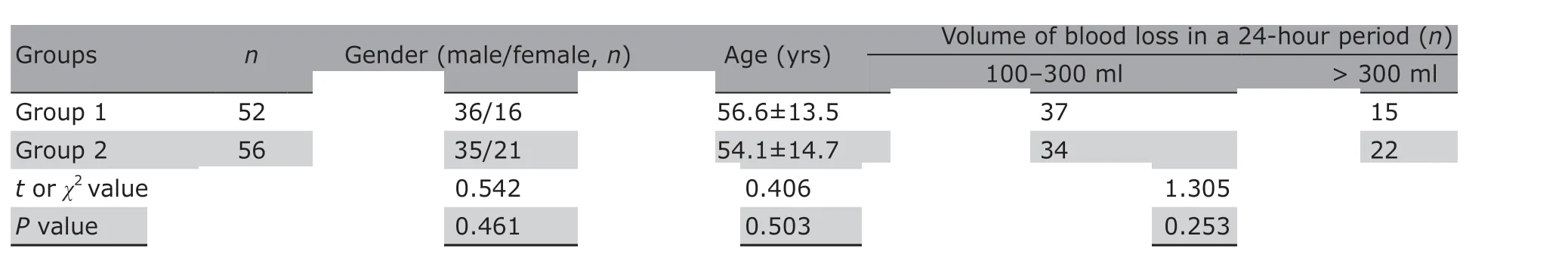
Table 1. General characteristics of the two groups
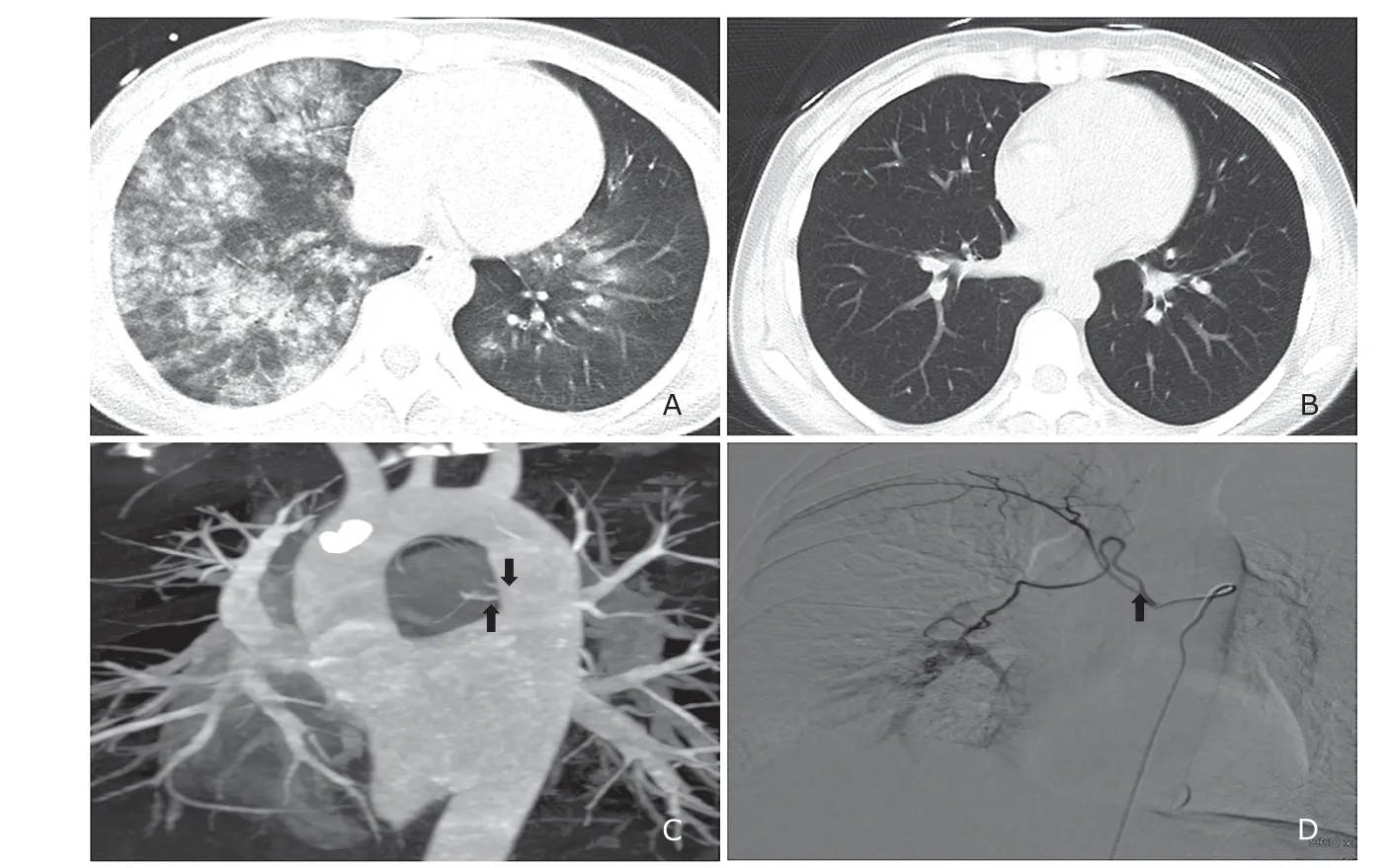
Figure 1. This is a 33-year-old woman with severe hemoptysis. A. CT showed severe hemoptysis with multiple consolidation.B. She recovered after embolization. C. MDCTA revealed moderately dilated bronchial artery. Maximal intensity projection reconstruction image demonstrated two bronchial arteries (arrows). D. She received angiography for persistent hemoptysis that was not relieved after conservative treatment. Bronchial artery-pulmonary artery fistulas was revealed (arrow).
DISCUSSION
The efficacy and safety of BAE in treating hemoptysis caused by various etiologies has been analyzed in both the short term and long term. In 90% of cases, embolization stops the bleeding immediately.[5-8]However, BAs can originate in ectopic or aberrant BAs and in those arising from systemic vessels, such as the internal mammary artery, the thyrocervical trunk, brachiocephalic trunk, subclavian, abdominal aorta, aortic arch, or inferior phrenic arteries.[9]Given the variable nature of the bronchial arterial supply, it may be difficult to identify the responsible vessels during bronchial angiography, thus leaving the patient at risk of relapse.[10]
In the last few years, several works have recommended MDCTA before BAE.[3-5]MDCTA is useful in planning the embolization procedure (selection of catheter type and size, amount of embolization material). It clearly shows the anatomy of the thoracic vasculature, thus providing important information for the interventional radiologist.[11]This approach enables detection of the localization of aberrant BAs before treatment. MDCTA can replace the routine use of preliminary flush aortography for determining the number and site of abnormal arteries. MDCTA before embolization has the potential to decrease the duration of the procedure and the exposure to radiation. These advantages increase the overall efficiency of the technique.In our study, MDCTA detected all origin sites of BAs and 24 nonbronchial systemic arteries for patients who underwent BAE. We therefore recommend routine use of MDCTA before interventions in patients with massive hemoptysis.
However, conservative treatment may be adequate to stop the hemorrhage for some hemoptysis patients, and BAE occasionally causes a serious complication such as cerebral infarction or spinal cord injury.[12]So how to select these patients who need BAE?MDCTA is not only useful in planning the embolization procedure, but also useful for evaluating severity of bleeding in the BAs and the need for BAE in hemoptysis patients.[13-16]Some authors used the degree of BA dilatation for determining whether BAE is indicated or whether conservative treatment is sufficient.[13]Moriet al.[13]retrospectively studied 41 patients and revealed the BA diameter was an independent predictive factor for BAE. Evaluation of BAs on MDCT images could be useful for determining whether BAE is indicated or whether conservative treatment is sufficient.However, the BA that is the source of the hemoptysis may not always have a large diameter in our study. In our clinical practice, the diameter of BAs in many patients with bronchiectasis may be very large, but they never experienced hemoptysis. So BAs evaluation with MDCT could not be used to determine appropriate initial management of hemoptysis. Clinical bedside evaluation and monitor may be more important.
In conclusion, MDCTA provides useful information for identifying the anatomical characteristics of bleeding-related BAs and nonbronchial systemic arteries for the management of patients with severe hemoptysis.However, MDCTA could not select which patient needs BAE through measurement of BAs diameter.
Conflicts of interest statement
All authors declare no conflicts of interest.
杂志排行
Chinese Medical Sciences Journal的其它文章
- Research on the Antitumor Compounds from Cephalotaxus Hainanensis
- Artificial Musk R&D and Manufacturing
- Management of an Adult with Goodpasture’s Syndrome Following Brain Trauma with Extracorporeal Membrane Oxygenation: A Case Report
- Transvaginal Reduction of a Heterotopic Cornual Pregnancy with Conservation of Intrauterine Pregnancy
- Research Progress on Diagnosis and Treatment of Chronic Osteomyelitis
- Association between GSTT1 Homozygous Deletion and Risk of Pancreatic Cancer: A Meta Analysis