Non-albicans Candida prosthetic joint infections:A systematic review of treatment
2019-08-14ChristosKoutserimpasStylianosZervakisSofiaMarakiKalliopiAlpantakiArgyriosIoannidisDiamantisKofteridisGeorgeSamonis
Christos Koutserimpas,Stylianos G Zervakis,Sofia Maraki,Kalliopi Alpantaki,Argyrios Ioannidis,Diamantis P Kofteridis,George Samonis
Abstract
Key words: Fungal prosthetic joint infection; Knee arthroplasty infection; Hip arthroplasty infection; Antifungal treatment; Non-albicans Candida prosthetic joint infections
INTRODUCTION
Prosthetic joint infection (PJI) is a severe complication of joint surgery,involving the joint prostheses and contiguous tissue,representing a main cause of total arthroplasty failure[1].A plethora of microorganisms have been held responsible for these infections,such as Gram-positive and negative bacteria,while fungal microorganisms are considered rare causes.Fungal PJIs occur in about 1-2% of all cases,while the most common spread type seems to be hematogenous[2].
Optimal treatment is considered the two stage revision surgery in combination with an antifungal agent.However,no clear guidelines have yet been developed regarding the agent and treatment duration.Hence,a broad range of antifungal and surgical treatments have been reported so far[3,4].
Candidaspp represent the most common fungal pathogens for PJIs,withCandida albicansbeing the most prevalent species.However,over the last years,the incidence of non-albicans CandidaPJIs has increased[4,5].The purpose of this study was to clarify,by reviewing current published cases,the treatment options of non-albicans CandidaPJIs in order to potentially improve the medical and surgical care of such cases.
MATERIALS AND METHODS
A search of PubMed and MEDLINE databases was performed to identify all existing articles reporting the management of non-albicans CandidaPJIs cases through April 2018.Isolated and combined terms of “fungal prosthetic joint infection”,“fungal arthroplasty infection”,“fungal hip arthroplasty infection”,“fungal knee arthroplasty infection”,“fungal shoulder arthroplasty infection”,as well as terms including each non-albicans Candidaspecies (e.g.,“candida glabratajoint infection”,“candida parapsilosisjoint infection,etc) were used.The citations in each article were reviewed to locate additional references that were not retrieved during the initial search.
The present review is limited to papers published in English,peer-reviewed journals.Furthermore,cases without information about management and treatment were excluded.The data extracted from these studies included age,gender,affected joint,responsible non-albicans Candidaspecies,duration and type of antifungal treatment,type of surgical treatment,time between initial arthroplasty and symptom onset,time between symptom onset and definite diagnosis (culture),outcome of the infection and follow-up of each case.Charlson Comorbidity score was calculated,when possible,by two independent investigators based on the information provided from each report.
Data were recorded and analyzed using Microsoft Excel 2010 (Microsoft Corporation,Redmond,Washington).Two-sided Fisher’s exact tests were used to compare success rates between groups.Statistical analyses were carried out at the 5%level of significance.
RESULTS
Table1 highlights the findings from the electronic search,covering a 39 year period ending in 2018.A total of 83 non-albicans CandidaPJIs were identified[4,6-47].A total of 46 cases (55.4%) were female patients,thirty-six male (43.4%),while in one case the gender was not clarified.The mean age of the study population was 66.3 years[standard deviation (SD) = 10.2].The affected joint was the knee in 52 cases (62.6%),the hip in 29 (35%) and the shoulder in two (2.4%).Two of the knee prosthetic joint cases were bilateral.The mean Charlson comorbidity index of patients was 4.4 (SD =1.5).
1.3.4 福山区政府政策优势。福山区政府确立了以特色樱桃产业带动经济发展、以优秀电商模式推动特色樱桃产业的双驱动模式,不断提升樱桃特色产业的水平,使大樱桃的电商模式驶入“快车道”。自2006年以来,在面对其他大樱桃地区的快速发展时,福山政府推动了樱桃品牌的创立,大樱桃产业发展需要品牌意识,以实现利益与品牌价值的捆绑提升,在提高水果质量的同时,也提升了品牌认证的力度,不断地巩固福山区大樱桃的优势地位[1]。
The mean time from initial arthroplasty implantation surgery to symptom onset was 27.2 mo (SD = 43),while the mean time from symptom onset to culture-confirmed diagnosis was 7.5 mo (SD = 12.5).Regarding the causative non-albicans Candidaspecies,the most frequently isolated one wasC.parapsilosis,found in 45 cases (54.2%),followed byC.glabratain 18 (21.7%),C.tropicalisin ten (12%),C pelliculosain three(3.6%) andC.lusitanaein two (2.4%),whileC.famata,C.lipolytica,C.utilis,C.guilliermondiiandC.freyschussiihad caused one case each (1.2%) (Figure 1).
Regarding surgical treatment,in the majority of the described cases (44 cases; 53%)a two stage revision arthroplasty (TSRA) was performed,followed by resection arthroplasty (RA) (18 cases; 22%),one stage revision arthroplasty (OSRA) (eight cases;9.6%),arthrodesis (five cases; 6%),debridement (three cases; 3.6%) and amputation(two cases; 2.4%).In three cases (3.6%),there was no surgical treatment (Figure 2).TSRA exhibited a success rate of 96%,RA a rate of ≥ 61% [in 7 cases information about the infection outcome was not provided (studies 8,31,32,46,60,62,66 in Table 1)],OSRA a rate of 73%,debridement a rate of 75%,amputation a rate of 100%,while no surgical treatment has shown a success rate of 60%.TSRA when compared to OSRA had a higher success rate (96%vs73%;P-value = 0.023).
Regarding the preferred antifungal agent,38 cases (45.8%) were treated with a single drug,29 (34.9%) with two,12 (14.5%) with more than two,while one case did not receive antifungal treatment [(1.2%); case 17 in Table 1; the antifungal agent was not reported in case 32].
Fluconazole was used in most cases [59; (71%),in 31 of them (52.5%) as monotherapy],followed by amphotericin B [41; (49.4%),in 4 (9.8%) as monotherapy],flucytosine [13; (15.7%),in 1 (7.7%) as monotherapy],caspofungin [7; (8.4%),in 1(14.3%) as monotherapy],voriconazole [7; (8.4%),in 2 (28.6%) as monotherapy],ketoconazole [5; (6%),none as monotherapy],itraconazole [3; (3.6%),none as monotherapy] and anidulafungin [l; (1.2%),not as monotherapy].The final outcome was successful in 74 cases (89.2%).
The majority of patients withC.parapsilosisPJIs were treated with fluconazole [30 cases; (66.7%),in 22 (73.3%) as monotherapy],followed by amphotericin B [19;(42.2%),none as monotherapy],flucytosine [8; (17.8%),in 1 (12.5%) as monotherapy],ketoconazole [3; (6.7%),none as monotherapy],while voriconazole and itraconazole were used in 1 case each (none as monotherapy).Outcome was successful in 40 cases(88.9%).
The majority of cases withC.glabrataPJIs were treated with amphotericin B [8;(44.4%),in 1 (12.5%) as monotherapy],followed by fluconazole [7; (38.9%),in 3(42.9%) as monotherapy].Caspofungin and voriconazole were used in 5 cases (27.8%)each,in 1 (20%) case each as monotherapy.Furthermore,three (16.7%) patients received flucytosine (none as monotherapy),two (11.1%) itraconazole (none as monotherapy) and one (5.6%) anidulafungin (not as monotherapy).Outcome was successful in 17 cases (94.4%),while one patient (case number 11 in Table 1) passedaway from unrelated causes.

Table1 Non-albicans Candida prosthetic joint infection cases
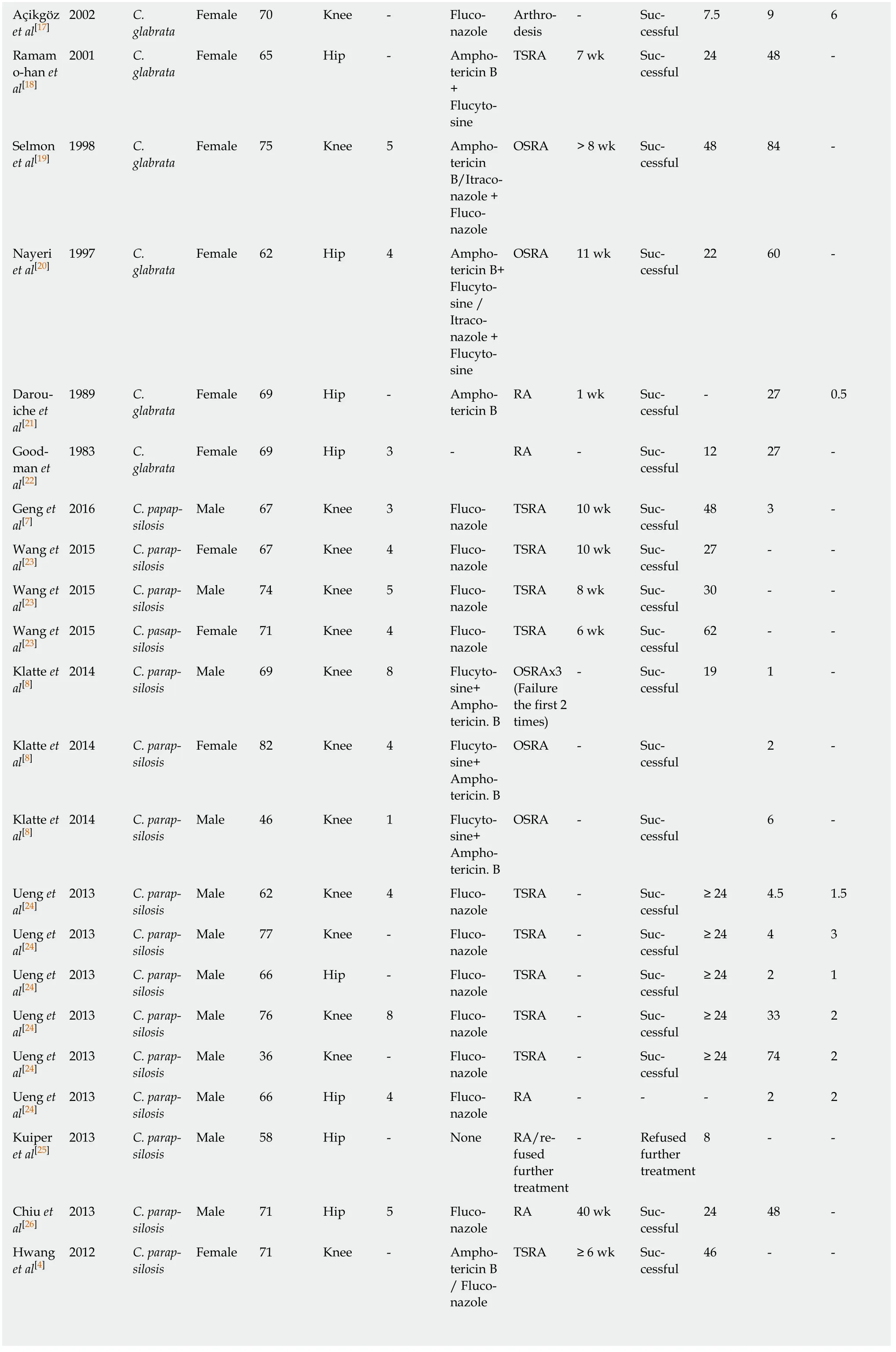
Açikgöz et al[17]2002 C.glabrata Female 70 Knee-Fluconazole Arthrodesis- Successful 7.5 9 6 Ramam o-han et al[18]2001 C.glabrata Female 65 Hip-Amphotericin B+Flucytosine TSRA 7 wk Successful 24 48 -Selmon et al[19]1998 C.glabrata Female 75 Knee 5 Amphotericin B/Itraconazole +Fluconazole OSRA > 8 wk Successful 48 84 -Nayeri et al[20]1997 C.glabrata Female 62 Hip 4 Amphotericin B+Flucytosine /Itraconazole +Flucytosine OSRA 11 wk Successful 22 60 -Darouiche et al[21]1989 C.glabrata Female 69 Hip-Amphotericin B RA 1 wk Successful- 27 0.5 Goodman et al[22]1983 C.glabrata Female 69 Hip 3-RA-Successful 12 27 -Geng et al[7]2016 C.papapsilosis Male 67 Knee 3 Fluconazole TSRA 10 wk Successful 48 3 -Wang et al[23]2015 C.parapsilosis Female 67 Knee 4 Fluconazole TSRA 10 wk Successful 27--Wang et al[23]2015 C.parapsilosis Male 74 Knee 5 Fluconazole TSRA 8 wk Successful 30--Wang et al[23]2015 C.pasapsilosis Female 71 Knee 4 Fluconazole TSRA 6 wk Successful 62--Klatte et al[8]2014 C.parapsilosis Male 69 Knee 8 Flucytosine+Amphotericin.B OSRAx3(Failure the first 2 times)- Successful 19 1 -Klatte et al[8]2014 C.parapsilosis Female 82 Knee 4 Flucytosine+Amphotericin.B OSRA-Successful 2 -Klatte et al[8]2014 C.parapsilosis Male 46 Knee 1 Flucytosine+Amphotericin.B OSRA-Successful 6 -Ueng et al[24]2013 C.parapsilosis Male 62 Knee 4 Fluconazole TSRA-Successful≥ 24 4.5 1.5 Ueng et al[24]2013 C.parapsilosis Male 77 Knee-Fluconazole TSRA-Successful≥ 24 4 3 Ueng et al[24]2013 C.parapsilosis Male 66 Hip-Fluconazole TSRA-Successful≥ 24 2 1 Ueng et al[24]2013 C.parapsilosis Male 76 Knee 8 Fluconazole TSRA-Successful≥ 24 33 2 Ueng et al[24]2013 C.parapsilosis Male 36 Knee-Fluconazole TSRA-Successful≥ 24 74 2 Ueng et al[24]2013 C.parapsilosis Male 66 Hip 4 Fluconazole RA---2 2 Kuiper et al[25]2013 C.parapsilosis Male 58 Hip-None RA/refused further treatment- Refused further treatment 8--Chiu et al[26]2013 C.parapsilosis Male 71 Hip 5 Fluconazole RA 40 wk Successful 24 48 -Hwang et al[4]2012 C.parapsilosis Female 71 Knee-Amphotericin B/ Fluconazole TSRA ≥ 6 wk Successful 46--
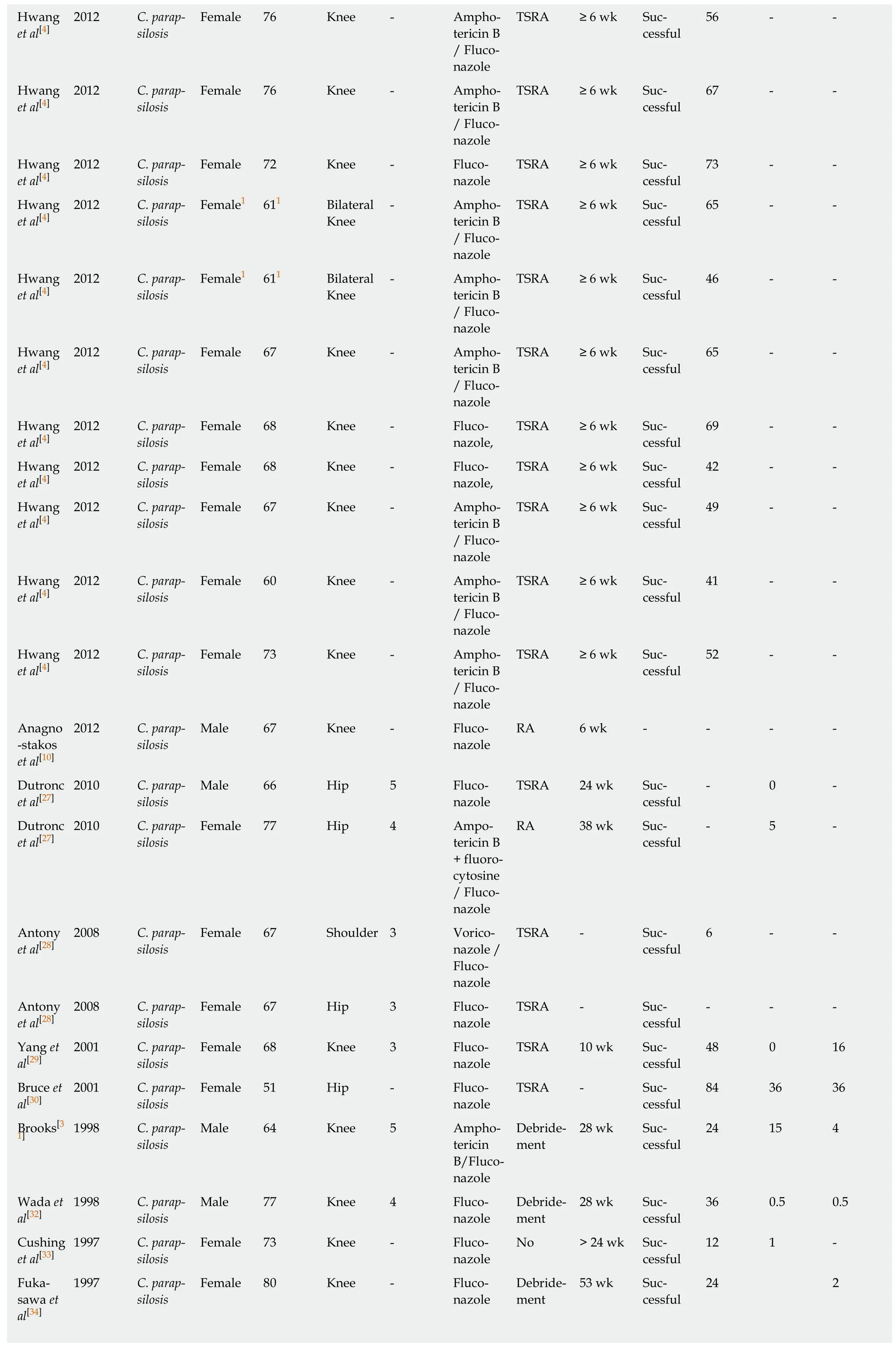
Hwang et al[4]2012 C.parapsilosis Female 76 Knee-Amphotericin B/ Fluconazole TSRA ≥ 6 wk Successful 56--Hwang et al[4]2012 C.parapsilosis Female 76 Knee-Amphotericin B/ Fluconazole TSRA ≥ 6 wk Successful 67--Hwang et al[4]2012 C.parapsilosis Female 72 Knee-Fluconazole TSRA ≥ 6 wk Successful 73--Hwang et al[4]2012 C.parapsilosis Female1 611 Bilateral Knee- Amphotericin B/ Fluconazole TSRA ≥ 6 wk Successful 65--Hwang et al[4]2012 C.parapsilosis Female1 611 Bilateral Knee- Amphotericin B/ Fluconazole TSRA ≥ 6 wk Successful 46--Hwang et al[4]2012 C.parapsilosis Female 67 Knee-Amphotericin B/ Fluconazole TSRA ≥ 6 wk Successful 65--Hwang et al[4]2012 C.parapsilosis Female 68 Knee-Fluconazole,TSRA ≥ 6 wk Successful 69--Hwang et al[4]2012 C.parapsilosis Female 68 Knee-Fluconazole,TSRA ≥ 6 wk Successful 42--Hwang et al[4]2012 C.parapsilosis Female 67 Knee-Amphotericin B/ Fluconazole TSRA ≥ 6 wk Successful 49--Hwang et al[4]2012 C.parapsilosis Female 60 Knee-Amphotericin B/ Fluconazole TSRA ≥ 6 wk Successful 41--Hwang et al[4]2012 C.parapsilosis Female 73 Knee-Amphotericin B/ Fluconazole TSRA ≥ 6 wk Successful 52--Anagno-stakos et al[10]2012 C.parapsilosis Male 67 Knee-Fluconazole RA 6 wk----Dutronc et al[27]2010 C.parapsilosis Male 66 Hip 5 Fluconazole TSRA 24 wk Successful- 0 -Dutronc et al[27]2010 C.parapsilosis Female 77 Hip 4 Ampotericin B+ fluorocytosine/ Fluconazole RA 38 wk Successful- 5 -Antony et al[28]2008 C.parapsilosis Female 67 Shoulder 3 Voriconazole /Fluconazole TSRA-Successful 6--Antony et al[28]2008 C.parapsilosis Female 67 Hip 3 Fluconazole TSRA-Successful---Yang et al[29]2001 C.parapsilosis Female 68 Knee 3 Fluconazole TSRA 10 wk Successful 48 0 16 Bruce et al[30]2001 C.parapsilosis Female 51 Hip-Fluconazole TSRA-Successful 84 36 36 Brooks[3 1] 1998 C.parap-24 15 4 silosis Male 64 Knee 5 Amphotericin B/Fluconazole Debridement 28 wk Successful Wada et al[32]1998 C.parapsilosis Male 77 Knee 4 Fluconazole Debridement 28 wk Successful 36 0.5 0.5 Cushing et al[33]1997 C.parapsilosis Female 73 Knee-Fluconazole No > 24 wk Successful 12 1 -Fukasawa et al[34]1997 C.parapsilosis Female 80 Knee-Fluconazole Debridement 53 wk Successful 24 2
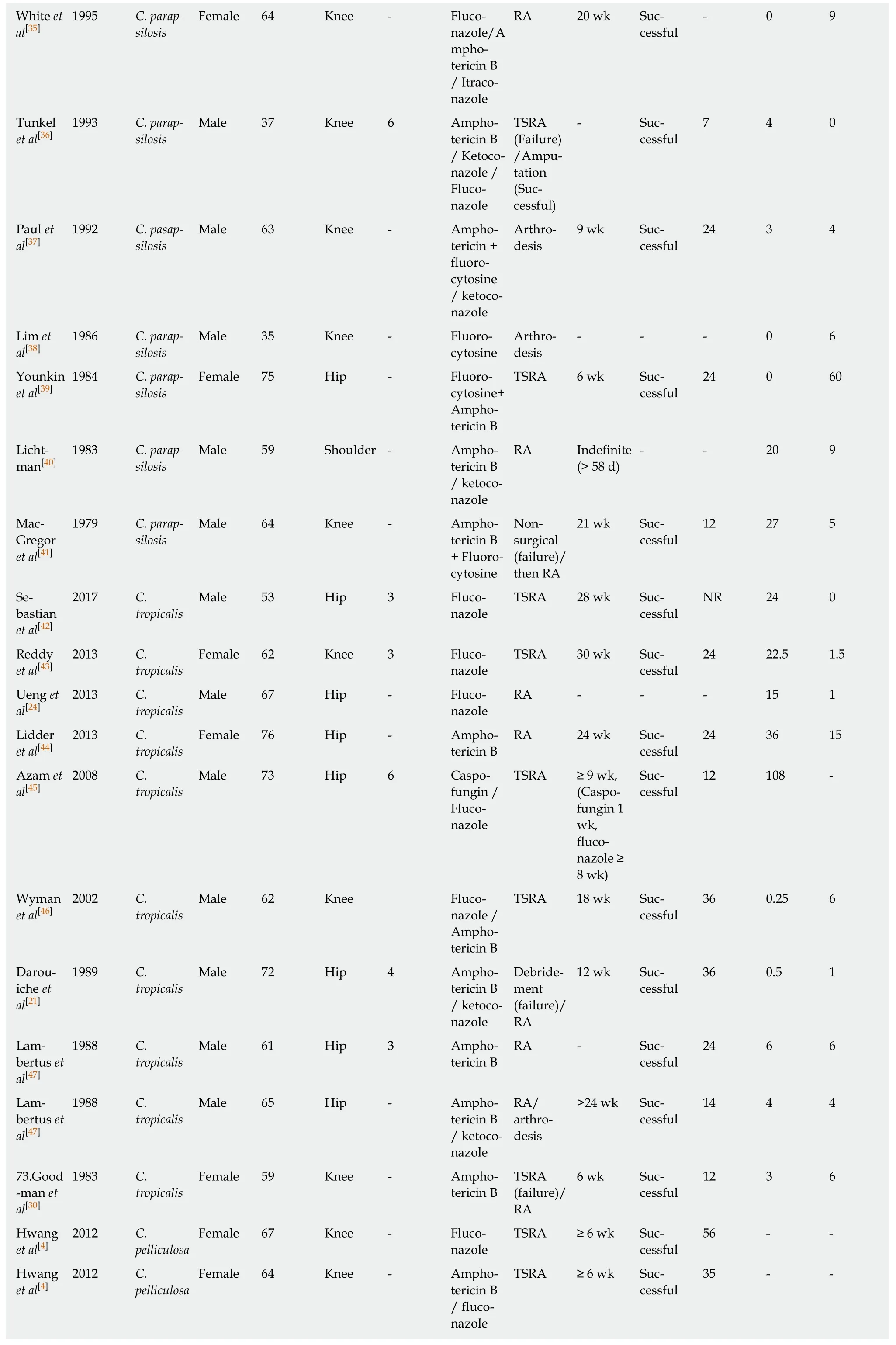
White et al[35]1995 C.parapsilosis Female 64 Knee-Fluconazole/A mphotericin B/ Itraconazole RA 20 wk Successful- 0 9 Tunkel et al[36]1993 C.parapsilosis Male 37 Knee 6 Amphotericin B/ Ketoconazole /Fluconazole TSRA(Failure)/Amputation(Successful)- Successful 7 4 0 Paul et al[37]1992 C.pasapsilosis Male 63 Knee-Amphotericin +fluorocytosine/ ketoconazole Arthrodesis 9 wk Successful 24 3 4 Lim et al[38]1986 C.parapsilosis Male 35 Knee-Fluorocytosine Arthrodesis--- 0 6 Younkin et al[39]1984 C.parapsilosis Female 75 Hip-Fluorocytosine+Amphotericin B TSRA 6 wk Successful 24 0 60 Lichtman[40]1983 C.parapsilosis Male 59 Shoulder-Amphotericin B/ ketoconazole RA Indefinite(> 58 d)--20 9 Mac-Gregor et al[41]1979 C.parapsilosis Male 64 Knee-Amphotericin B+ Fluorocytosine Nonsurgical(failure)/then RA 21 wk Successful 12 27 5 Sebastian et al[42]2017 C.tropicalis Male 53 Hip 3 Fluconazole TSRA 28 wk Successful NR 24 0 Reddy et al[43]2013 C.tropicalis Female 62 Knee 3 Fluconazole TSRA 30 wk Successful 24 22.5 1.5 Ueng et al[24]2013 C.tropicalis Male 67 Hip-Fluconazole RA---15 1 Lidder et al[44]2013 C.tropicalis Female 76 Hip-Amphotericin B RA 24 wk Successful 24 36 15 Azam et al[45]2008 C.tropicalis Male 73 Hip 6 Caspofungin /Fluconazole TSRA ≥ 9 wk,(Caspofungin 1 wk,fluconazole ≥8 wk)Successful 12 108 -Wyman et al[46]2002 C.tropicalis Male 62 Knee Fluconazole /Amphotericin B TSRA 18 wk Successful 36 0.25 6 Darouiche et al[21]1989 C.tropicalis Male 72 Hip 4 Amphotericin B/ ketoconazole Debridement(failure)/RA 12 wk Successful 36 0.5 1 Lambertus et al[47]1988 C.tropicalis Male 61 Hip 3 Amphotericin B RA-Successful 24 6 6 Lambertus et al[47]1988 C.tropicalis Male 65 Hip-Amphotericin B/ ketoconazole RA/arthrodesis>24 wk Successful 14 4 4 73.Good-man et al[30]1983 C.tropicalis Female 59 Knee-Amphotericin B TSRA(failure)/RA 6 wk Successful 12 3 6 Hwang et al[4]2012 C.pelliculosa Female 67 Knee-Fluconazole TSRA ≥ 6 wk Successful 56--Hwang et al[4]2012 C.pelliculosa Female 64 Knee-Amphotericin B/ fluconazole TSRA ≥ 6 wk Successful 35--
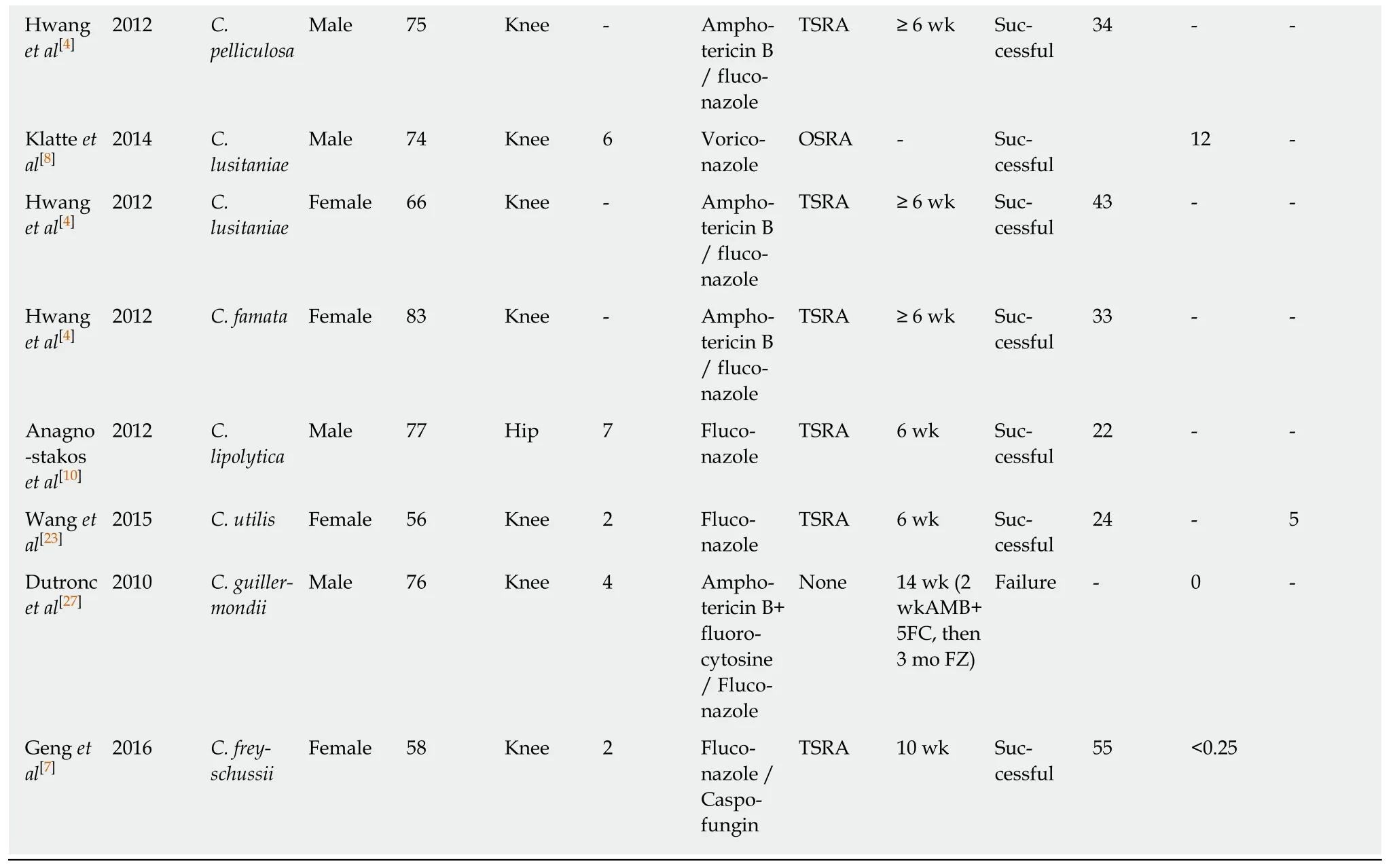
Patient demographics,antifungal treatment,its duration,as well as infection outcome and follow-up period are presented.1Bilateral PJI in the same patient; -:Not reported or unclear.TSRA:Two stage revision arthroplasty; OSRA:One stage revision arthroplasty; RA:Resection arthroplasty.
The majority ofC.tropicalisPJIs were treated with amphotericin B [6; (60%),in 3(50%) as monotherapy],followed by fluconazole [5; (50%),in 3 (60%) as monotherapy],ketoconazole [2; (20%),none as monotherapy] and caspofungin [1;(10%),not as monotherapy].Outcome was successful in 9 cases (90%; case number 66 in Table 1,treated with fluconazole as monotherapy,did not provide information about outcome).
All patients suffering fromC.pelliculosaPJI received fluconazole [3 cases; (100%),1(33.3%) as monotherapy],while 2 of them (66.7%) received amphotericin B (none as monotherapy).All patients (100%) were treated successfully.Both patients suffering fromC.lusitaniaewere treated successfully.Voriconazole was used as monotherapy in 1 case (50%),while amphotericin B and fluconazole were used in the other.
One patient suffering fromC.famatawas successfully treated with amphotericin B and fluconazole,while fluconazole as monotherapy was successfully used for the treatment of each case ofC.lipolyticaandC.utilisPJI.One case ofC.freyschussiiwas successfully treated with fluconazole and caspofungin.A case ofC.guilliermondiiinfection received amphotericin B,fluorocytosine and fluconazole,however,the result was failure.The mean antifungal treatment duration was 12.8 wk (SD = 10.9),while the mean follow-up of these cases was 33.3 mo (SD = 19.6).
DISCUSSION
Fungal invasive infections,such as PJIs,due toCandidaspecies have been acknowledged as a major cause of morbidity and mortality.These infections have been associated with progress in medical modalities,and is some cases have been considered iatrogenic[3,4].CandidaPJIs are relative rare,since only case reports or small case series have been reported so far.Candida albicansis the most prevalent species.However,the incidence of invasive candidiasis and PJIs due to non-albicans Candidais increasing[5,48].Optimal treatment of these infections remains unclear,since no certain guidelines exist for the antifungal,as well as for the surgical treatments[48].It is,therefore,of paramount importance to report such cases and to obtain a better understanding of treatment options and outcomes of these infections.The present study is an effort to review,in a systematic way,the non-albicans CandidaPJI cases
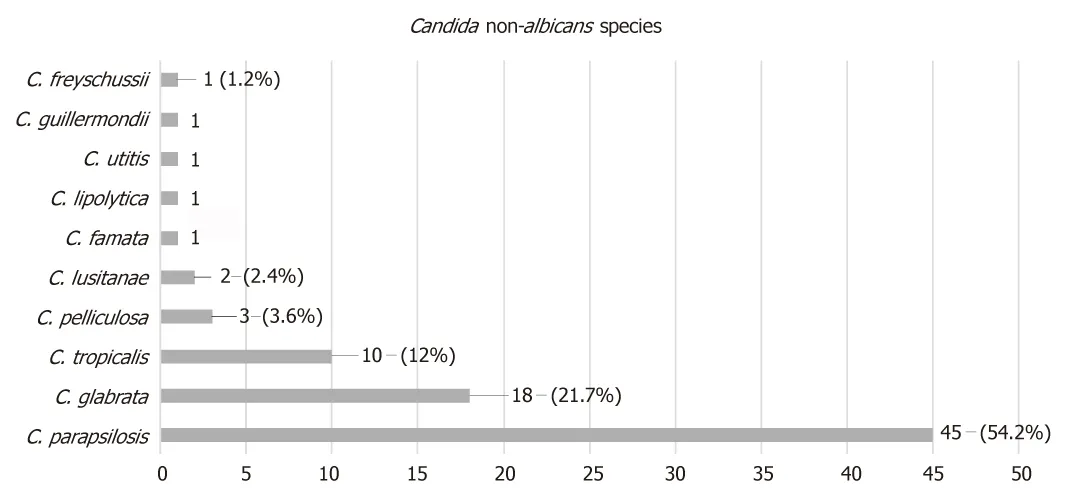
Figure1 Prosthetic joint infection causative non-albicans Candida species.
DISCUSSION
Fungal invasive infections,such as PJIs,due toCandidaspecies have been acknowledged as a major cause of morbidity and mortality.These infections have been associated with progress in medical modalities,and is some cases have been considered iatrogenic[3,4].CandidaPJIs are relative rare,since only case reports or small case series have been reported so far.Candida albicansis the most prevalent species.However,the incidence of invasive candidiasis and PJIs due to non-albicans Candidais increasing[5,48].Optimal treatment of these infections remains unclear,since no certain guidelines exist for the antifungal,as well as for the surgical treatments[48].It is,therefore,of paramount importance to report such cases and to obtain a better understanding of treatment options and outcomes of these infections.The present study is an effort to review,in a systematic way,the non-albicans CandidaPJI cases described in the literature.The study focuses on the preferred antifungal agent,the optimal surgical treatment,and the duration of therapy.
The electronic search has revealed a total of 83 patients with non-albicans CandidaPJI.Their mean age was 66.3 years.AlthoughCandidaPJI is still considered rare,its incidence is expected to rise,due to the increasing number of joint arthroplasty surgeries performed worldwide[2,48].
Several risk factors have been identified for invasive candidiasis,such as immunosuppression,long-term antimicrobial use and systemic disease[3,4,5,48].Such a patient profile has been illustrated by the relatively high mean Charlson comorbidity index of the present study’s population,found to be 4.4.
CandidaPJI is most commonly considered of hematogenous origin[2,6,48].The mean time between initial arthroplasty surgery and symptomatology onset in the study population was 27.2 mo,while it ranged from immediately after surgery to 264 mo.It is of note that in 13 cases [15.7%; cases 8,23,47,51,54,55,57,60,61,69,70,82,83(Table 1)] this time was found to be less than 1 mo.Therefore,in these cases the spread should be considered perioperative.
It is also of interest that the mean time between symptomatology onset and definite(culture-based) diagnosis was 7.5 mo,ranging from immediately after onset to 60 mo.This could be attributed to the fact that the main symptoms ofCandidaPJI are nonspecific,which mainly include pain and swelling[1-5,48].The symptomatology onset may be mild,insidious and slowly progressive.Therefore,diagnosis may be delayed due to low suspicion index.
The most frequently isolated non-albicans Candidaspp wasC.parapsilosis,found in 45 cases (54.2%),followed byC.glabratain 18 ( 21.7%),C.tropicalisin 10 (12%),C pelliculosain 3 (3.6%),C.lusitanaein 2 ( 2.4%) and 1 case each (1.2%) of PJI caused byC.famata,C.lipolytica,C.utitis,C.guillermondiiandC.freyschussii.
In the present study,C.parapsilosiswas found to be the predominant pathogen causing PJIs,as compared to other non-albicans Candidaspecies.C.parapsilosisprevalence has dramatically increased over the last 3 decades.Infections due to this pathogen are more frequently associated with prosthetic devices,indwelling catheters and hyperalimentation solutions.The pathogenesis of the infection depends on the expression of virulence factors,including adherence to host cells and tissues,biofilm formation and secretion of extracellular hydrolytic enzymes[5,49].

Figure2 Surgical treatment for non-albicans Candida prosthetic joint infection.
The treatment ofC.parapsilosisPJIs has proven to be successful in 88.9% of the studied cases.This is probably due to the fact that echinocandines were not used for the treatment of such cases,taking into account thatC.parapsilosis’ MICs are usually elevated to echinocandins,as compared to otherCandidaspp[50].
Treatment ofC.glabrataPJIs has been successful in 94.4% of the studied cases.This is probably due to the fact that an azole compound has rarely been used for treatment and,in the limited number of cases when an azole was used,the drug has been given in combination with another antifungal,taking into account thatC.glabratais often resistant to azoles[50].In most cases ofC.tropicalisPJIs,treatment has been successful,since either single antifungal agents or combinations are known to be effective against thisCandidaspp.
All cases ofC.pelliculosaPJIs have been treated successfully due to the use of effective agents.C.lusitaniaeis intrinsically resistant to amphotericin B[50,51].One case received this agent in combination with fluconazole,while the other one was treated with voriconazole as monotherapy.Hence,finally,the 2 cases caused byC.lusitanaewere successfully treated.
The cases ofC.famata,C.lypoliticaandC.utiliswere successfully treated with the antifungals given.It is of note that the single case ofC.guillermondii,although treated with a combination of antifungals,resulted in failure.For successful treatment,it is of the utmost importance to carry out susceptibility testing to obtain accurate MIC values followingCandidaisolation,taking into account that differentCandidaspecies are characterized by intrinsic resistance to certain antifungal compounds.Regarding the preferred antifungal agent,fluconazole was used in most cases [59; (71%),in 31 of them (52.5%) as monotherapy],followed by amphotericin B [41; (49.4%),in 4 (9.8%) as monotherapy].Fluconazole has been rarely associated with severe hepatotoxicity.Therefore,liver function tests should be performed regularly during prolonged fluconazole therapy[50,51].Amphotericin B is an effective broad spectrum agent.However,it is relatively toxic and its side effects,including renal dysfunction,may restrict its long-term use,which is essential in PJI cases[6].Echinocandines are the most recently developed anti-Candida agents.Although C.parapsilosis strains mostly exhibit high MICs,these agents can often be clinically effective due to their immunomodulatory properties and the fact that they successfully penetrate biofilms[52].
The mean duration of antifungal treatment in the study population was 12.8 wk,while it ranged from 1 to 53 wk.One case (case 32 in Table 1) did not receive any antifungal treatment.Guidelines for the treatment of osteoarticular infections fromCandidaspp exist.However,no clear recommendations are available for the treatment of such PJIs[6,48].Therefore,the treatment duration is mainly based on the clinical and laboratory findings of each case.
Several options for surgical treatment have also been described.In the study population,in most cases (44 cases; 53%) a TSRA was performed,followed by RA (18 cases; 22%),OSRA (8 cases; 9.6%),arthrodesis (5 cases; 6%),debridement (3 cases;3.6%) and amputation (2 cases; 2.4%).Three cases did not receive surgical treatment(3.6%; case 4,55 and 82 in Table 1).RA,arthrodesis,amputation and debridement are usually considered alternative options to arthroplasty exchange.TSRA had a statistically significant higher success rate when compared to OSRA (96%vs73%;Pvalue = 0.023).Therefore,it seems more proper that TSRA should be considered as the optimal surgical intervention.
The present review has shown that non-albicans CandidaPJIs represent a dangerous reality.Optimal management consists of a combination of the proper medical antifungal treatment based on susceptibility testing and surgical intervention.Although there have been reports of successful treatment of such cases with OSRA and debridement only,TSRA should be strongly recommended.The combination of TSRA separated by 3-6 mo and a prolonged period of antifungal therapy is suggested on the basis of limited data.Additional issues,such as the duration of antifungal therapy after prosthesis implantation (second stage of the TSRA),as well as the role of antifungal-loaded cement spacers,need to be addressed in order to determine the optimal treatment combinations.
ARTICLE HIGHLIGHTS
Research background
Prosthetic joint infection (PJI) represents a severe complication of joint reconstruction surgery,causing total arthroplasty failure.Many pathogens have been identified in PJIs,such as Grampositive and negative bacteria,while fungal microorganisms are considered rare causes,occurring in 1-2% of cases.Candida spp represent the most common fungal pathogens in these infections,with Candida albicans being the most prevalent species.However,the incidence of non-albicans Candida PJIs has increased over the last years.Hence,regarding non-albicans Candida PJIs,only case reports or small series have been reported so far.Optimal treatment is considered the two stage revision surgery in combination with an antifungal agent.However,no clear guidelines have yet been developed regarding the agent and treatment duration.Hence,a broad range of antifungal and surgical treatments has been reported so far.The present review article represents the first effort of evaluating the reported non-albicans Candida PJIs,aiming to clarify the treatment options of these infections and,possibly,to improve the medical and surgical care of such cases.
Research motivation
The absence of clear guidelines regarding fungal PJIs represents a primary issue in managing these infections in clinical practice.A broad range of antifungal and surgical treatments have been reported,while treatment duration remains unclear.Furthermore,due to the limited data regarding these infections,information about patient demographics,responsible non- albicans Candida species,time between initial arthroplasty and symptom onset,time between symptom onset and definite diagnosis (culture),and outcome of the infection has not been reported in a systematic way.Hence,it is of utmost importance in the future to report such cases in order to obtain a better understanding about this devastating arthroplasty complication.
Research objectives
The main objective of this study was to clarify,by systematically reviewing current published cases in the literature,the treatment options of non-albicans Candida PJIs and,possibly,to improve the medical and surgical care of such cases.During the process of reviewing the literature,it became apparent that information about patient demographics,fungal species,time between initial arthroplasty and symptom onset,time between symptom onset and definite diagnosis (culture),as well as outcome of the infection should also be reported,due to the absence of a systematic review regarding this topic.
Research methods
A meticulous electronic search of Pub Med and MEDLINE databases was performed to identify all articles reporting the management of non-albicans Candida PJIs cases through April 2018 by two independent investigators.The citations in each article were reviewed to locate additional references that were not retrieved during the initial search.The evaluated parameters were patient demographics and comorbidities,affected joints,responsible non- albicans Candida species,duration and type of antifungal treatment,type of surgical treatment,time between initial arthroplasty and symptom onset,time between symptom onset and definite diagnosis(culture),and outcome of the infection.Data were recorded and analyzed using Microsoft Excel 2010 (Microsoft Corporation,Redmond,Washington).Two-sided Fisher’s exact tests were used to compare success rates between groups.Statistical analyses were carried out at the 5% level of significance.
Research results
A total of 83 non-albicans Candida PJIs were located,with a mean age of 66.3 years (SD = 10.2).The knee was the affected joint in 52 cases (62.6%),the hip in 29 (35%) and the shoulder in 2(2.4%).The mean time from arthroplasty to symptoms onset was found to be 27.2 mo (SD = 43),while the mean time from symptoms onset to culture-confirmed diagnosis was 7.5 mo (SD =12.5).The most commonly isolated non-albicans Candida species was C.parapsilosis,found in 45 cases (54.2%),followed by C.glabrata in 18 (21.7%),C.tropicalis in 10 (12%),C pelliculosa in 3(3.6%) and C.lusitanae in 2 (2.4%),while C.famata,C.lipolytica,C.utilis,C.guilliermondii and C.freyschussii had caused one case each (1.2%).A two stage revision arthroplasty (TSRA) was performed in most cases (44 cases; 53%),followed by RA (18 cases; 22%),OSRA (8 cases; 9.6%),arthrodesis (5 cases; 6%),debridement (3 cases; 3.6%) and amputation (2 cases; 2.4%),while 3 cases (3.6%) received no surgical treatment.TSRA when compared to OSRA had a higher success rate (96%vs73%;P-value = 0.023).Fluconazole was used in most cases as antifungal treatment[59; (71%),in 31 of them (52.5%) as monotherapy],followed by amphotericin B [41; (49.4%),in 4(9.8%) as monotherapy],flucytosine [13; (15.7%),in 1 (7.7%) as monotherapy],caspofungin [7;(8.4%),in 1 (14.3%) as monotherapy],voriconazole [7; (8.4%),in 2 (28.6%) as monotherapy],ketoconazole [5; (6%),none as monotherapy],itraconazole [3; (3.6%),none as monotherapy] and anidulafungin [l; (1.2%),none as monotherapy].The final outcome was successful in 74 cases(89.2%).The mean antifungal treatment duration was 12.8 wk (SD = 10.9),while the mean follow-up of these cases was 33.3 mo (SD = 19.6).The present review has shown that the optimal management of non-albicans Candidaconsists of a combination of the proper medical antifungal treatment and surgical intervention.Although there have been reports of the successful treatment of such cases with OSRA and debridement only,TSRA should be strongly recommended.The combination of TSRA and a prolonged period of antifungal therapy based on susceptibility testing is suggested on the basis of limited data.Additional issues,such as the duration of antifungal therapy after prosthesis implantation (second stage of the TSRA) and the role of antifungal-loaded cement spacers need to be addressed in order to determine an optimal treatment combination.
Research conclusions
The present study is an effort to review,in a systematic way,the non-albicans CandidaPJI cases described in the literature.The study focuses on the preferred antifungal agent,the optimal surgical treatment,and the duration of therapy.C.parapsilosiswas found to be the predominant pathogen causing PJIs,as compared to other non-albicans Candidaspecies.For successful management of non-albicans CandidaPJI,susceptibility testing to obtain accurate MIC values should always be performed following theCandidaisolation,considering that differentCandidaspecies are characterized by intrinsic resistance to certain antifungal compounds.The mean duration of antifungal treatment in the present review was 12.8 wk,while it ranged from 1 to 53 wk.Although,guidelines for the treatment of osteoarticular infections fromCandidaspp are available,no clear recommendations exist for the treatment of such PJIs.Therefore,the treatment duration is mostly based upon clinical and laboratory findings.In most cases (44 cases; 53%) a TSRA was performed,followed by RA (18 cases; 22%),OSRA (8 cases; 9.6%),arthrodesis (5 cases;6%),debridement (3 cases; 3.6%) and amputation (2 cases; 2.4%).Three cases did not receive surgical treatment (3.6%).RA,arthrodesis,amputation and debridement are usually considered alternative options to arthroplasty exchange.TSRA when compared to OSRA had a statistically significant higher success rate (96%vs73%;P-value= 0.023).Therefore,it seems more proper that TSRA should be considered as the optimal surgical intervention.The present review has shown that the optimal management of non-albicans CandidaPJIs consists of a combination of the proper medical antifungal treatment based on susceptibility testing and a surgical intervention,while TSRA should be strongly recommended.The combination of TSRA separated by 3-6 mo,in addition to a prolonged period of antifungal therapy,is suggested.
Research perspectives
Non-albicans CandidaPJIs represent a dangerous reality.The combination of TSRA separated by 3-6 mo and a prolonged period of antifungal therapy is suggested on the basis of limited data.It is of paramount importance to report the treatment of such cases,even the failed ones,in order to obtain a better understanding of these infections and to determine the optimum treatment combination.
猜你喜欢
杂志排行
World Journal of Clinical Cases的其它文章
- Thoracotomy of an asymptomatic,functional,posterior mediastinal paraganglioma:A case report
- Novel heterozygous missense mutation of SLC12A3 gene in Gitelman syndrome:A case report
- Female genital tract metastasis of lung adenocarcinoma with EGFR mutations:Report of two cases
- Premonitory urges located in the tongue for tic disorder:Two case reports and review of literature
- Removal of pediatric stage IV neuroblastoma by robot-assisted laparoscopy:A case report and literature review
- Secondary lymphoma develops in the setting of heart failure when treating breast cancer:A case report
