Predictors of non-response to cardiac resynchronization therapy implantation in patients with class I indications: the markedly dilated left ventricular end-diastolic dimension and the presence of fragmented QRS
2019-08-19YiRanHUWeiHUAShengWenYANGMinGUHongXiaNIULiGangDINGJingWANGRanJINGXiaoHanFANShuZHANG
Yi-Ran HU, Wei HUA, Sheng-Wen YANG, Min GU, Hong-Xia NIU, Li-Gang DING, Jing WANG, Ran JING, Xiao-Han FAN, Shu ZHANG
State Key Labor atory of Car diovascular Disease, Arrhythmia Center, Fuwai Hospital;
National Center for Ca rdiovascular Diseases, Chinese A cademy of Medical Sciences and Peking Union Medical College, Beijing, China
Abstract Background Cardiac resynchronization therapy (CRT) is a highly effective treatment in patients with a class I recommendation. However, a small proportion of the strictly selected patients still fail to respond. This study was designed to identify predictors of non-response in patients with class I indications for CRT and determine the non-response probability of the patients. Methods A total of 296 consecutive patients with a class I recommendation received CRT from January 2009 to January 2017 were retrospectively analyzed. Multivariate logistic regression analysis was performed to identify predictors for non-response (defined as cardiac death, heart transplantation, or HF hospitalization during 1-year follow-up). Results Among 296 patients, 30 (10.1%) met non-response. Multivariate analysis demonstrated that non-response to CRT was associated with a fragmented QRS (odd ratio (OR) = 2.86, 95% CI: 1.14-7.12; P = 0.025) and left ventricular end-diastolic dimension (LVEDD) ≥ 77 mm (OR = 3.02, 95% CI: 1.17-7.82; P = 0.022). Patients with both of the predictors had a non-response probability of 46.2% (95% CI: 19.1%-73.3%). Conclusion In patients with left bundle branch block and wider QRS duration, the proportion of non-response to CRT is not low in real world. The presence of the dilated LVEDD or fragmented QRS is a strong predictor of non-response to CRT. The probability of non-response in the patients with the two predictors was 46.2%.
Keywords: Cardiac resynchronization therapy; Class I indication; Non-response; Predictors
1 Introduction
Cardiac resynchronization therapy (CRT) is an effective treatment modality for heart failure (HF) patients with reduced left ventricular ejection fraction (LVEF). It reduces morbidity and mortality in appropriately selected patients.[1,2]Current guidelines offer a class I recommendation for CRT implantation in symptomatic HF patients with LVEF ≤ 35%, left bundle branch block (LBBB) and wider QRS duration, despite at least three months of optimal medical therapy (OMT).[3,4]However, a small proportion of the strictly selected patients who underwent this this relatively expensive treatment still failed to derive benefit as a result of the so-called 'non-response'.[5,6]
Considering common pre-implant baseline parameters in addition to QRS duration and morphology may help further improve the overall benefit of CRT. To the best of our knowledge, factors that distinguish non-responders from eligible patients with a class I recommendation for the implantation remain unclear. Therefore, our research was aimed at identifying basic pre-implant clinical and echocardiographic parameters to predict non-response in patients with class I indications for CRT.
2 Methods
2.1 Study population and design
This was a single-center, retrospective observational study with 455 consecutive patients with reduced LVEF who successfully underwent CRT implantation in Arrhythmia Center of Fuwai Hospital (Beijing, China), between January 2009 and January 2017. This retrospective study was performed with written informed consent from all patients and approval from the ethics committee of Fuwai Hospital and in accordance with the Declaration of Helsinki. The indication for CRT implantation was based on the latest guidelines.[3,4]Patients with a class I recommendation for CRT (symptomatic HF, sinus rhythm, LVEF ≤ 35%, LBBB and QRS duration ≥ 130 ms, despite at least three months of OMT) were included. Patients were excluded if (1) they received CRT for pacemaker/defibrillator upgrade (class II recommendation); (2) their left ventricular (LV) lead position was neither in posterolateral/lateral cardiac veins nor in anterior cardiac veins; (3) they died of non-cardiac causes within 1-year follow-up; and (4) they were lost to 1-year follow-up. All patients received optimal medical therapy before and after implantation.
LV pacing leads were implanted transvenously through the coronary sinus, and preferably in lateral or posterolateral implant sites. After the implantation, atrioventricular delay optimization was programmed individually to reach the optimal diastolic filling through the Doppler mitral inflow before discharge. V-V delay ranged from 0 to 40 ms according to the standard of the shortest biventricular paced QRS duration. The patients were continually given the recommended OMT treatment when discharged.[4]After that, patients were required for examination at our hospital, typically after 3, 6 and 12 months during the first year and subsequently every 6-12 months if patients were normal. At each visit, devices were interrogated; echocardiography and laboratory tests were also performed. Among those patients who were tolerant of angiotensin-converting enzyme inhibitors (ACEIs)/angiotensin receptor blockers (ARBs)/β- block, they were given correspondingly increased doses, which tried to reach target doses.[4]All enrolled patients were followed up to January 2018. Baseline clinical data, including demographic characteristics, laboratory data and medications, were obtained from Fuwai Electronic Medical Record System.
During each visit, echocardiographic parameters including left atrial diameter (LAD), left ventricular end-diastolic dimension (LVEDD) and LVEF were routinely measured (Vivid E9, GE Healthcare, General Electric-Vingmed). LVEF was measured with the modified Simpson method and calculated from conventional apical two- and four- chamber images with the biplane Simpson technique. The degree of mitral regurgitation (MR) and tricuspid regurgitation (TR) was assessed semi-quantitatively in two classes (none/trivial/mild and moderate/severe).
At 1-year follow-up, patients were considered non-responders if they (1) died of cardiac causes, (2) underwent heart transplantation, or (3) HF hospitalization.
Among all the patients, the history of HF was defined as the interval between first hospitalization for HF (or first detection of LV dysfunction) and CRT implantation. LBBB was defined as QRS duration ≥ 120 ms, monophasic QS or rS complex in lead V1, and monophasic R wave with no Q waves in lead V6.[7]Fragmented QRS with bundle branch block (BBB) morphology was defined as the presence of > 2 notches (at least 1 notch more than the typical BBB) or multiple notches of the R wave, or > 2 notches in the nadir of the S wave recorded in ≥ 2 contiguous leads in 12-lead ECG (Figure 1).[8]Frequent premature ventricular contractions (PVCs) were defined as the presence of over 1000 PVCs recorded by 24-h Holter monitoring.[9]

Figure 1. Example of fragmented QRS of a patient with LBBB. Arrows denote fragmented QRS. LBBB: left branch bundle block.
Based on the obtained significant predictors, receiver- operating characteristic curve (ROC) analysis with the Youden index was used to define the optimum cut-off values of the QRS duration, LVEF, LAD and LVEDD for non-response prediction at 1-year follow-up.
2.2 Statistical analysis
SPSS 22.0 statistical software (SPSS, Inc, IBM, Armonk, New York) was used for statistical analysis. The mean ± SD were used as the descriptive statistics for continuous variables, and numbers and percentage for categorical variables. Significant continuous variables were transformed to binary variables using cut-off values. Optimum cut-off values were identified through ROC curves with Youden index. Group comparisons were carried out through the Student t test or Mann-Whitney U test for continuous variables and chi-square test or Fisher's exact test for categorical variables. Changes in variables from baseline to 1-year follow-up in each group were compared using paired Student t test. Univariate and multivariate logistic regression analysis were performed to examine for significant predictors of non-response. The factors with P values < 0.05 in the univariate analysis were entered into a multivariate logistic regression model with a forward stepwise method to identify the independent predictors of non-response. The accuracy of the model was verified with the Hosmer-Lemeshow test. A two-sided P-value < 0.05 was considered statistically significant.
3 Results
A total of 328 patients with sinus rhythm, LVEF ≤ 35%, LBBB and QRS duration ≥ 130 ms (class I indications) successfully underwent CRT implantation in our study. Among them, 32 were excluded (13 LV lead position were ineligible; 4 died of non-cardiac death causes within 1-year follow-up; 15 lost 1-year follow-up). As a result, the remaining 296 patients were included in the final analysis, and 30 (10.1%) of them met non-response (11 died of cardiac death, 2 underwent heart transplant and 17 had HF hospitalization). The study flow diagram is shown in Figure 2.
Baseline characteristics of non-responders and responders are summarized in Table 1. In brief, there was no significant difference in most of the clinical characteristics among the two groups. Neither were the proportions of OMT among the two groups. However, a lower percentage of non-responders (16.7%) than in responders (43.2%) were present in females. Compared with the latter, non-responders more likely had Fragmented QRS and wider QRS duration. They also had lower LVEF, larger LVEDD and LAD than responders.
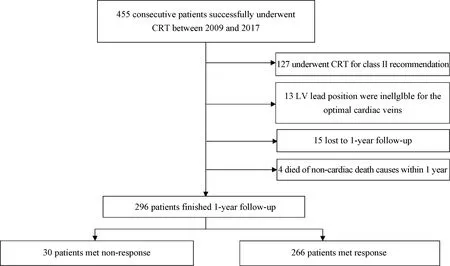
Figure 2. Flow diagram of included subjects. CRT: cardiac resynchronization therapy; LV: left ventricular.
The comparison of echocardiographic parameters between non-responders and responders was illustrated in Figure 3. After 1-year follow-up, among CRT non-responders, changes in LVEF (24.5% ± 3.7% vs. 26.2% ± 4.0%; P = 0.124) and LVEDD (76.8% ± 6.3% vs. 75.3% ± 7.3%; P = 0.241) are not very noticeable. On the contrary, responders to CRT manifested a significant improvement in LVEF (27.4% ± 5.2% vs. 42.5% ± 10.4%, P < 0.001). This increase was associated with a significant decrease in LVEDD (70.3 ± 9.1 vs. 61.8 ± 10.3 mm, P < 0.001). Besides, changes of LVEF and LVEDD from baseline to follow-up were significantly greater in responders than in non-responders (P < 0.001).

Table 1. Baseline characteristics according to CRT response.
The ROC was used to determine a cut-off of 4 significantly continuous variables as a categorical predictor for non-response. As shown in Figure 4, the area under the receiver-operating characteristic curve (AUC) for the QRS duration before CRT implantation was 0.69 and a cut-off value of 174 ms had a sensitivity of 63.3% and a specificity of 66.5% for non-response prediction. Accordingly, AUC for the three echocardiographic parameters—LVEF, LAD and LVEDD before CRT implantation were 0.64, 0.67 and 0.71 respectively; the sensitivity of a 26.5%, 42.5 mm and 76.5 mm cut-off value for LVEF, LAD and LVEDD was 53.3%, 70.0% and 53.3% respectively and the specificity of the same sequence was at 59.8%, 59.0% and 77.8%, respectively for non-response prediction.
Multiple logistic regression analysis revealed two factors as independent predictors for non-response to CRT at the 1-year follow-up: fragmented QRS [odd ratio (OR) = 2.86, 95% CI: 1.14-7.12; P = 0.025)] and LVEDD ≥ 77 mm (OR = 3.02,95% CI: 1.17-7.82; P = 0.022) as shown in Table 2. The accuracy of the model was confirmed by the Hosmer-Lemeshow test (P = 0.815). If neither of the two predicators was present in a patient with LBBB and wider QRS duration, the probability of non-response to CRT would be only about 4%. If either the fragmented QRS or the dilated LVEDD was present in the same patient, the probability of non-response would be 14% to 17%. More important, if both of the predictors surfaced in the same patient, the probability of non-response would reach nearly 50% according to our model. Table 3 summarizes the probabilities of non-response predicted by the regression model.
4 Discussion
The major findings of our study were as follows: (1) the proportion of non-responders was still relatively high in real world despite the fact that patients were selected according to a class I recommendation for CRT (LVEF ≤ 35%, LBBB and QRS duration ≥ 130 ms) and successfully underwent the implantation. According to our definition of non-response to CRT, there were 10.1% non-responders in our single center. (2) Multivariate logistic analysis showed that non-response to CRT was associated with a fragmented QRS by electrocardiogram and a dilated LVEDD by echocardiography at baseline. According to our model, if a patient with LBBB and wider QRS duration did not have fragmented QRS and dilated LVEDD, the probability of non-response to CRT would be less than 5%. However, if the same patient had both of the two predictors mentioned above, the probability of non-response to CRT would be over 45%. Therefore, clear detection of non-responders to CRT and further identification of eligible patients are required. This is conducive to improve the overall response rate to this relatively expensive device, make full use of medical and financial resources, especially for those developing countries like China.

Figure 3. Changes in echocardiographic parameters during follow-up. (A): LVEF at last follow-up (P < 0.001), and change from baseline to 1-year follow-up (P < 0.001) were all significantly greater in responders than non-responders; and (B): LVEDD at last follow-up (P < 0.001), and change from baseline to 1-year follow-up (P < 0.001) were all significantly greater in responders than non-responders. In the non-responder group, 13 patients who died or underwent heart transplantation during 1-year follow-up are excluded. CRT: cardiac resynchronization therapy; LVEDD: left ventricular end-diastolic dimension; LVEF: left ventricular ejection fraction.

Figure 4. Receiver-operating characteristic curves of continuous variables predicting non-response. (A): Receiver-operating characteristic curve of QRS duration; (B): receiver-operating characteristic curve of LVEF; (C): receiver-operating characteristic curve of LAD; and (D): receiver-operating characteristic curve of LVEDD. AUC: area under the receiver-operating characteristic curve; CRT: cardiac resynchronization therapy; LAD: left atrial diameter; LVEDD: left ventricular end-diastolic dimension; LVEF: left ventricular ejection fraction.

Table 2. Predictors of non-response to CRT, uni- and multivariate Logistic regression models.

Table 3. Predicted value of probability of non-responding to CRT during follow-up.
Currently, guidelines emphasize QRS morphology and duration which serves as main criteria before CRT implantation.[3,4]Bleeker, et al.[10]prospectively incorporated patients with LBBB, wider QRS duration and LVEF ≤ 35% and evaluated the posterolateral scar tissue with contrast- enhanced magnetic resonance imaging (MRI). They found that patients with scar in posterolateral area were of a low response rate to CRT. Besides, a meta-analysis also showed that among patients with QRS duration 130-149 ms, the males failed to benefit from CRT.[11]Thus, there exist limitations for the ECG indicator alone as the criteria to achieve proper selection of CRT candidates.[12]Taking other baseline parameters into consideration, it is necessary to comprehensively evaluate individual response to CRT before implantation, so as to reduce the rate of non-response and improve the overall benefits from the treatment. In our study, we identified two independent predictors of non-response to CRT based on the patients in China's largest single center. Our findings suggest that, despite a class I recommendation for CRT in patients with LBBB and wider QRS duration, checking for fragmented QRS and (or) LVEDD before CRT implantation is required for those who are elderly, have financial issues or suffer from severe organic diseases (such as chronic kidney disease). Clinical decisions should be made on a cost-effective basis.
Echocardiographic measures of reverse remodeling were often employed to assess CRT response in previous studies, only a few used cardiac death or heart transplantation to define non-response to CRT.[6]Goldenberg, et al.[13]proposed a CRT response score from MADIT-CRT population and identified seven factors (male sex, ischemic cardiomyopathy, QRS duration < 150 ms, non-LBBB, baseline left ventricular end-diastolic volume < 125 mL/m2and baseline left atrial volume ≥ 40 mL/m2) associated with low echocardiographic response. Patients in the first response score quartile did not derive a significant reduction in the risk of heart failure or death. Kydd, et al.[14]created a multi- parametric score (defined as the anticipated probability of response to CRT) which offered potential to predict non- response to CRT. In spite of these meaningful results, several technical problems still stand in the way of measuring reverse remodeling.[5]For example, a relatively large inter-observer variability surfaces when 2-dimensional echocardiography is used to assess LV volume and LVEF. Therefore, event-based measures are more suitable for evaluating the effects of CRT on prognosis.[6]Díaz-Infant, et al.[15]defined non-responders if patients (1) died of heart failure, (2) underwent heart transplantation, or (3) did not increase the walking distance in 6 minutes by > 10%. They found that ischemic heart disease, severe MR and LVEDD ≥ 75 mm were the independent predictors of non-response to CRT. Patients with these three factors only had a probability response of 27%. However, enrolled patients in their study included patients with permanent AF (class II recommendation for CRT).[4]To the best of our knowledge, there is no prior research focusing on predictors of non-response to CRT in patients who had a class I recommendation for this therapy. Our study drew on hard clinical endpoints (death, heart transplantation and HF hospitalization) for the definition of CRT non-response. The endpoints are more effective than echocardiographic parameters in evaluation of the therapeutic effects on especially patients of class I indications.
Of the two independent predictors of non-response identified, fQRS results from myocardial scarring or cardiac fibrosis and can cause heterogeneous ventricular activation and systolic dyssynchrony in patients with ischemic or non- ischemic cardiomyopathy.[8,16]Prior studies have indicated that presence of fQRS and more leads on ECG with fQRS were associated with non-response to CRT.[17,18]In terms of LVEDD, dilated LVEDD may be a signal of a more advanced cardiac disease and a marker of an uneasily reversible cardiac pathologic condition.[19]Non-responders had a wider LVEDD than responders in other studies of CRT.[15,20]Consistent with these former studies, our findings showed that the presence of fQRS on baseline ECG and LVEDD ≥ 77 mm on baseline echocardiogram was an independent predictor of non-response to CRT. According to our results, we may suggest that fQRS and LVEDD remain simple standard electrocardiographic and echocardiographic measurements that are routinely reported in clinical practice and that can provide immediate clinical guidance in predicting non-response to CRT. Besides, it should be noted that young physicians tend to mistakenly regard true-LBBB (defined as conventional LBBB plus QRS duration ≥ 130 ms and mid- QRS notching/slurring in at least two of the leads I, aVL, V1, V2, V5, or V6) as fQRS because notches on the R/S wave on ECG are easily misjudged.[20]Notably, instead of being true-LBBB for predicting super-response, fQRS shows the opposite result in response prediction.[18,20]
With regard to other predictive factors for non-response to CRT, such as ischemic origin of cardiomyopathy[15]and broadly wider QRS duration[21]multivariate analysis did not show significant difference in our study. According to similar studies, non-ischemic cardiomyopathy was more commonly seen in patients from Asia.[20,22]In our study, non-ischemic cardiomyopathy was present in 81.4% of our study population. Thus, the enrolled patients may be a potential explanation for the absence of statistical difference in this predictive factor. In respect to QRS duration, previous studies have demonstrated that patients with a wider QRS duration are more likely to respond to CRT.[5,23]Yet, a recent study by Sassone, et al.[21]showed that patients with LBBB and QRS duration ≥ 178 ms on baseline ECG had worse echocardiographic response to CRT. They speculated that a marked QRS duration widening reflected the presence of a severe LV mechanical dyssynchrony unamenable to resynchronization by biventricular pacing. Our results did not reveal much significance of QRS duration, which might be attributed to the difference in definition of non-response to CRT.
OMT plays a significant part in stabilizing the disease progression and improving the prognosis in spite of HF patients undergoing CRT.[24]However, only a small proportion of CRT patients were on the target doses recommended by the guidelines in clinical practice.[4]According to ESC Heart Failure Long-Term Registry, including patients with CRT implantation, the target dosage of ACEI, ARB and BBs were used merely in 29.3%, 24.1% and 17.5% of patients with heart failure, respectively.[25]Besides, from China-HF, the use of ACEIs/ARBs and β-block in patients with HF was only 67.5% and 70.0%, respectively.[26]Treatment of OMT should be followed by gradually increasing dose on the condition that CRT patients were tolerate with them, which could, to a large extent, ensure further improvement in CRT response rate.
There are several limitations in our study. Firstly, this was a retrospective and single-center study that only took baseline clinical and echocardiographic variables into account. The level of serum biomarkers (N-terminal pro-brain natriuretic peptide, Creatinine, et al.) related to outcomes were usually influenced by metabolism from many organs and thus excluded from the Logistic analysis. Though possible variables for effects on prognosis were incorporated in our final multivariate analysis to undermine the influence of confounding factors, unknown confounding factors were not considered and thence could not be excluded from this study. Secondly, data on late gadolinium enhancement with T1 mapping was not utilized due to insufficient data volume, although MRI is currently considered as the gold standard for assessment of myocardial fibrosis and scar.[4]Besides, there is also a lack in estimating left/biv ventricular dyssynchrony by echocardiography. Finally, among the CRT patients receiving OMT in our study, there is only a small proportion of them on target doses, which may increase the non-response rate to CRT.
In conclusion, In HF patients with LBBB and wider QRS duration, the proportion of non-response to CRT is not low in real world. CRT non-responders had poorer clinical outcome in comparison with the responders. The presence of the dilated LVEDD or fragmented QRS is a strong predictor of non-response to CRT. The probability of non-response in the patients with the two predictors was 46.2%.
Acknowledgements
This study was financially supported by the National Natural Science Foundation of China (81570370) and CAMS Innovation Fund for Medical Sciences (2017-I2M-1-009). The author declares that there has no conflict of interest.
杂志排行
Journal of Geriatric Cardiology的其它文章
- The utility of coronary computed tomography angiography in elderly patients
- The relevance of serum albumin among elderly patients with acute decompensated heart failure
- The value of serum metabolomics analysis in predicting the response to cardiac resynchronization therapy
- Effects of febuxostat on atrial remodeling in a rabbit model of atrial fibrillation induced by rapid atrial pacing
- Adverse reactions of Amiodarone
- Approach to a patient with cardiac amyloidosis
