Transvaginal Reduction of a Heterotopic Cornual Pregnancy with Conservation of Intrauterine Pregnancy
2019-10-15YingyaLiLiyanDuanFengliChiKunmingLi
Yingya Li, Liyan Duan, Fengli Chi*, Kunming Li*
Center of Reproductive Medicine, Shanghai First Maternity and Infant Hospital,Tongji University School of Medicine, Shanghai 201204, China
Key words: heterotopic pregnancy; cornual pregnancy; in vitro fertilization; selective termination;assisted reproductive technique
Abstract Here we report a case of heterotopic cornual pregnancy after in vitro fertilization who was diagnosed at 6 weeks after frozen embryos transfer. The heterotopic pregnancy was successfully terminated by transvaginal ultrasound-guided selective fetal reduction. At 38+1 weeks, she underwent a cesarean section and delivered a healthy 3300 g male infant with Apgar score of 10-10’ evaluated at 1 min and 5 min.
HETEROTOPIC pregnancy (HP) is a scarce and lethal condition, which may cause massive hemorrhage and lead to hypovolemic shock, maternal mortality and fetal loss. It is defined as synchronous occurrence of both intrauterine and extrauterine pregnancy. The ectopic pregnancy could occur at various sites, such as fallopian tube, abdomen and uterine horn, etc.[1]The embryo implanting in the uterine horn is called cornual pregnancy and accounts for around 2% of ectopic pregnancies.[2]The incidence of heterotopic cornual pregnancy was estimated to be 1 in 3600 pregnancies conceived with assisted reproductive techniques (ART),[1]and it is much higher than that in spontaneous pregnancies.[3]Conventionally, three ways including non-surgical, surgical and expectant treatment are utilized for heterotopic cornual pregnancy management. Although surgical management is still prevalently used and shows good outcomes,[4,5]it may influence the intrauterine fetal development.[2]With the progress of ultrasound and minimally invasive techniques, embryos aspiration under ultrasound guidance has been carried out frequently to terminate extrauterine pregnancy, for their advantages of slighter stimulation to intrauterine gestation,[1,3]shorter operation time, more topical anesthesia and less invasion.[6]
Here, we present one case of heterotopic cornual pregnancy afterin vitrofertilization (IVF) with no symptoms who was diagnosed by ultrasound scan. The heterotopic cornual pregnancy was successfully treated with transvaginal ultrasound-guided embryo aspiration and the intrauterine pregnancy was conserved. The publication of this case report and attached images has obtained the written informed consent from the patient.
CASE DESCRIPTION
A 28-year-old gravida 1, para 0 woman had a history of polycystic ovarian syndrome and a right tubal pregnancy achieved after ovulation induction treatment, and was treated with right salpingectomy.Unfortunately, the latest hysterosalpingography showed that her left fallopian tube was partially obstructed. So she came to our hospital and received IVF treatment.
Controlled ovarian stimulation was achieved with a long gonadotropin-releasing hormone agonist protocol. The gonadotropin, a highly purified urinary follicle stimulating hormone (HP-uFSH) (Livzon Pharmaceutical Co. Ltd., China), was given for 11 days with a full dose of 1650 IU. Recombinant human luteinising hormone (r-hLH) (Merck Serono, Switzerland) at a dosage of 75 IU/d and recombinant human growth hormone(r-hGH) (Ankebio Co. Ltd., China) of 4 IU per day were administered for 7 days. After 36 h of recombinant human chorionic gonadotropin (r-hCG, 250 μg, i.h.)(Merck Serono, Switzerland) administration, the mature oocytes were retrieved using follicle aspiration under vaginal ultrasound guidance. Endometrial thickness assessed in the midsagittal planeviatransvaginal ultrasound was 5 mm on the day of hCG injection. It has been proved that endometrial thickness less than 7 mm would reduce the implantation rate and pregnancy rate,[8]thereby the fresh embryo transfer was not performed and all the embryos were cryopreserved.
During frozen embryo transfer cycle, 2 cryopreserved-thawed embryos (9/III, 8/II) were transferred on cycle day 17. Transvaginal sonography performed 4 weeks after the transfer revealed an intrauterine pregnancy with normal gestational sac and positive cardiac activity. Two weeks later, another gestational sac in the right uterine horn, having similar size to gestational sac seen in the intrauterine, with visible heartbeat,was identified (Figure 1). During this period, she had no complaints.

Figure 1. Transvaginal sonography performed after embryo transfer.
Two days later, she underwent transvaginal ultrasound guided selective fetal reduction of the cornual pregnancy. Briefly, a 16-gauge needle guided by an ultrasound system (Prosound 6, Hitachi Aloka Medical,Ltd., Japan) was advanced transvaginally into the ectopic gestational sac. Once the needle had been secured in place, about 5 ml fluid was aspirated from the embryonic vesicles and the fetal heart was punctured for three times until cardiac asystole was confirmed (Figure 2).After surgery, sonography scan showed the intrauterine pregnancy had normal cardiac activity. Serial Doppler ultrasound examinations over the next few weeks revealed gestational sac of the cornual pregnancy was getting smaller in size and blood flow was getting lower.Intrauterine pregnancy continued to develop normally. And she received cesarean section at 38+1 weeks’pregnancy and delivered a healthy 3300 g male infant with 10-10’ Apgar score at 1 min and 5 min. Some residual tissues located in the right uterine horn were removed surgically at the time of delivery.
DISCUSSION
Many factors such as previous ectopic pregnancy,a history of pelvic inflammatory disease, fallopian tube abnormality and pelvic surgery are considered to be a risk to heterotopic pregnancy.[1]For this case, a history of right tubal pregnancy and the partially obstructed left fallopian tube make her a high-risk group of heterotopic pregnancy.
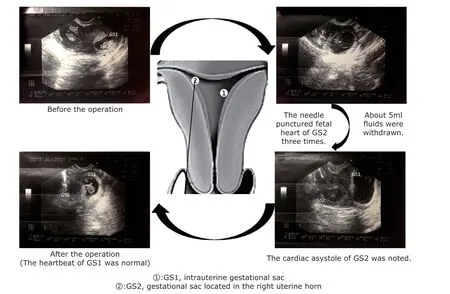
Figure 2. The transvaginal ultrasound-guided selective embryos aspiration of the cornual pregnancy.
Embryo implantation time and multiple embryos transfer has been proved to be concerned with ectopic pregnancy. Embryo implantation is a precisely synchronous interaction between the implantation embryo and the endometrium.[7]In general, anin vivofertilized embryo undergoes programmed division and differentiation to become a mature embryo at the blastocyst stage that is most suitable for implantation, during traveling a long distance in the oviduct and the uterine. However, anin vitrofertilized embryo is commonly transferred into the uterus at the early cleavage stage(4-8 cell stage) that is not the correct stage to implant.This asynchronism of embryo development and endometrial implantation window makes the embryo linger in the uterine cavity until the endometrium is ready for implantation, and the longer it takes, the higher incidence of ectopic pregnancy will occur.[8]
In order to increase the pregnancy rate, multiple embryo transfer was used in most IVF-embryo transfer (IVF-ET) cycles, which may also increase the incidence of heterotopic pregnancy. Therefore,patients receiving ART therapy should be monitored closely after the diagnosis of pregnancy. Currently in our center, conventional ultrasound is performed twice after the pregnancies are confirmed by a blood test. The examination is generally performed once for spontaneous pregnancy during first-trimester pregnancy. This is very meaningful, especially for patients who have no symptoms at an early stage.For this case, a coexisting ectopic gestational sac,which was similar to the intrauterine one in size, was not visualized on the initial ultrasound image, and was found 2 weeks later by ultrasonography. But the patient had no symptoms at all during this period. This condition may delay the diagnoses and treatment.Because heterotopic pregnancy is relatively rare and its clinical features are nonspecific, the frequency of misdiagnosis or delayed diagnosis is very high,[9]so the sonographers should be more conscientious and careful for those with high risk of heterotopic pregnancy.
In the past several years, surgical management has become the most common treatment option for heterotopic pregnancy and shows good outcomes.[10-13]However, surgical stimulation is more pronounced than non-surgical management and may affect the growth of the intrauterine fetus.[14]With the progress of ultrasound and minimally invasive techniques,these shortcomings can be overcome. Surboneet al.[2]revealed injecting potassium chloride, hypertonic solution or methotrexate directly into the ectopic gestational sac and selective embryo aspiration can improve the survival rate of the intrauterine pregnancy. Short operation time, topical anesthesia and minimal invasion can result in a better outcome and higher patient's acceptance. A retrospective study carried out in 2011 showed that ultrasoundguided embryo aspiration could successfully manage heterotopic cornual pregnancy.[6]The relevant case reports on account of technical difficulty were limited.Due to technical difficulties of surgery, the incidence of tubal rupture, hematoma formation and internal hemorrhage was higher.[15]Careful selection of patients(gestational week ≤8 weeks or embryo bud length between 5-13 mm) and follow-up are very important.[6]Meanwhile, the surgeon must be well trained.[6]For this case, the heterotopic cornual pregnancy was found at the 8th gestational week and she worried about the safety of intrauterine fetus. After careful evaluation,we confirmed she can be followed closely, treated her with transvaginal ultrasound-guided selective embryo aspiration and obtained a good pregnancy outcome.In addition, expectant management can be used if ultrasound examination can ensure that the fetus of the ectopic pregnancy has died and the patient has no symptoms.[16]
Overall, after managment of this case, we suggest embryos aspiration under ultrasound guidance is effective in treating heterotopic cornual pregnancy.The biggest difference between this case and the previously reported cases is that this patient had no complaints during the entire period and no ectopic gestational sac was observed in the initial ultrasound.These two features make this case easy to be missed or delayed diagnosis, which will lead to life-threatening consequences. Therefore, physicians and sonographers should pay more attention to pregnant women after ART treatments, especially for those with high risk of ectopic pregnancy.
Conflicts of interest statement
The authors have no conflicts of interest to disclose.
杂志排行
Chinese Medical Sciences Journal的其它文章
- Research on the Antitumor Compounds from Cephalotaxus Hainanensis
- Artificial Musk R&D and Manufacturing
- Management of an Adult with Goodpasture’s Syndrome Following Brain Trauma with Extracorporeal Membrane Oxygenation: A Case Report
- Research Progress on Diagnosis and Treatment of Chronic Osteomyelitis
- Association between GSTT1 Homozygous Deletion and Risk of Pancreatic Cancer: A Meta Analysis
- IL-36β Promotes Inflammatory Activity and Inhibits Differentiation of Keratinocytes In Vitro