Adjuvant hormone therapy after radical prostatectomy in highrisk localized and locally advanced prostate cancer: First multicenter, observational study in China
2019-07-13DingweiYeWeiZhangLulinMaChuanjunDuLipingXieYiranHuangQiangWeiZhangqunYeYanqunNa
Dingwei Ye, Wei Zhang, Lulin Ma, Chuanjun Du, Liping Xie, Yiran Huang, Qiang Wei,Zhangqun Ye, Yanqun Na
1Department of Urology, Fudan University Shanghai Cancer Center, Shanghai 200032, China;
2Department of Urology, Jiangsu Province Hospital,Nanjing 210029, China;
3Department of Urology, Peking University Third Hospital, Beijing 100191, China;
5Department of Urology, the First Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou 310003, China;
6Department of Urology, Renji Hospital Shanghai Jiaotong University School of Medicine, Shanghai 200127, China;
7Department of Urology, West China Hospital, Sichuan University, Chengdu 610041, China;
8Department of Urology, Tongji Hospital, Tongji Medical College of Huazhong University of Science and Technology, Wuhan 430030, China;
9Department of Urology, Peking University Shougang Hospital, Beijing 100144, China
Abstract Objective: Potential of combined androgen blockade (CAB) has not been explored extensively in Chinese males with prostate cancer (PCa). Therefore, this study evaluated the 2-year prostate-specific antigen (PSA) recurrence rate and quality of life (QoL) in patients with high-risk localized and locally advanced PCa receiving adjuvant hormone therapy (HT) after radical prostatectomy (RP).Methods: This prospective, multicenter, observational study conducted in 18 centers across China enrolled patients with high-risk factor (preoperative PSA>20 ng/mL or Gleason score >7) or locally advanced PCa. Different adjuvant HT were administered after RP according to investigator’s decision in routine clinical practice.Relationship of baseline and postoperative characteristics was assessed with recurrence rate. PSA recurrence rate and Functional Assessment of Cancer Therapy-Prostate (FACT-P) QoL scores were recorded at 12 months and 24 months. Kaplan-Meier analysis was used to construct the PSA recurrence rate during follow-up.Results: A total of 189 patients (mean age: 66.9±6.5 years) were recruited, among which 112 (59.3%) patients showed serum PSA>20 ng/mL preoperatively. The highest postoperative pathological advancement noticed was from clinical T2 (cT2) to pathological T3 (pT3) (43.9%) stage. The majority of the patients (66.1%) received CAB as adjuvant HT, for a median duration of 20.0 months. The least recurrence (15.2%) was noticed in patients treated with CAB, followed by those treated with luteinizing hormone-releasing hormone agonist (LHRHa) (16.1%), and antiandrogen (19.0%), with non-significant difference noted among the groups. None of the baseline or postoperative characteristics was related with PSA recurrence in our study. The 24-month FACT-P QoL score of 119 patients treated for >12 months showed significant improvement above baseline compared with those treated for ≤12 months.Conclusions: Adjuvant CAB therapy after RP showed reduction trend in 2-year PSA recurrence rate in highrisk Chinese patients with localized and locally advanced PCa, compared with adjuvant anti-androgens (AA) or LHRHa therapy. Further long-term therapy (>12 months) significantly improved QoL compared to short-term HT therapy, suggesting the beneficial effect of long-term CAB therapy in improving QoL.
Keywords: Adjuvant hormone therapy; combined androgen blockade; PSA recurrence; quality of life; radical prostatectomy
Introduction
According to 2012 GLOBOCAN data, an estimated 1.1 million new cases of prostate cancer (PCa) occurred globally in 2012, making it the second most diagnosed cancer in men after lung cancer (1). The 2017 United States cancer statistics reported PCa to have the first highest incidence (161,360 new cases) and the third highest estimated deaths (26,730 deaths) in men (2). In China,cancer data obtained through National Central Cancer Registry revealed PCa as the 7th most common cancer with increasing incidences in men, though lung cancer remains the most common cause of mortality (3). Over the years,the number of PCa cases has declined in developed countries due to early prostate-specific antigen (PSA)screening and better treatment modalities. In contrast,owing to the changing lifestyle and westernization, an increase in incidence and mortality has been observed in the developing countries (4). According to the published literature, Asian men have the least prevalence of PCa in comparison to Western (Caucasians) and Black men, which might play a role in their management also (5,6). On a molecular level, 5 alpha-reductase type II (SRD5A2);cytochromes p 450 CYP3A4, CYP3A5 and CYP3A43, and androgen receptor (AR) gene are responsible for PCa development via the testosterone pathway. Further, genes including macrophage scavenger receptor 1 (MSR1),IVS7delinsTTA and 2’-5’-oligoadenylate-dependent RNase L (RNASEL) Arg462Gln are associated with PCa severity in African-American and Europeans (7).
Among the various diagnostic options, PSA testing is preferred for early diagnosis of PCa, followed by final confirmatory diagnosis through prostate biopsy (8). Radical prostatectomy (RP) is considered the gold standard for treating localized PCa (9). However, biochemical recurrence was high with metastasis diagnosed after 7-8 years in asymptomatic cases (10). Although surgical castration was the standard for androgen deprivation therapy (ADT) (11), hormonal therapies (HT) with luteinizing hormone-releasing hormone agonists(LHRHa), anti-androgens (AA) and combined androgen blockade (CAB) have shown beneficial effects (12).
Efficacy of CAB has been determined in multiple studies in Asian population. A retrospective analysis conducted in 608 Chinese patients with PCa showed superiority of CAB in prolonging the overall survival (OS) and progression free survival (PFS) than castration alone (13). Studies have also reported similar beneficial effects of CAB in men of Asian origin such as Japanese and Filipinos (14). Further, the effects of CAB treatment have also been explored in RP treated high-risk PCa patients in China, where it prolonged PFS (15). With little evidence present in Chinese population, it became imperative to further explore the efficacy and safety of CAB in the huge Chinese male population. Therefore, in the present study, we investigated the treatment pattern and impact of adjuvant HT selection (including CAB, LHRHa and AA) in Chinese patients with high-risk localized and locally advanced PCa,in terms of PSA recurrence and quality of life (QoL) during 2-year follow-up.
Materials and methods
Study design and patient selection
This 2-year, multicenter, prospective, single-arm,observational study aimed at determining the treatment trends and QoL outcomes in patients with localized and locally advanced PCa at 18 centers from major cities in China (Beijing, Shanghai, Guangzhou, Tianjin, Hangzhou,Wuhan, Nanjing, Chengdu, Xi’an and Shenyang).
The inclusion criteria for patients in the study were: 1)age ≥18 years at baseline; 2) histological confirmation of PCa treated by RP and high-risk of recurrence factors(Gleason score ≥8 or preoperative serum PSA≥20 ng/mL)or locally advanced PCa (T≥pT3, N0M0 and any T,N1M0); and 3) immediate administration with adjuvant HT post-surgery. Adjuvant HT with LHRHa (goserelin,leuprorelin, triptorelin) or AA (flutamide, bicalutamide) or CAB was administered after RP, according to investigator’s decision in routine clinical practice as per the 2014 version of the Chinese Guidelines for Prostate Cancer (16).Patients treated with neoadjuvant HT before surgery were excluded from the study.
The study protocol was approved by Institutional Review Boards of all the 18 centers. The study was conducted in accordance with the International Conference on Harmonization guidelines for Good Clinical Practice(ICH-GCP, E6), and Declaration of Helsinki (1964, and its subsequent revisions). All of the patients were required to provide an informed consent before enrolling into the study.
Data collection
Data for the analysis were collected over 4 years, between April 2010 and August 2014. Data on demographics (age,height, weight and other vitals), clinicopathologic parameters (including preoperative clinical stage,preoperative serum PSA, postoperative pathological stage and nodal status, postoperative Gleason score, surgical margin and seminal vesicle involvement) and treatments(including type of adjuvant HT administered and treatment duration) were collected. Whereas the postoperative data including PSA follow-up and QoL were collected using Functional Assessment of Cancer Therapy-Prostate(FACT-P) QoL questionnaire at 12- and 24-months.
Study outcomes
PSA fluctuations are not rare; however, PSA levels gradually decline after 18-24 months of treatment (17). It has been observed that the reference time span of 2 years is a better discriminator for PCa-associated metastases and mortality (18). Therefore, the primary endpoint of the study was to evaluate 2-year PSA recurrence rate of the high-risk localized or locally advanced Chinese PCa patients with immediate postoperative adjuvant HT. The secondary endpoint included determination of the treatment pattern of postoperative adjuvant HT and QoL using FACT-P questionnaire at 12- and 24-months.
PSA recurrence was defined based on the postoperative baseline serum PSA value. As per previous literature,biochemical recurrence (BCR) was defined in terms of PSA. A PSA of ≥0.05 ng/mL, ≥2 rising PSAs of ≥0.05 ng/mL, A PSA of ≥0.20 ng/mL and A PSA of ≥0.40 ng/mL represented 50%, 50%-75%, 76%-90%, and >90% of BCR, respectively over 5-year progression. Among multiple definitions, BCR of 63%-79% was defined as PSA value ≥0.4 ng/mL (19,20). For patients with postoperative baseline serum PSA<0.2 ng/mL, a change in serum PSA of≥0.2 ng/mL at least twice within two years was regarded as PSA recurrence. However, for those with serum PSA≥0.2 ng/mL, recurrence was defined as doubling of baseline serum PSA value at any time within 2 years.
Statistical analysis
Assuming a sample size of 200 patients and 10% drop out,the estimated number of evaluable patients was 180.Assuming a 2-year recurrence rate of 10%, the estimated range of 95% confidence interval (95% CI) as 4.4%, was considered optimal for the conduct of the study.Descriptive statistics was used to present baseline characteristics, wherever applicable. Chi-square test was used for checking statistical significance and P≤0.05 was considered significant. The results of the primary endpoint were presented as percentage and 95% CI. Continuous variables were expressed as mean, median and standard deviation (SD). Frequency tables were used for analyzing categorical data at baseline, 12- and 24-months. Kaplan-Meier analysis was used to calculate the PSA recurrence rate during follow-up. A paired t-test was used to compare the baseline FACT-P score with 12-month and 24-month FACT-P scores. Statistical analysis was performed using SAS software (Version 9.2; SAS Institute Inc., Cary, NC,USA).
Results
Baseline characteristics
During initial screening, 201 patients with PCa were included, of which 192 met the inclusion criteria. The cohort with complete follow-up records included 189 patients with PCa (mean age: 66.9±6.5 years). There were 112 (59.3%) patients with preoperative serum PSA>20 ng/mL. The majority of the patients were in clinical T2 stage [145 (76.7%)] and pathologic T3 stage [118 (62.4%)].Postoperative T-stage escalation was the highest observed in cT2, with 83 (43.9%) cases in the pT3 stage, when compared to preoperative staging. Postoperatively, positive nodes, surgical margin and seminal vesicle involvement were recorded in 23 (12.2%), 69 (36.5%) and 60 (31.7%)patients, respectively. A total of 84 (44.7%) patients had postoperative Gleason score >7, which differed significantly among CAB, LHRHa and AA groups (P=0.0193). Other important demographic and clinicopathological findings are summarized in Table 1.
2-year PSA recurrence rate
Cumulative BCR for 12-month follow-up was 10.5% (95%CI, 6.8%-15.9%), whereas that for 24-month follow-up was 17.4% (95% CI, 10.7%-27.6%) (Figure 1). Among them, the 2-year PSA recurrence rate of CAB, LHRHa and AA subgroups was 15.2% (95% CI, 8.1%-27.7%), 16.1%(95% CI, 4.3%-50.6%) and 19.0% (95% CI, 10.3%-33.3%), respectively. However, comparison of proportions of recurrence rate in CAB group was non-significantly lower compared with AA group (15.2% vs. 19.0%,P=0.5370) and LHRHa (15.2% vs. 16.1%, P=0.9319)group did not demonstrate significant differences, which was probably due to large difference in number of subjects under treatment groups.
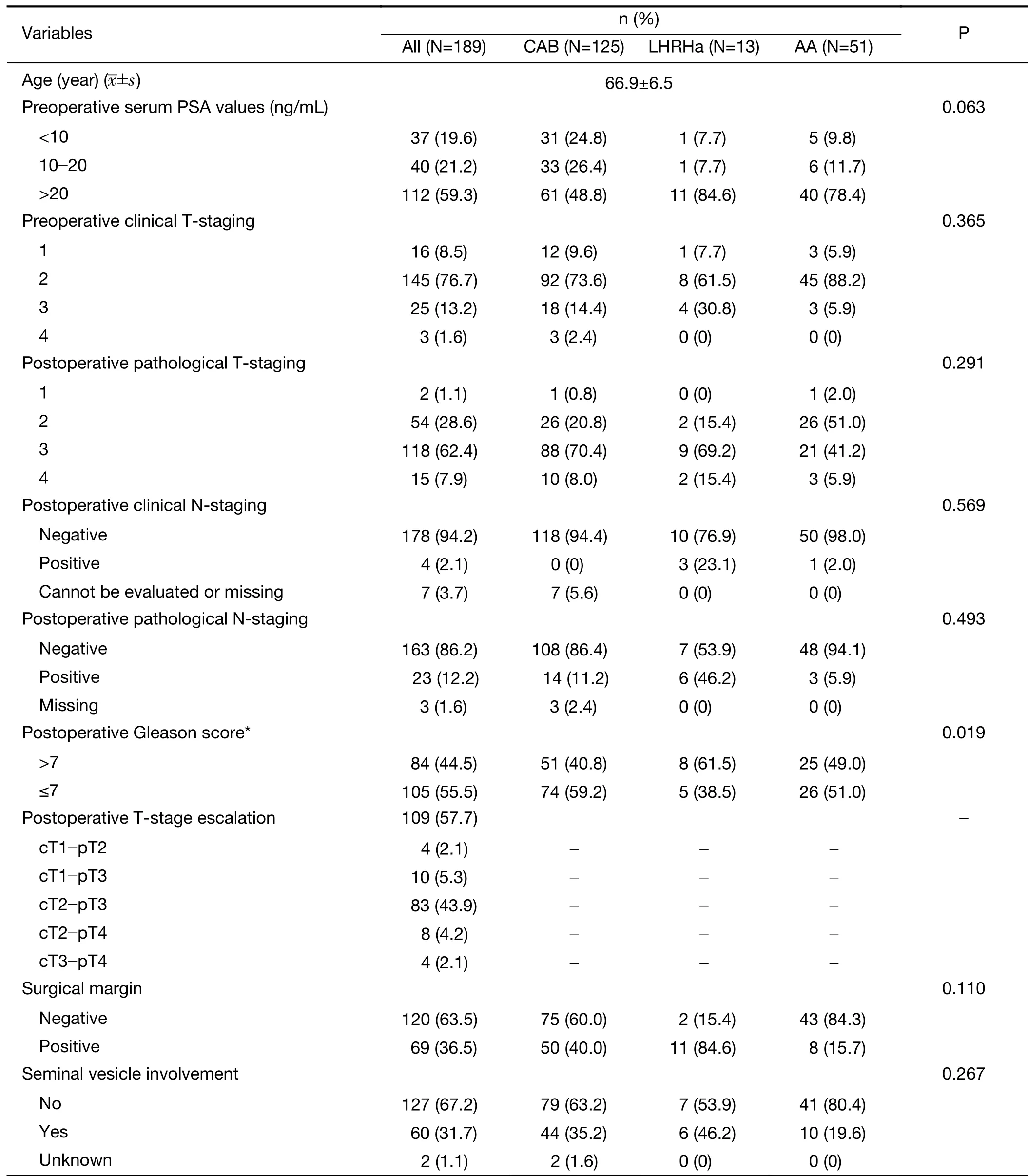
Table 1 Baseline characteristics and postoperative adjuvant HR (N=189)

Figure 1 Two-year prostate-specific antigen (PSA) recurrence rate for prostate cancer cohort. 95% CI, 95% confidence interval.
Table 2 presents the logistic regression analysis (n=175,31 recurrence events) with independent predictors of recurrence rate. Due to missing data values for N staging,Gleason score and seminal vesicle involvement, these data were excluded from the complete dataset in the regression model. Odds of recurrence with CAB therapy were similar to the AA group and LHRHa groups. The findings showed none of the factors was significantly associated with 2-year BCR/PSA recurrence rate.
Postoperative adjuvant HT pattern
Of the 189 patients who underwent post-surgical adjuvant HT, the majority of the patients (66.1%) were prescribed CAB treatment. Only 6.9% and 27.0% of the patient population was treated with monotherapy of LHRHa and AA, respectively. Among 54 patients with pathologic T2 stage, only 48.1% of patients received CAB, compared to 74.6% of patients with pathologic T3 stage. In addition,40.0% of patients with positive margins were also treated with CAB. Of the 60 patients with invasion into seminal vesicle, 35.2% received CAB treatment as given in Table 1.The median time to receive adjuvant HT was 20.0 (range,0.8-27.0) months. The median interval for PSA monitoring was 118 days, and the proportion of patients who received 6 or more PSA tests at 2 years was 79.9%(151/189).
Change in QoL with adjuvant therapy
In the 189 enrolled patients, mean FACT-P score was 65.75±11.00 at baseline, 63.44±9.48 at 12-month and 63.94±9.67 at 24-month, respectively. Seventy patients underwent HT for ≤12 months and 119 patients were treated for >12 months. A total of 138 (73.01%) patients underwent FACT-P QoL questionnaire at 2-year followup. The mean FACT-P score of patients treated with ≤12 months HT at baseline was 69.11±9.48, while those treated for >12 months had the score of 63.96±11.44. The QoL of patients treated with HT for ≤12 months decreased significantly from baseline to 24-month, whereas a significant increase was observed in patients treated with HT for >12 months. At 24-month, patients treated for >12 months had significantly greater FACT-P score compared with patients treated for ≤12 months (65.33±9.05 vs.61.57±10.32, P=0.0270) (Table 3).
Discussion
In recent years, progress in the local treatment of PCa has led to more high-risk localized and locally advanced PCa patients receiving RP. For such patients, adjuvant HT after RP aims to eliminate micro metastases and prevent distant metastases (21), thereby, making the choice of adjuvant treatments an important aspect in the management of such cases. To the best of our knowledge, this prospective observational study was the first multicenter study including 18 centers across China to evaluate the PSA recurrence rates and treatment pattern of adjuvant HT(CAB, LHRHa or AA) in high-risk Chinese patients with PCa, who were treated in accordance to investigator’s decision in routine clinical practice.

Table 2 Logistic regression of independent factors affecting recurrence rate (N=175)
Although over the years, there has been advancement in the diagnostic modalities for PCa, pathological status of tumor is still underestimated in 10%-50% of the cases prior to surgery (22,23) and reports suggest a T stage escalation (to pT3) in about 43% of patients after RP (24).A retrospective analysis in 106 Japanese patients with T3N0M0 PCa (preoperative PSA>20 ng/mL) reported high recurrence rate (87.1%) at 2-year follow-up (25).Another study in French patients reported positive correlation of pT3 staging of high-risk PCa with biochemical recurrence (26). In our study, 109 (57.7%) out of 189 patients had a postoperative pathologic advancement, with 83 patients upgraded from cT2 to pT3.In 118 pT3 patients, the proportion of patients receiving CAB was 74.6%. Due to high risk of recurrence, clinicians need to draw more attention towards postoperative pathological T stage escalation as it might directly affect the choice of postoperative treatment.
Due to lack of success in the treatment of locally advanced PCa patients by single treatments like RP (27,28),the need for multimodal treatment strategies in combination with radiotherapy (RT) (29,30) and HT(31,32) has risen. In the western population, adjuvant RT after RP has shown low rate of clinical recurrence and good tolerability, even in cases with aggressive pathological PCa(33). However, due to their serious adverse effects (34,35)and challenge in relevant technical skills, we did not include them in the present study. Moreover, evidence from previous studies has supported that compared to western population, effective and significant results can be achieved with ADT using HT in high-risk PCa patients from Asian ethnicity (14,36). Therefore, we attempted to depict a real-world practice in China for the management of high-risk PCa patients using adjuvant HT after RP.

Table 3 Change of FACT-P QoL score in patients treated for ≤12 months and >12 months
Previous studies conducted globally have emphasized on the role of adjuvant HT in PCa after RP. A randomized controlled trial (RCT) conducted in US reported a 5-year OS rate of 96% and 5-year PSA recurrence-free survival of 92.5% in high-risk PCa patients treated with RP + adjuvant HT (37). In Japanese patients with pT3N0 PCa, immediate adjuvant HT after RP showed clinical recurrence in only 3 out of 105 patients and PFS without recurrence in 96.0%and 93.0% of patients at 5- and 10-year, respectively (24).The present study showed a low PSA-recurrence rate at 12-and 24-months (10.5% and 17.4%). The results of our study were consistent with the study results of Chang et al.(15), which was also conducted in Chinese patients with high-risk PCa. This indicated that adjuvant HT may be feasible in routine clinical practice to prevent PSA recurrence.
Though multiple studies are conducted on the effect of adjuvant HT after RP, the choice and duration of treatment with HTs is highly debatable. Study by Dorff et al. in high-risk PCa showed high survival rates with CAB(goserelin + bicalutamide) administered for 2 years (37). A 16-year prospective trial reported high rates of OS (77.0%)and cancer-specific survival (86.3%) after 8-year follow-up(38). The CU1005 involving 209 Chinese patients compared the treatment effect of 9-month adjuvant HT(with CAB or bicalutamide 150 mg), after RP. In comparison to bicalutamide group, patients treated with CAB therapy had lower recurrence rate (19.6% vs. 37.3%)and longer recurrence-free survival after a median followup of 27 months (15). The difference in recurrence rates in the present study might be due to larger proportion of patients receiving CAB and longer duration of adjuvant HT administration. However, limited studies report the comparison between long-term and short-term adjuvant HT in terms of OS, PSA failure and disease-specific survival (DSS). The long-term and short-term therapies did not differ significantly in terms of OS rate (65% vs.61%, P=0.53), PSA failure (55% vs. 53%, P=0.99) and DSS(96% vs. 97%, P=0.72) (39). In another study, significant difference was observed in the 5-year biochemical PFS rates between short- (<36 months) and long-term (≥36 months) ADT (84.0% vs. 96.2%; P=0.04). However, the difference in OS was not significant (86.8% vs. 94.4%;P=0.16) (40). In our study, the majority of the patients(66.6%) received CAB, followed by AA (27.0%) and LHRHa (6.9%) for median 20 months. At 2-year, the recurrence rate was lower with CAB (15.2%) than that reported with LHRHa (16.1%) or AA (19.0%), which is consistent with previously published evidence, indicating that CAB is a more suitable option for adjuvant HT after RP in high-risk Chinese patients with PCa. In addition, a longer duration of HT (>12 months) was associated with significantly greater improvement in QoL on the FACT-P score, confirming that long-term HT improved not only efficacy, but also the QoL improvement in advanced PCa patients. Therefore, it suggests that long-term HT treatment should be recommended in real-world practice for PCa management.
As per the 2016 European Association of Urology (EAU)guidelines, regular PSA monitoring is an important step in the prevention and treatment of recurrence (15). The median time interval for PSA monitoring in our study was 118 days during the 2-year follow-up, indicating that PSA monitoring after RP in China was in line with international guidelines.
Adverse reactions in patients receiving HT may affect the QoL (41). FACT-P is considered a reliable measure for QoL evaluation in PCa patients (42,43). In our study, an increase in the FACT-P score (by 1.37 points) after 24 months indicated an improvement in QoL when postoperative adjuvant HT was continued for >12 months,compared to ≤12-month treatment. Therefore, long-term adjuvant HT improves the QoL in patients with high-risk PCa and enhances physician’s confidence in postoperative adjuvant HT in clinical practice.
Our study has a few limitations. Firstly, since the present study is a real-world observational study, the number of patients receiving adjuvant HT was highly varied with majority of the patients receiving CAB. Due to this high discrepancy in number, it was not possible statistically to compare the difference between the effectiveness of different adjuvant treatment regimens. Secondly, we did not perform any imaging test during this study as similar published observational studies have not used imaging techniques to analyze outcomes in patients receiving adjuvant treatment after prostatectomy (44,45). Thirdly,serum testosterone levels were not checked for the analysis.This was an observational study carried out in China, and as per Chinese guidelines, evaluation of serum testosterone levels is not mandatory in the real-world clinical practice in China (16). Similar studies in China and other countries did not evaluate the serum testosterone levels in patients with localized or locally advanced PCa after prostatectomy(46,47). Fourthly, we experienced high dropout rate in this study. However, we believe the data are still relevant as QoL was analyzed as a secondary outcome. Moreover, a published observational study on PCa patients reported with similar dropout rate, i.e., 29% (48). Fifthly, the duration of our study was 24-month, which was comparatively shorter than some previous studies. A study recording the survival outcomes (OS, PFS and cancerspecific survival) for longer duration would provide more robust outcomes.
Conclusions
Adjuvant CAB after RP may be considered as an effective treatment for patients with high-risk localized and locally advanced PCa in China, as it demonstrated the trend of decreasing in 2-year PSA recurrence rate compared with adjuvant AA or LHRHa, in Chinese patients with high-risk localized and locally advanced PCa. However, the study did not reveal any significant statistical difference between the groups in terms of decreasing 2-year PSA recurrence. In addition, long-term adjuvant HT (>12 months) improved the QoL in these patients, which could also indicate that long-term CAB therapy caused significantly greater improvement in QoL than short-term CAB therapy.Further RCTs including patients with similar and comparable demographics must be performed to provide further evidence and establish our findings.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
杂志排行
Chinese Journal of Cancer Research的其它文章
- Burden of colorectal cancer in China, 1990-2017: Findings from the Global Burden of Disease Study 2017
- Immune signature profiling identified prognostic factors for gastric cancer
- Correlation of radiotherapy with prognosis of elderly patients with hormone receptor-positive breast cancer according to immunohistochemical subtyping
- Impact of crizotinib on long-term survival of ALK-positive advanced non-small-cell lung cancer: A Chinese multicenter cohort study
- Hexokinase II promotes the Warburg effect by phosphorylating alpha subunit of pyruvate dehydrogenase
- Mutant p53 increases exosome-mediated transfer of miR-21-3p and miR-769-3p to promote pulmonary metastasis