The utility of coronary computed tomography angiography in elderly patients
2019-08-19JordanLaggouneNiteshNerlekarKiranMunnurBrianSHKoJamesCameronSujithSeneviratneDennisTLWong
Jordan Laggoune, Nitesh Nerlekar, Kiran Munnur, Brian SH Ko, James D Cameron, Sujith Seneviratne, Dennis TL Wong,2,#
1Monash Cardiovascular Research Centre, Monash University and MonashHeart, Monash Health, Clayton, Victoria, Australia
2South Australian Health Medical Research Institute, Adelaide, Australia
Abstract Background Coronary computed tomography angiography (CCTA) is often avoided in elderly patients due to a presumption that a high proportion of patients will have heavily calcified plaque limiting an accurate assessment. We sought to assess the image quality, luminal stenosis and utility of CCTA in elderly patients with suspected coronary artery disease (CAD) and stable chest pain. Methods Retrospective analysis of elderly patients (> 75 years) who underwent 320-detector row CCTA between 2012-2017 at MonashHeart. The CCTA was analysed for degree maximal coronary stenosis by CAD-RADS classification, image quality by a 5-point Likert score (1-poor, 2-adequate, 3-good, 4-very good, 5-excellent) and presence of artefact limiting interpretability. Results 1011 elderly patients (62% females, 78.8 ± 3.3 years) were studied. Cardiovascular risk factor prevalence included: hypertension (65%), hyperlipidaemia (48%), diabetes (19%) and smoking (21%). The CCTA was evaluable in 68% of patients which included 52% with non-obstructive CAD (< 50% stenosis), 48% with obstructive CAD (> 50%) stenosis. Mean Likert score was 3.1 ± 0.6 corresponding to good image quality. Of the 323 (32%) of patients with a non-interpretable CCTA, 80% were due to calcified plaque and 20% due to motion artefact. Male gender (P = 0.009), age (P = 0.02), excess motion (P < 0.01) and diabetes mellitus (P = 0.03) were associated with non-interpretable CCTA. Conclusion Although CCTA is a feasible non-invasive tool for assessment of elderly patients with stable chest pain, clinicians should still be cautious about referring elderly patients for CCTA. Patients who are male, diabetic and >78 years of age are significantly less likely to have interpretable scans.
Keywords: Coronary artery calcium; Coronary CT angiography; Multi-detector row CT; The elderly #Correspondence to: Dennis TL Wong, Monash Cardiovascular Research Centre, MonashHeart, Monash Medical Centre, 246 Clayton Road, Clayton, Melbourne, VIC 3168, Australia. E-mail: drdenniswong@yahoo.com.au Telephone: +61-3-95942726 Fax: +61-3-9594 6939 Received: June 24, 2019 Revised: June 25, 2019 Accepted: July 26, 2019 Published online: July 28, 2019
1 Introduction
Coronary computed tomography angiography (CCTA) is an effective tool for the assessment of patients with suspected coronary artery disease (CAD). This is due to its high sensitivity and negative predictive value in identifying non-obstructive CAD. Current guidelines recommend utilising CCTA as a first-line modality of assessment in patients with stable chest pain and a low-intermediate risk or pre-test probability for CAD.[1-3]There is however minimal data that has investigated the utility of CCTA in elderly patients. Previous small-scale studies assessing the utility of CCTA in elderly patients have indicated that it is a feasible and accurate method of assessment.[4-7]Despite this, there is still some reticence for clinicians to refer patients for CCTA due to the possible presence of excessive calcification and heavy atherosclerotic plaque burden that could preclude an effective diagnostic assessment.
Current guidelines do not define an age threshold at which a CCTA should not be performed,[1-3]but recommend that the clinician take into consideration the demographics and pathology of the patient when referring for a CCTA. This, in combination with a lack of evidence demonstrating the utility and efficacy of CCTA in the elderly may contribute to the lack of CCTA being frequently performed in the elderly population. The aim of this study was to evaluate the utility of CCTA in low-intermediate risk patients ≥ 75 years of age, with suspected CAD. We also sought to assess any factors associated with non-interpretable CCTA in elderly patients.
2 Methods
This was a single-site, retrospective, observational study, designed to investigate the utility of CCTA in patients ≥ 75 years of age (Figure 1). Patients were eligible for the study if they were (1) ≥ 75 years of age at the time of the CCTA, (2) referred for a CCTA with stable chest pain. Patients who were referred for a non-coronary CT, previous history of coronary artery bypass graft surgery and atrial fibrillation were excluded from the study.
2.1 CCTA protocol
All CCTAs were performed on a 320 detector CT (Toshiba Aquilion One, Toshiba Medical Systems, Tokyo, Japan) using previously published department protocols.[8]The IV contrast injection protocol involved a 2-phase injection: the contrast amount varied according to patient size using 1 mL/kg of IV contrast. Contrast injection rate also varied according to contrast amount allowing an injection time of 11-13 s. For the scan acquisition, the volume acquisition used up to 320 Z-axis detectors, Z axis coverage varied according to heart size which was determined using a low dose planning scan from carina to below heart. For heart rates below 65 beats/min, prospective gating using 10% padding centred on 75% R-R interval was utilised. For heart rates above 65 beats/min, prospective gating covering from 30%-80% R-R interval was utilised. The process for image reconstruction was to acquire slice thickness and interval of 0.5 mm slices every 0.25 mm, using reconstruction algorithm: FC43 (angiogram soft tissue), iterative process: AIDR3D enhanced, Initial reconstructed cardiac phase: 75% R-R, Scan FOV: 350 mm. Additional reconstructions were used if cardiac motion is seen on the original 75% phase additional cardiac phases are reconstructed using Cardio Image Exact. Oral and/or intravenous beta-blockers were administered to achieve a pre-CCTA scan heart rate below 60 beats/minute. Sublingual nitroglycerin (400 μg) was routinely given prior to the scan, as well as other adjunctive medication where indicated.

Figure 1. Study flow chart. CAD: coronary artery disease; CCTA: coronary computed tomography angiography; ITP: interpretability; NITP: non-interpretability.
2.2 CCTA analysis
CCTA were interpreted by two experienced CCTA clinicians (level B). The CCTA clinicians read independently of each other, and discrepant findings were reconciled by consensus. The image quality of CCTA was determined by the 5-point Likert scale: 1 = poor, 2 = adequate, 3 = good, 4 = very good and 5 = excellent. We defined CCTA to be interpretable (ITP) if all coronary vessels were clearly imaged and conclusive luminal stenosis assessment was able to be performed. CCTA was classified as non-interpretable (NIPT) if all coronary vessels were not clearly imaged and/or if there was inconclusive luminal stenosis assessment in any segment.
Reasons for NITP CCTA including coronary artery calcium (CAC), motion artefact, acquisition heart rate, poor contrast opacification and metal artefact were recorded. The degree of luminal stenosis was graded according to SCCT grading scale of 0 = no visible stenosis, 1%-24% = Minimal stenosis, 25%-49% = mild stenosis, 50%-69% = moderate stenosis, 70%-99% = severe stenosis and 100% = occluded. Each patient was then assigned a CAD-RADS (Table 1) classification based on the highest degree of luminal stenosis observed.[9]Patients with CAD-RADS classification of 0-2 were classified as non-obstructive CAD while patients with CAD-RADS classification of ≥ 3 were classified as obstructive CAD. Where segments containing heavy calcification were apparent that precluded an accurate assessment, a default CAD-RADS score of 3 was used to denote a level of stenosis no less than 50% or moderate, unless there was a greater level or stenosis such as; severe or greater clearly identified by the reader.
2.3 Statistical analysis
Data are presented as mean ± SD, or as frequencies and percentages as appropriate and compared with t-test or chi-squared test as appropriate. Binary logistic regression with non-interpretability as an outcome was performed at a univariable level, and further multivariable regression performed with covariates with a univariate P < 0.20. Estimates are reported as odds ratios (OR) with 95% confidence intervals. A two-sided P-value of < 0.05 was statistically significant, and all analysis was performed using Stata MP/14.0 (StataCorp, College Station, TX).
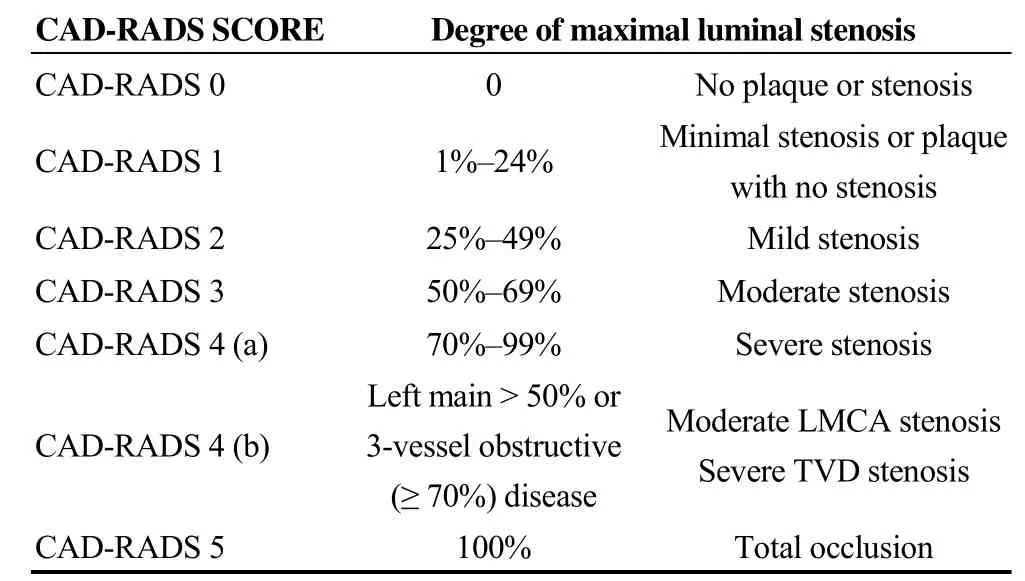
Table 1. CAD-RADS reporting and data system for patients presenting with stable chest pain.
3 Results
3.1 Clinical characteristics
A total of 1724 patients > 75 years of age referred for CCTA between 2012 and 2017 at MonashHeart for suspected coronary artery disease were screened, and 1011 patients met study inclusion criteria (Figure 1). The mean age of patients was 78 ± 3.3 years (range 75-91 years). Patient characteristics are summarised in Table 2. The mean estimated effective radiation dose in our study was 4.4 mSv. Detailed CT scan parameters are summarised in Table 3.

Table 2. Baseline characteristics (n = 1015 ).

Table 3. CCTA scan parameters.
There were 688 (68%) patients with an interpretable (ITP) CCTA. Mean Likert score was 3.1 ± 0.6 corresponding to good image quality. Coronary calcification (254 patients, 80%) was the most common cause of NITP CCTA. Motion artefact was present in 64 patients (20%). The mean heart rate (65 ± 7 beats/min) of patients with motion artefact was higher than the overall cohort 56 ± 8.6 beats/min (P < 0.01). There were two patients with non-interpretable studies due to pacemaker lead artefact and poor contrast opacification (Table 4). In the NIPT cohort (323 patients, 32%), significant CAD (≥ 50% stenosis) could not be excluded due to CAC in 257 (80%) patients.
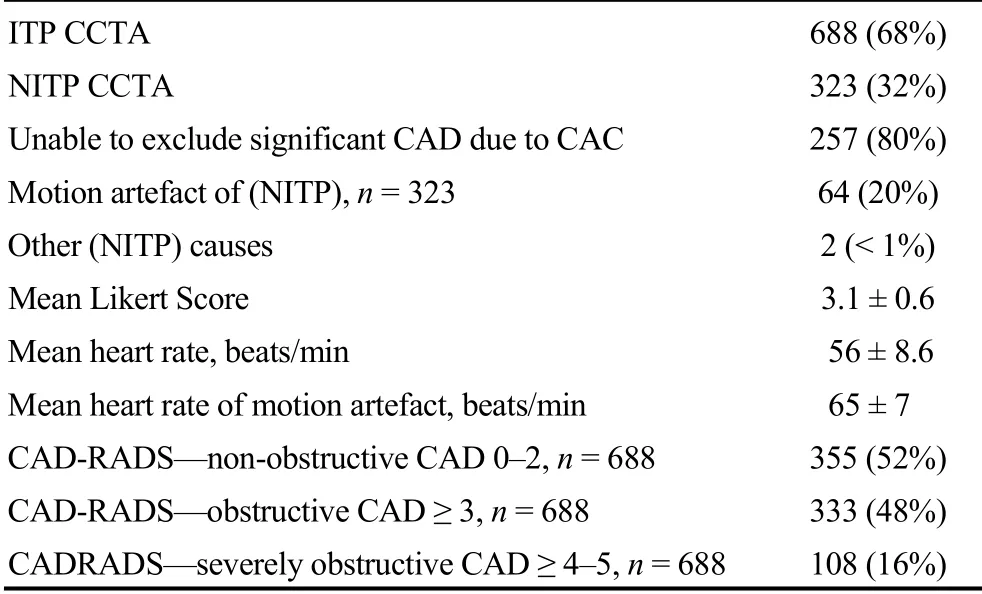
Table 4. Results of interpretability.
In the ITP group, 355 patients (52%) had non-obstructive CAD (CAD-RADS ≤ 2), 333 patients (48%) had obstructive CAD (CAD-RADS ≥ 3) and 108 patients (16%) had severe obstructive CAD (CAD-RADS score ≥ 4-5/>70% stenosis, left main disease > 50%, triple vessel disease > 70%). The degree of CAD in the NITP group were not assessed, as not all coronary vessels could not be imaged, and therefore would represent a disproportionate result compared to the ITP group, where all coronary vessels were effectively imaged and assessed.
3.2 Predictors of non-interpretability
On univariate analysis, of all the traditional cardiovascular risk factors (Figure 2), only diabetes mellitus (OR: 1.54, 95% CI: 1.11-2.14; P = 0.01) was a predictor of NITP. Hypertension, hyperlipidaemia and smoking were not associated with NITP. Male gender (OR: 0.74; 95% CI: 0.56-0.96; P = 0.03) and age (OR: 1.05; 95% CI: 1.01-1.09; P = 0.02) were also associated with NITP (Table 5). Increasing age was associated with an increased probability of NITP (Figure 3). Receiver operator characteristic analysis predicted that a cut-off age of 78 years was associated with sensitivity of 62% and specificity of 45% to predict NITP. Heart rate at the time of CCTA scan was also a predictor or NITP (OR: 1.04, 95% CI: 1.02-1.06, P < 0.01). In particular heart rate > 60 beats/min was a strong predictor of NITP with an odds ratio of 2.06 (95% CI: 1.56-2.73). On multivariate analysis, age, male gender, heart rate > 60 beats/min and
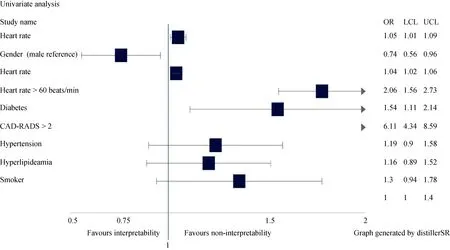
Figure 2. Forest plot of univariate analysis. LCL: lower control limit; UCL: upper control limit.

Table 5. Predictors of non-interpretability.
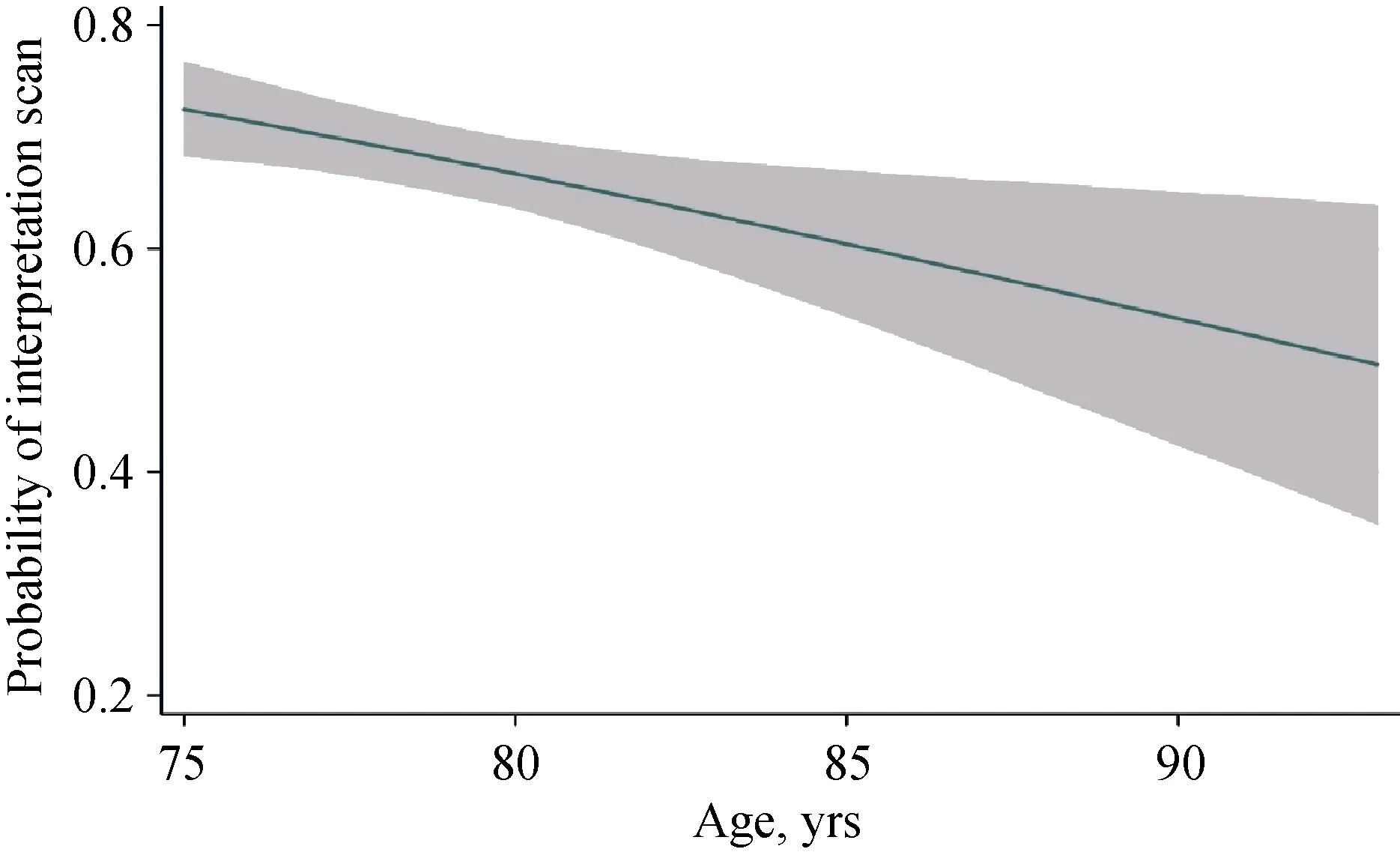
Figure 3. Age and non-interpretability.diabetes mellitus remained significant predictors of NITP (Table 5).
3.3 Cardiac catheterisation and revascularisation
Within the 1011 eligible study patients, 207 patients (20%) underwent invasive (ICA) coronary angiography within a 6-month period of their initial CCTA. Of these 93 patients (45%), 74 patients (80%) underwent percutaneous coronary intervention (PCI) while 19 patients (20%) underwent coronary artery bypass surgery (CABG) (Table 6).

Table 6. Invasive angiography vs. coronary CT.
4 Discussion
The current study demonstrates that the majority (68%) of elderly patients with suspected stable coronary artery disease referred for CCTA have scan results that are interpretable and diagnostic. Furthermore, we also show that patients who are male, diabetic, and > 78 years of age are significantly less likely to have interpretable scans. Lastly, high resting heart rate also predicts non-interpretable CCTA in elderly patients.
CCTA is widely used and recommended for assessing suspected CAD in low-intermediate risk patients with stable chest pain.[1-3]This recommendation stems from the high sensitivity and negative predictive value of CCTA for the detection of coronary artery stenosis.[10-12]The advancement of multi-detector row CT scanners has led to improvement in spatial and temporal imaging of coronary arteries at lower radiation dose. Consequently, the recent PROMISE trial had demonstrated that CCTA can improve diagnostic certainty, and is non-inferior to functional assessment.[13]Despite this, there is often reluctance amongst clinicians to select this modality for elderly patients due to perception that images are likely to be non-diagnostic due to the possible presence of excessive calcification and heavy atherosclerotic plaque burden. Sun, et al.[14]have previous demonstrated that the percentage of patients with significant coronary artery stenosis reached 38% in patients aged over 65 years compared to less than 15% in patients under 56 years. Thus far, there have only been a few small studies which have assessed the utility of CCTA in elderly patients and have indicated that it is a feasible and accurate method of assessment.[4-7]
The focus of this study was to determine the feasibility and utility of CCTA in elderly patient's ≥ 75 years of age, with stable chest pain and a low-intermediate risk profile. We showed that 68% of CCTAs were fully interpretable. What is also of significance is that of the 688 patients with a fully interpretable CTA, more than half (52%) demonstrated non-obstructive CAD. The importance of this, is that despite the patients advanced age, the utility of CCTA within the cohort of this study was still able to effectively identify and exclude obstructive CAD. Despite the use of a 320-detector row scanner which requires shorter breath hold, single beat imaging and an average heart of 56 beats/min at acquisition, 32% of scans were not interpretable in this study. Moreover, in the NITP group, only 20% were due to preventable factors such as motion while 80% were due to excessive calcification. Therefore, although the study did demonstrate a possible utility of CCTA in the elderly population, larger, prospective, randomised, multi-centre trials that compare the utility of CCTA versus invasive or functional testing would be required to confirm CCTA as a reliable alternative in the evaluation of elderly patients with stable chest pain.
Evidently, functional studies can demonstrate the functional capacity and coronary ischemia compared with CCTA, as was shown in the PROMISE trial.[13]CCTA on the other hand is able to identify plaque features, which are strongly associated with patient outcomes regardless of functional capacity.[15]Additionally, there is minimal evidence that currently exists in elderly populations regarding the application of functional capacity and preventive medications, and as life expectancies continue to rise the initial results of this study may further our understanding towards to an increased utility and application of CCTA in the elderly.
CCTA may demonstrate some inherent benefits compared with other methods of coronary assessment, but CCTA is not without its drawbacks. Specifically, the acute effect of contrast admiration on renal function, as well as the progressive deterioration of renal function with age. Both these factors need to be considered when considering the application of CCTA in elderly groups.
The increased incidence of atrial fibrillation is also a factor that could limit the application and efficacy of CCTA in a cohort with advancing age. As with increasing heart rates, there is also the greater possibility of non-interpretable scan due to a higher signal to noise ratio. This study didn't assess the utility of CCTA in patients with atrial fibrillation, therefore this would need to be investigated further before any definitive conclusions are made on what impact atrial fibrillation has on the utility of CCTA.
While there is a demonstrable utility for CCTA in the elderly, there remains issues that can affect the interpretability of the CTA. The heart rate control of the patients remains a critical factor. We showed that resting heart rate had a significant association with NITP. It is therefore imperative to control the resting heart rate to < 60 beats/min with oral and/or intravenous metoprolol. The mean heart rate in our study was low 56 ± 8.6 beats/min and this is partly contributed by the high usage (76%) of oral metoprolol.
This study also showed that age, male gender and diabetes mellitus were associated with a non-interpretable CCTA. As shown in Figure 5, advancing age increases the probability of non-interpretable CCTA. It appears that subjects over 78 years of age would be much more likely to demonstrate a NITP versus those subjects < 78 years of age. A probable explanation for this is the correlation between increasing age and plaque burden. The incidence of CAD in males compared to women has been widely researched and reported, and recent evidence suggested that CAD develops 7-10 years earlier in men than women.[16]As well as an earlier onset of CAD, men also demonstrate a significantly higher burden of coronary artery plaque.[17-19]
As reported, diabetes mellitus showed a significant association with NITP. The most probable cause of this is the strong correlation of diabetes and CAC. Wong, et al.,[17]observed that the incidence of CAC (per 100 person years) was 13.9% versus 6.2% in non-diabetic males. As CAC made up 80% of the causes of NITP in this study, it further supports the notion that diabetes is a significant predictor of NITP, and a CCTA should where possible be avoided in this demographic in favour of functional testing or ICA.
4.1 Limitations
This study was a single-site, retrospective observational study and therefore caution needs to be used when considering the impact of these results across a broader spectrum of both population and clinical practice. All scans in this study were performed on a 320-detector row CT which requires much shorter breath hold than 64-detector row CT. As breath holding may be problematic in elderly patients, our results cannot be generalised to all CT scanners. There was a degree of referral bias as the subjects were initially referred for a CCTA by their own physician. Additionally, the investigators of this study determined the minimum age for inclusion would be 75 years of age; based on current evidence, although it should be reiterated that all consecutive patients of MonashHeart over the age of 75 years of age, referred for a CCTA with stable chest pain between 2012 and 2017 were considered for analysis. While this study has discussed some of the issues that were associated with non-interpretable CCTA's, this is by no means a conclusive list, further investigation needs to be directed towards understanding the possible correlation between burden of coronary artery calcium score and non-interpretable CCTA. This was not performed as part of this study, as there was only a small percentage of the population that underwent calcium scoring as part of their CCTA. Additionally, further investigation is required to ascertain the extent to which subject's cardiovascular risk factors are managed and the during that each subject has been exposed to a specific risk factor, as this was not included in the analysis and could influence results.
4.2 Conclusion
Although CCTA is a feasible non-invasive tool for assessment of elderly patients with stable chest pain, clinicians should still be cautious about referring elderly patients for CCTA. Patients who are male, diabetic and > 78 years of age are significantly less likely to have interpretable scans.
Acknowledgements
Dr. Brian SH Ko has received speaking fees from Canon Medical.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Predictors of non-response to cardiac resynchronization therapy implantation in patients with class I indications: the markedly dilated left ventricular end-diastolic dimension and the presence of fragmented QRS
- The relevance of serum albumin among elderly patients with acute decompensated heart failure
- The value of serum metabolomics analysis in predicting the response to cardiac resynchronization therapy
- Effects of febuxostat on atrial remodeling in a rabbit model of atrial fibrillation induced by rapid atrial pacing
- Adverse reactions of Amiodarone
- Approach to a patient with cardiac amyloidosis
