Thoracotomy of an asymptomatic,functional,posterior mediastinal paraganglioma:A case report
2019-08-14YiYuYinBinYangYeniAitAhmedHuaXin
Yi-Yu Yin,Bin Yang,Yeni Ait Ahmed,Hua Xin
Abstract
Key words: Mediastinal tumor; Paraganglioma; Pheochromocytoma; Hypertension; Case report
INTRODUCTION
Ninety percent of neuroendocrine tumors arise from chromaffin cells in the adrenal medulla and are commonly known as pheochromocytomas.The remaining 10%originate from neural crest progenitors located outside of the adrenal gland,and are called paragangliomas[1].The paragangliomas that occur in the mediastinum are extremely rare,accounting for only 1%-2% of all paragangliomas and < 0.3% of all mediastinal tumors[2],with only about 150 cases reported in the literature[3].Paragangliomas can be classified as functional or non-functional ones based on their ability to synthesize and release catecholamines[4].Most paragangliomas are nonfunctional[2],therefore asymptomatic functional posterior mediastinal paragangliomas are very rare.According to documented cases[2,5,6],perioperative interventions including oral administration of alpha-receptor blocker (phenoxybenzamine) and full intravenous fluid resuscitation for two weeks,intraoperative avoidance of tumor irritation,and postoperative close monitoring are all necessary.
CASE PRESENTATION
Chief complaints
Intermittent tearing pain on the left side of the chest and back for more than 10 mo in a 47-year-old man.
History of present illness
The patient was admitted to our hospital for physical examination revealing lesions in the left posterior mediastinum space 6 d previously.On admission,the patient’s blood pressure was 120/80 mmHg,pulse was 82 beats/min,breathing was 18 beats/min,and body temperature was 36.5 °C without headaches,palpitations,night sweats,weight loss,facial flushing,etc.
History of past illness
The patient had no history of hypertension.
Personal and family history
He had no history of cigarette smoking or alcohol use,and there were no similar cases in the family.
Physical examination upon admission
Physical examination was unremarkable.
Laboratory examinations
Plasma test of catecholamines yielded the following:Epinephrine 83 pg/mL,norepinephrine 420 pg/mL,and dopamine 82.6 pg/mL.Urine test showed epinephrine 3.22 μg/24 h,norepinephrine 224 μg/24 h,and dopamine 130.5 μg/24 h,suggesting that the tumor had neuroendocrine function.
Imaging examinations
A chest contrast-enhanced computed tomography (CT) scan revealed a round,solid mass in the left posterior mediastinum,with low-density cystic lesions in the middle,and no enlarged lymph nodes in the hilum or mediastinum (Figure 1).No multiple metastases were detected on the whole-body bone scan,which suggested a benign tumor.Preoperative ultrasound-guided biopsy result also indicated a paraganglioma.
FINAL DIAGNOSIS
The pathological diagnosis was paraganglioma with a tumor size of 6.5 cm × 6 cm × 4 cm and the capsule was incomplete.Immunohistochemistry analysis revealed the tumors to be:CK (-),EMA (-),vimentin (+),inhibinα (-),CD34 (-),S-100 (-),CD56 (+),CgA (+),SyN (+),and Ki-67 (<5%+) (Figure 2).
TREATMENT
The patient was placed in the right lateral decubitus position after general anesthesia with double-lumen endotracheal intubation.A 7 cm × 6 cm × 4 cm dark red mass was found on the left side,adjoining the T7-T8 vertebral body,with a clear border,rich blood supply,and incomplete capsule.The mass invaded the posterior chest wall and descending aorta adventitia.The patient’s blood pressure increased to 220/120 mmHg paroxysmally when we touched the tumor.After accelerating the liquid transfusion and reducing blood pressure immediately,the patient’s blood pressure became stable.Subsequently,the capsule of the tumor was peeled off sharply and bluntly.Resection of the tumor was achieved after transecting the nutrient artery derived from the descending aorta (Figure 3).The patient’s blood pressure varied between 115/70 and 120/75 mmHg.The postoperative pathologic tests reported the lesion as a mass with a size of 6.5 cm × 6 cm × 4 cm.The gray-and-red section was soft,with a little capsule about 0.1 cm thick,and a pale-edged cystic degeneration of 2.5 cm-diameter in the central part (Figure 4).
OUTCOME AND FOLLOW-UP
The patient recovered uneventfully after surgery,and his serum catecholamine level recovered to the normal level on postoperative day 3,with no abnormal blood pressure or recurrence during one year of follow-up visits.
DISCUSSION
Paragangliomas most frequently occur in patients with an average age of 49 years irrespective of gender and only 3% of these tumors secrete catecholamines.Meanwhile,paravertebral paragangliomas occur in younger people,with an average age of 29 years and almost half of these tumors synthesize catecholamines[7].Paragangliomas mainly occur in areas where the parasympathetic nerves are abundant in the body,such as the head,neck,mediastinum,adrenal glands,retroperitoneum,and even the bladder,duodenum,and thyroid[8].Mediastinal paraganglioma is mainly concentrated in two areas:the aortic sinus sympathetic ganglion of the posterior mediastinum or the autonomic ganglion of the superior or middle mediastinum[9].About 25% to 70% of extra-adrenal paraganglioma patients are characterized by symptoms and signs of excessive catecholamine secretion[10],mainly manifested as hypertension,facial flushing,palpitations,night sweats,etc.But the patient in the present case had no symptoms of excessive secretion of catecholamines and belonged to a normotensive pheochromocytoma patient.Such cases are rare.Detection of plasma biochemical markers (epinephrine,norepinephrine,and Chromogranin A) is the preferred laboratory test for pheochromocytoma and suspected paraganglioma[11].For the localized and qualitative diagnosis of paraganglioma,CT and magnetic resonance imaging (MRI) are important imaging examination methods.CT scans of paragangliomas show isodensity or slightly lower density,and enhanced CT shows a significant enhancement.MRI T1W1 shows equal or low signal.T2W1 shows medium,high,or non-uniform mixed signals.DW1 shows a high signal.The enhanced scan shows a significant enhancement of the tumor mass[12].When physical examinations reveal lesions in the posterior mediastinum,in addition to considering common neurogenic tumors such as schwannomas,rare ectopic tumors should also be considered to avoid misdiagnosis.
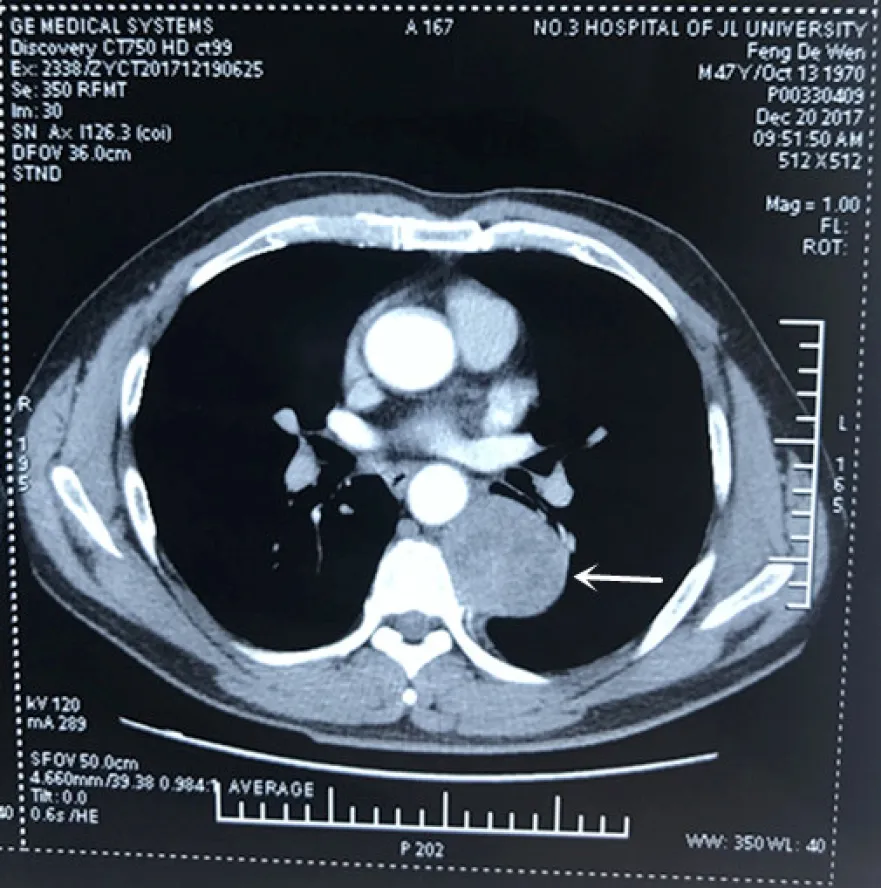
Figure1 Chest-enhanced computed tomography image revealing a round,solid mass in the left posterior mediastinum,with low-density cystic lesions in the middle.
Surgical resection is the preferred treatment for paraganglioma.Thoracoscopic surgery can perfectly expose the operative field and show the fine structure of the lesions.In addition,compared with the traditional thoracic surgery,thoracoscopic surgery has the following benefits:Less trauma,less postoperative pain,speedy recovery,and shorter hospitalization[13].However,because the tumor invades the posterior chest wall and the adventitia of the descending aorta,the thoracoscopic resection of the left posterior mediastinal functional paraganglioma has rarely been reported.Furthermore,cases of successful resection of the tumor in the first stage have rarely been reported,so we preferred a one-stage thoracotomy for safety reasons.Maet al[14]also believe that although thoracoscopic surgery has been successfully applied in their reports,thoracotomy is still the best choice for tumors with abundant blood supply.Perioperative management is also extremely important,including adequate preoperative preparation,careful intraoperative procedures,and strict postoperative care.In the present case,the following procedures were undertaken:(1) Sufficient peripheral vasodilation before surgery,applying αadrenoceptor blockers (phenoxybenzamine 40 mg/d,3 times orally) for 2 wk; (2)Volume expansion,applying low molecular dextran 500 mL/d infusion for 2 wk; (3)Preoperative blood preparation; (4) Real-time monitoring of blood pressure fluctuations during the operation; (5) Closely monitoring blood pressure and heart rate changes after surgery,and maintaining water electrolyte balance; and (6) Review of relevant laboratory indexes after surgery.
Most of the paragangliomas are benign,with only 10% being malignant,and it is difficult to differentiate the benign and malignant tumors just based on their morphology[15].The signs of malignant paraganglioma are metastasis and invasion into surrounding tissues,thus,pathological examination cannot determine the nature.Long-term follow-up visits are necessary to judge the effect of surgery.
CONCLUSION
Paraganglioma is a rare type of tumor,and asymptomatic functional paragangliomas occurring in the left posterior mediastinum are extremely rare.Surgical resection is the preferred method.In the management of such patients,adequate perioperative examination should be undertaken for an accurate diagnosis.One-stage surgical resection should only be performed after implementing suitable perioperative management.Because of the rarity of such tumors,it is necessary to report these cases to raise awareness regarding them.

Figure2 Pathology results.

Figure3 The tumor had a clear border,incomplete capsule.

Figure4 The gray-and-red section was soft,with a little capsule whose thickness was about 0.1 cm,and the 2.5 cm-diameter pale-edged cystic degeneration in the central part.
杂志排行
World Journal of Clinical Cases的其它文章
- Novel heterozygous missense mutation of SLC12A3 gene in Gitelman syndrome:A case report
- Female genital tract metastasis of lung adenocarcinoma with EGFR mutations:Report of two cases
- Premonitory urges located in the tongue for tic disorder:Two case reports and review of literature
- Removal of pediatric stage IV neuroblastoma by robot-assisted laparoscopy:A case report and literature review
- Secondary lymphoma develops in the setting of heart failure when treating breast cancer:A case report
- Longitudinal observation of ten family members with idiopathic basal ganglia calcification:A case report