Correlation of radiotherapy with prognosis of elderly patients with hormone receptor-positive breast cancer according to immunohistochemical subtyping
2019-07-13XiangchengZhiXiaonanYangTengPanJingjingLiuXiaoChenLipingLouZhendongShiJinZhang
Xiangcheng Zhi, Xiaonan Yang, Teng Pan, Jingjing Liu, Xiao Chen, Liping Lou, Zhendong Shi,Jin Zhang
Department of Breast Cancer, Tianjin Medical University Cancer Institute & Hospital, National Clinical Research Center of Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin’s Clinical Research Cancer for Cancer, Tianjin 300060, China
Abstract Objective: The present study examined the effect of radiotherapy on recurrence and survival in elderly patients with hormone receptor-positive early breast cancer.Methods: A retrospective analysis of 327 patients aged ≥65 years, with stage I-II, hormone receptor-positive breast cancer who underwent breast-conserving surgery and received endocrine therapy (ET) or radiotherapy plus endocrine therapy (ET+RT) was performed. Both groups were divided into luminal A type and luminal B type subgroups. Evaluation criteria were 5-year disease-free survival (DFS), local relapse rate (LRR), overall survival(OS), and distant metastasis rate (DMR).Results: There were significant differences in 5-year DFS [hazard ratio (HR)=1.59, 95% confidence interval(95% CI), 1.15-2.19; P=0.005] and LRR (HR=3.33, 95% CI, 1.51-7.34; P=0.003), whereas there were no significant differences in OS and DMR between ET group and ET+RT group. In luminal A type, there was no significant difference in 5-year DFS, LRR, OS and DMR between ET group and ET+RT group. In luminal B type,there were statistically significant differences in 5-year DFS (HR=2.19, 95% CI, 1.37-3.49; P=0.001), LRR(HR=5.45, 95% CI, 1.65-17.98; P=0.005), and OS (HR=1.75, 95% CI, 1.01-3.05; P=0.048) between ET group and ET+RT group. In the ET group, there were significant differences between luminal A type and luminal B type in 5-year DFS (HR=1.84, 95% CI, 1.23-2.75; P=0.003) and OS (HR=1.76, 95% CI, 1.07-2.91; P=0.026).Conclusions: After breast-conserving surgery, radiotherapy can reduce the LRR and improve the DFS and OS of luminal B type elderly patients, whereas luminal A type elderly patients do not benefit from radiotherapy.Without radiotherapy, luminal A type patients have better DFS and OS than luminal B type patients.
Keywords: Breast-conserving surgery; disease-free survival; endocrine therapy; hormone receptor-positive;overall survival; radiotherapy
Introduction
Breast cancer is currently the most common cancer among Chinese women, accounting for 12.2% of all newly diagnosed breast cancers and 9.6% of all deaths from breast cancer worldwide. Adopting measures to improve the health of breast cancer patients are important (1). Studies have shown that breast-conserving surgery is as effective as modified radical mastectomy with respect to local tumor control and disease-free survival (DFS) in Chinese patients with primary breast cancer (2). For most women with early breast cancer, the standard treatment after breastconserving surgery is radiotherapy plus endocrine therapy(ET+RT) (3); however, the absolute benefit of radiotherapy differs among women (4), and may decrease with increasing age (5). The prognosis of elderly breast cancer patients is usually better than that of young patients. Elderly patients with breast cancer have special physiological characteristics,such as low tumor cell proliferation rates, low histological grades, low expression of human epidermal growth factor receptor-2 (HER2), with mostly positive estorgen receptor(ER) and/or progesterone receptor (PR) and a good prognosis (6). The proportion of luminal A tumors in elderly patients is very high, and luminal A breast cancer is associated with better DFS and overall survival (OS) than other molecular subtypes (7).
Endocrine therapy is the most important adjuvant treatment for hormone receptor-positive breast cancer patients and can significantly improve DFS and reduce recurrence rates (8) with minimal side effects. Breast cancer patients who respond to endocrine therapy may have lower benefits of radiotherapy. Elderly patients have their own characteristics and frequently suffer from a variety of underlying diseases, showing an increased rate of postoperative complications (9). It is necessary to address the actual needs of the patient rather than maximizing adjuvant treatments to prevent the occurrence of side effects (10).
Here, we performed a retrospective study including patients aged ≥65 years, with stage I-II, hormone receptorpositive breast cancer who underwent endocrine therapy after breast-conserving surgery, and evaluated the impact of radiotherapy on breast cancer recurrence and survival.
Materials and methods
Research patients
Patients were selected from Tianjin Cancer Hospital, and female patients aged ≥65 years, with hormone receptorpositive stage I-II breast cancer who met the inclusion criteria were included between January 2008 and December 2013. The final analysis included 327 eligible patients. The inclusion criteria were: 1) according to the indications for breast-conserving surgery, patients who underwent breast conserving surgery and partial lymph node surgery (11); 2) postoperative pathology was T1-2N0-1M0 in stage I-II; 3) hormone receptor-positive breast cancer; 4) clear pathological negative margins (≥2 mm) (12); 5) received endocrine therapy; 6) confirmed by postoperative pathology for breast primary cancer; and 7)aged ≥65 years. The exclusion criteria were: 1) other concurrent malignant tumors; 2) bilateral breast cancer or multicenter breast cancers; 3) metastases; 4) endocrine therapy could not be performed because of side effects or personal causes; 5) incomplete clinical pathology or followup data; 6) received neoadjuvant chemotherapy; 7) HER2 positive luminal B who received targeted therapy; or 8)prior history of breast cancer.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the responsible committee on human experimentation(institutional and national). The protocol for the research project was approved by the Ethics Committee of Tianjin Medical University Cancer Institute & Hospital within which the work was undertaken and it conformed to the provisions of the Declaration of Helsinki (as revised in Fortaleza, Brazil, October 2013).
Grouping
Patients were divided into two groups: the endocrine therapy (ET) and ET+RT groups. The ET group was divided into luminal A type (108 cases) and luminal B type(81 cases) subgroups. The ET+RT group was divided into luminal A type (70 cases) and luminal B type (68 cases)subgroups.
Evaluation criteria
DFS was defined as the time from first treatment to local recurrence, distant metastasis, death, or termination of follow-up. Local relapse rate (LRR) was defined as the time from first treatment to local recurrence. OS was defined as the time from first treatment to any cause of death or termination of follow-up. Distant metastasis rate (DMR)was defined as the time from first treatment to distant metastasis.
Follow-up
Patients were followed up from the date of surgery until November 2018 or until death. Follow-up methods included access to outpatient and inpatient medical records,telephone calls, letters, and home visits. Follow-up evaluations included whether the patient had recurrence and metastasis, especially local recurrence and distant metastasis time, DFS and OS. Mammography and cervical thoracic computed tomography (CT) were performed every 6 months. Whole body color Doppler ultrasound,whole body bone scan, and breast magnetic resonance imaging (MRI) were performed every year. Within 2 years after treatment, the patients were reviewed every 3 months.Within 5 years, they were reviewed every 6 months. After 5 years, they were reviewed every year. Endocrine drug compliance and side effects were assessed each time.
Data collection
First, immunohistochemical intrinsic subtyping (The diagnostic criteria were defined according to the 2013 St.Gallen International Breast Cancer Conference.): Luminal A: ER+ and/or PR+, HER2-, Ki-67 <20%; Luminal B:HER2-, ER+ and/or PR <20%, HER2-, Ki-67 ≥20%.Second, treatment: All patients underwent breastconserving surgery, of which 121 (37.0%) underwent axillary lymph node dissection (ALND), and 206 (63.0%)received sentinel lymph node biopsy (SLNB). In the entire cohort, 189 patients (57.8%) received single ET and 138 patients (42.2%) received ET+RT. Third, radiotherapy technology: Conventional radiotherapy technology was used in all patients. The current “standard mode” for postoperative breast-conserving radiotherapy is conventional total-dose radiotherapy (50 Gy/25 f/35 d),followed by sequential tumor bed replenishment (10-16 Gy/5-8 f). Fourth, endocrine therapy: Third-generation aromatase inhibitors (AIs) including non-steroidal AIs(anastrozole, letrozole) and steroidal AIs (exemestane) were used. Letrozole was administered orally at 2.5 mg daily for 5 years. Anastrozole was administered orally at 1.0 mg daily for 5 years. Exemestane was administered orally at 25 mg daily for 5 years (13).
Complete clinical and pathological data and follow-up data were available in all cases. The collected clinical and pathological data included pathological type, pathological stage, histological grade, lymph node status, axillary procedure, ER/PR/Her2/P53/Ki-67, endocrine therapy,and whether the patient underwent radiotherapy. Complete follow-up data included whether the patient had any recurrence, metastasis time and location, and time of death.
Statistical analysis
Statistical analysis was performed using SAS software(Version 9.3; SAS Institute Inc., Cary, USA). Qualitative data were expressed as n (%). The Kaplan-Meier method was used for survival analysis, and the survival rates were calculated at different time points. The Cox proportional hazard regression model was used to analyze the following data: 1) DFS, LRR, OS, and DMR of “all patients”; 2)factors affecting the DFS, LRR and OS in the “luminal B type”; and 3) factors affecting the DFS and OS of patients in the “ET group”. The stepwise method was used to filter variables, introduce and remove variables at the significance level α=0.05, and calculate the hazard ratio (HR) and its 95% confidence interval (95% CI). According to different study endpoints (DFS, LRR, OS and DMR), the log-rank test was used to compare the four groups (ET group luminal A type, ET group luminal B type, RT+ET group luminal A type, and RT+ET group luminal B type), and a survival curve was drawn. P<0.05 was considered statistically significant.
Results
Clinicopathological features
There were 327 patients with a median age of 72 (66-78)years (≥65 years), including 247 patients (75.5%) with T1N0M0, 14 patients (4.3%) with T1N1M0, 55 patients(16.8%) with T2N0M0, and 11 patients (3.4%) with T2N1M0. There were 25 lymph node-positive patients(7.6%) and 246 patients (75.2%) with invasive ductal carcinoma. There were 162 patients (49.5%) with histological grade I, 153 patients (46.8%) with histological grade II, and 12 patients (3.7%) with histological grade III.There were 178 patients (54.4%) with luminal A and 149 patients (45.6%) with luminal B (Four groups are shown in Table 1).
Prognosis analysis
The median follow-up time was 5.83 y ears. The median survival time was 9.17 years. Of 327 patients, 113 (34.6%)died, 15 (4.6%) died of breast cancer, and 98 (30.0%) died of other diseases or accidents. Of 189 patients in the ET group, 67 (35.4%) died, 9 (4.8%) died of breast cancer, and 58 (30.7%) died of other diseases or accidents. Of 138 patients in the ET+RT group, 46 (33.3%) died, 6 (4.3%)died of breast cancer, and 40 (29.0%) died of other diseases or accidents. Local recurrence occurred in 37 patients(11.3%), of which 29 (8.9%) were in the ET group and 8(2.4%) were in the ET+RT group. Distant metastases occurred in 15 patients (4.6%), of which 9 (2.8%) were in the ET group and 6 (1.8%) were in the ET+RT group.
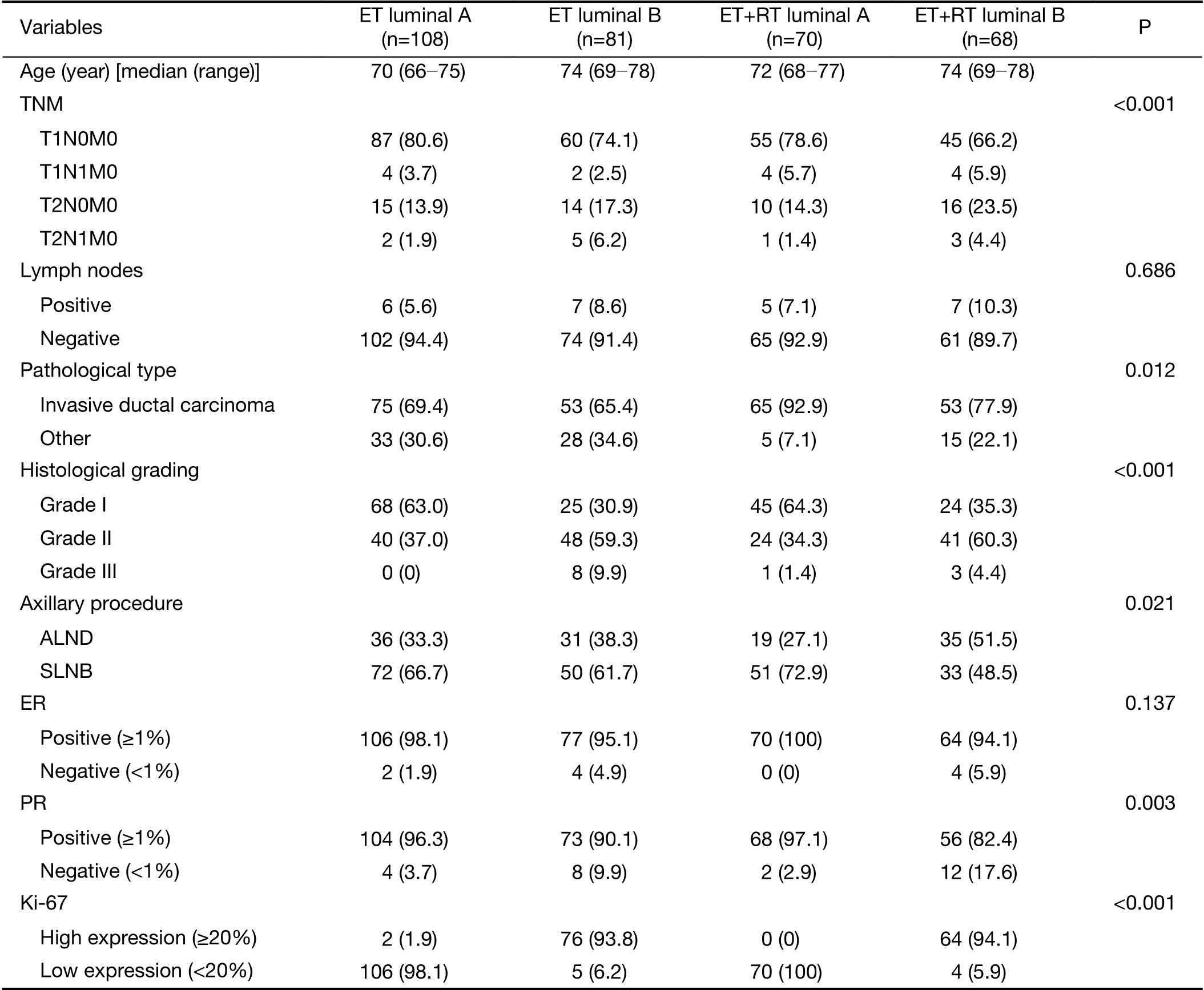
Table 1 Patients’ characteristics (N=327)
There were significant differences in 5-year DFS between the ET group (69.8%) and ET+RT group (76.1%)(HR=1.59, 95% CI, 1.15-2.19; P=0.005). In luminal A type, there was no significant difference in the 5-year DFS between the ET group (72.0%) and the ET+RT group(72.0%) (P=0.293). In luminal B type, the 5-year DFS differed significantly between the ET group (68.0%) and ET+RT group (73.0%) (HR=2.19, 95% CI, 1.37-3.49;P=0.001). In the ET group, there were significant differences in DFS between luminal A type and luminal B type (HR=1.84, 95% CI, 1.23-2.75; P=0.003).
There were significant differences in 5-year LRR between the ET group (8.9%) and the ET+RT group(3.0%) (HR=3.33, 95% CI, 1.51-7.34; P=0.003). In luminal A type, there was no significant difference in the 5-year LRR between the ET group (6.9%) and the ET+RT group(3.0%) (P=0.101). In luminal B type, the 5-year LRR differed significantly between the ET group (8.5%) and the ET+RT group (3.0%) (HR=5.45, 95% CI, 1.65-17.98;P=0.005). No significant difference in LRR was observed in the ET group between luminal A type and luminal B type(P=0.220) (5-year DFS and LRR are shown in Table 2;Kaplan-Meier survival curves are shown in Figure 1-3).

Table 2 Comparison of 5-year DFS and LRR
There were no significant differences in 5-year OS between the ET group (80.0%) and the ET+RT group(77.0%) (P=0.149). The 10-year predicted OS rates were 30.0% in the ET group and 50.0% in the ET+RT group,and the difference was not statistically significant(HR=1.10, 95% CI, 0.69-1.75; P=0.691). In luminal A type, there was no significant difference in the 5-year OS between the ET group (80.0%) and the ET+RT group(82.0%) (P=0.793). In luminal B type, the 5-year OS differed significantly between the ET group (77.0%) and the ET+RT group (78.0%) (HR=1.75, 95% CI, 1.01-3.05;P=0.048). In the ET group, there were significant differences in 5-year OS between luminal A type and luminal B type (HR=1.76, 95% CI, 1.07-2.91; P=0.026).

Figure 1 Disease-free survival (DFS) of endocrine therapy (ET)group and radiotherapy plus endocrine therapy (ET+RT) group.ET group and ET+RT group [hazard ratio (HR)=1.59, 95%confidence interval (95% CI), 1.15-2.19; P=0.005].
There were no significant differences in 5-year DMR between the ET group (2.5%) and ET+RT group (2.7%)(P=0.580). In luminal A type, there was no significant difference in the 5-year DMR between the ET group(2.0%) and the ET+RT group (4.4%) (P=0.988). In luminal B type, there was no significant difference in 5-year DMR between the ET group (4.4%) and the ET+RT group(4.0%) (P=0.307). No significant difference in DMR was observed in the ET group between luminal A type and luminal B type (P=0.064) (5-year OS and DMR are shown in Table 3; Kaplan-Meier survival curves are shown in Figure 4-6).
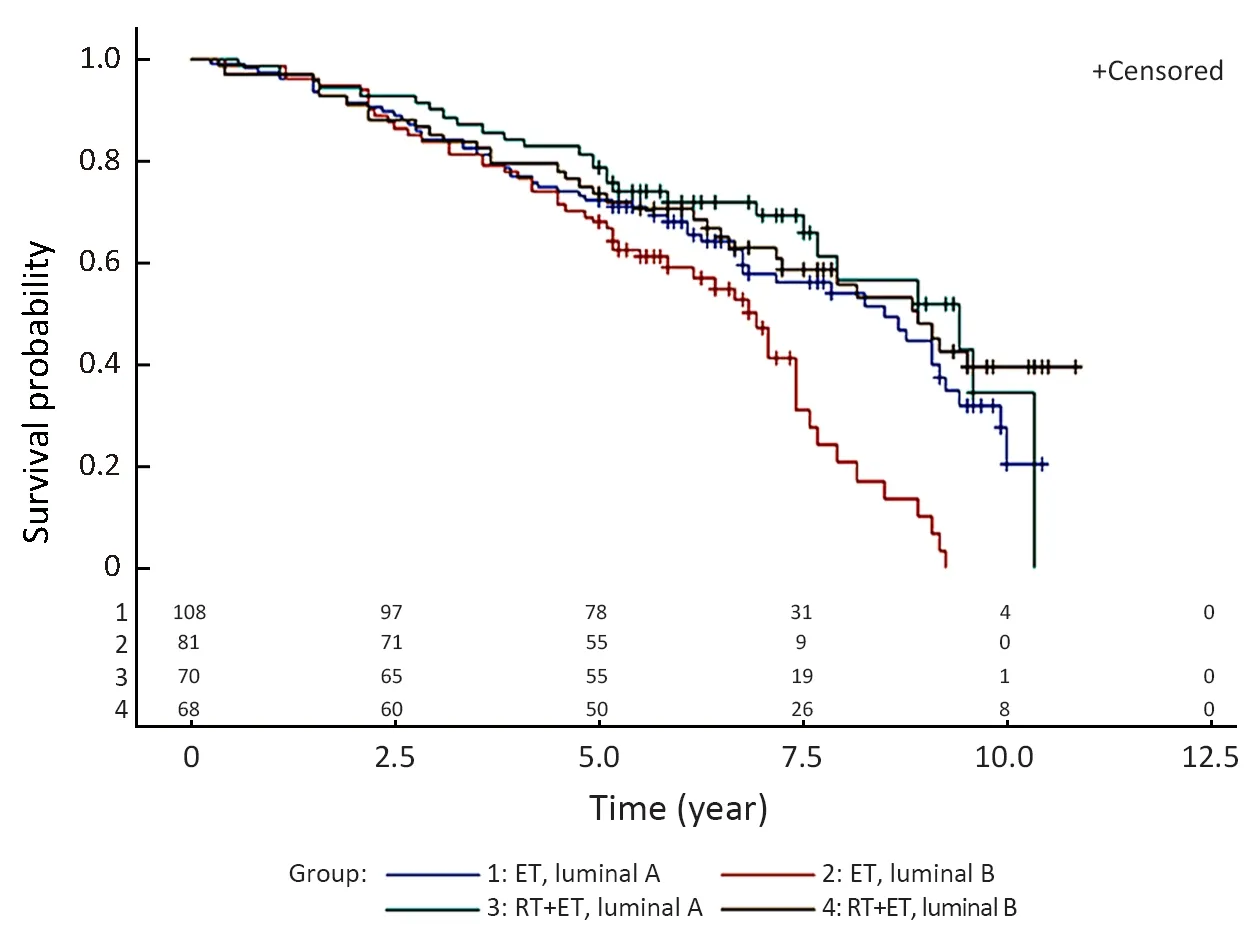
Figure 2 Disease-free survival (DFS) of four groups. Luminal A type [hazard ratio (HR)=1.28, 95% confidence interval (95% CI),0.81-2.04; P=0.293]. Luminal B type (HR=2.19, 95% CI,1.37-3.49; P=0.001). Endocrine therapy (ET) group (HR=1.84,95% CI, 1.23-2.75; P=0.003).
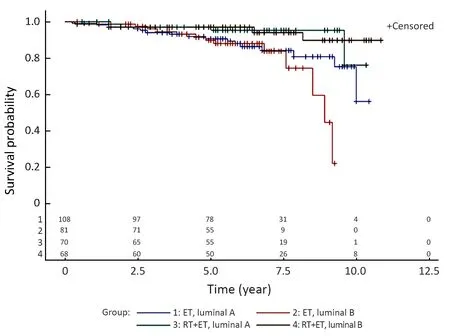
Figure 3 Local relapse rate (LRR) of four groups. Luminal A type[hazard ratio (HR)=2.51, 95% confidence interval (95% CI),0.84-7.52; P=0.101]. Luminal B type (HR=5.45, 95% CI,1.65-17.98; P=0.005). Endocrine therapy (ET) group (HR=1.62,95% CI, 0.75-3.49; P=0.220).
The Cox proportional hazard regression model was used to analyze the factors affecting DFS, LRR, OS and DMR of “all patients”. According to Cox proportional hazard model analysis, group (radiotherapy or not), molecular type, age, pathological type, TNM stage, and axillary procedure were independent risk factors for DFS; group(radiotherapy or not), TNM stage and axillary procedure were independent risk factors for LRR; age, pathological type and lymph nodes were independent risk factors for OS; no independent risk factors for DMR were identified in the Cox proportional hazard model.
The Cox proportional hazard regression model was used to analyze factors affecting DFS, LRR and OS in “luminal B type”. According to Cox proportional hazard model analysis, group (ET or ET+RT), age, pathological type,histological grade, axillary procedure, and lymph nodes were independent risk factors for DFS; histological grade and axillary procedure were independent risk factors for LRR; age, pathological type and lymph nodes were independent risk factors for OS.
The Cox proportional hazard regression model was used to analyze factors affecting DFS and OS in patients in “ET group”. According to Cox proportional hazard model analysis, molecular type, pathological type and lymph nodes were independent risk factors for DFS; molecular type, pathological type, and lymph nodes were independent risk factors for OS.
Discussion
In the present study, the effect of radiotherapy on the prognosis of hormone receptor-positive breast cancer patients after breast-conserving surgery was not consistent with that reported in several international studies. AmongPRIME II (14) subjects with early breast cancer who were 65 years old or older with high ER expression, there were significant differences in terms of recurrence rate, whereas there was no significant difference in the DMR or OS. The CALGB 9343 (15) study suggested that the LRR of the Tamoxifen (TAM) plus radiotherapy group was lower than that of the single TAM group, but the difference between the DMR and the OS was not statistically significant.Tinterri (16) studied early breast cancer patients aged 55-75 years, and concluded that there were no statistically significant differences in in-breast-recurrences and mortality between the two groups.
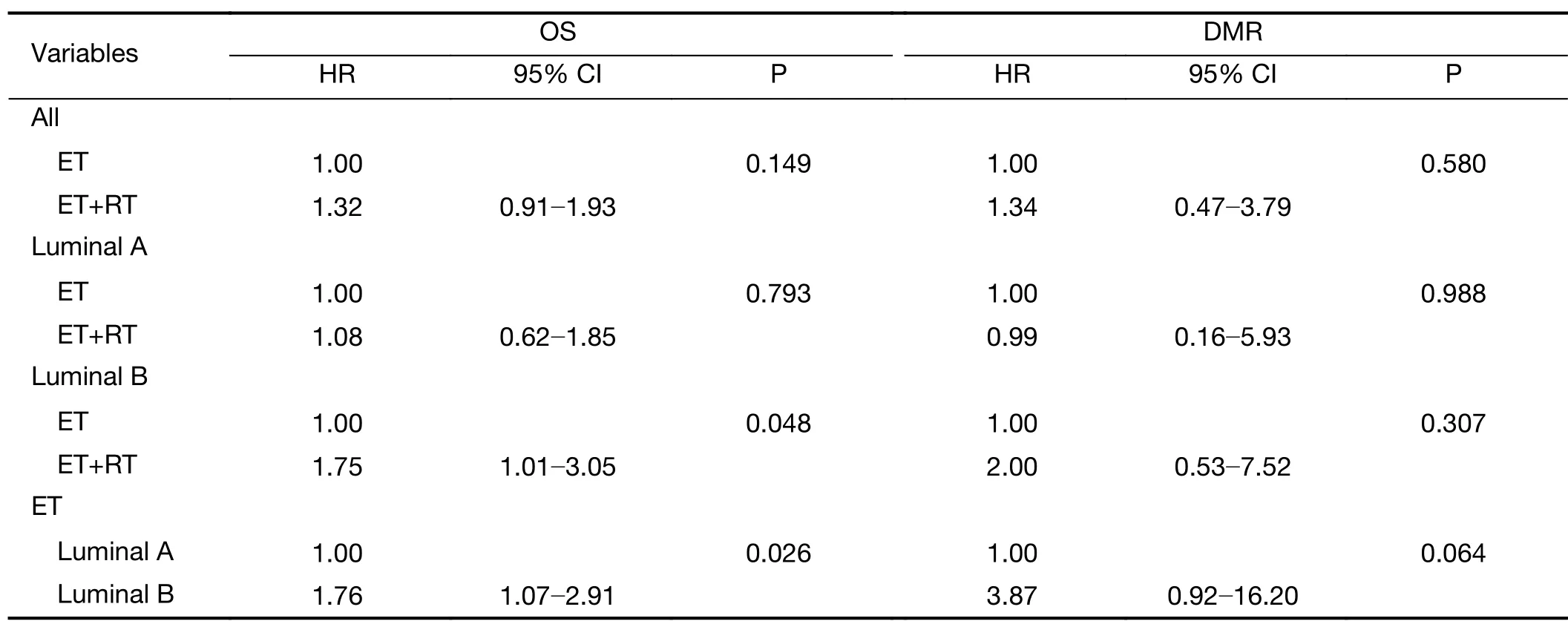
Table 3 Comparison of 5-year OS and DMR

Figure 4 Overall survival (OS) of endocrine therapy (ET) group and radiotherapy plus endocrine therapy (ET+RT) group. ET group and ET+RT group (HR=1.32, 95% CI, 0.91-1.93;P=0.149).
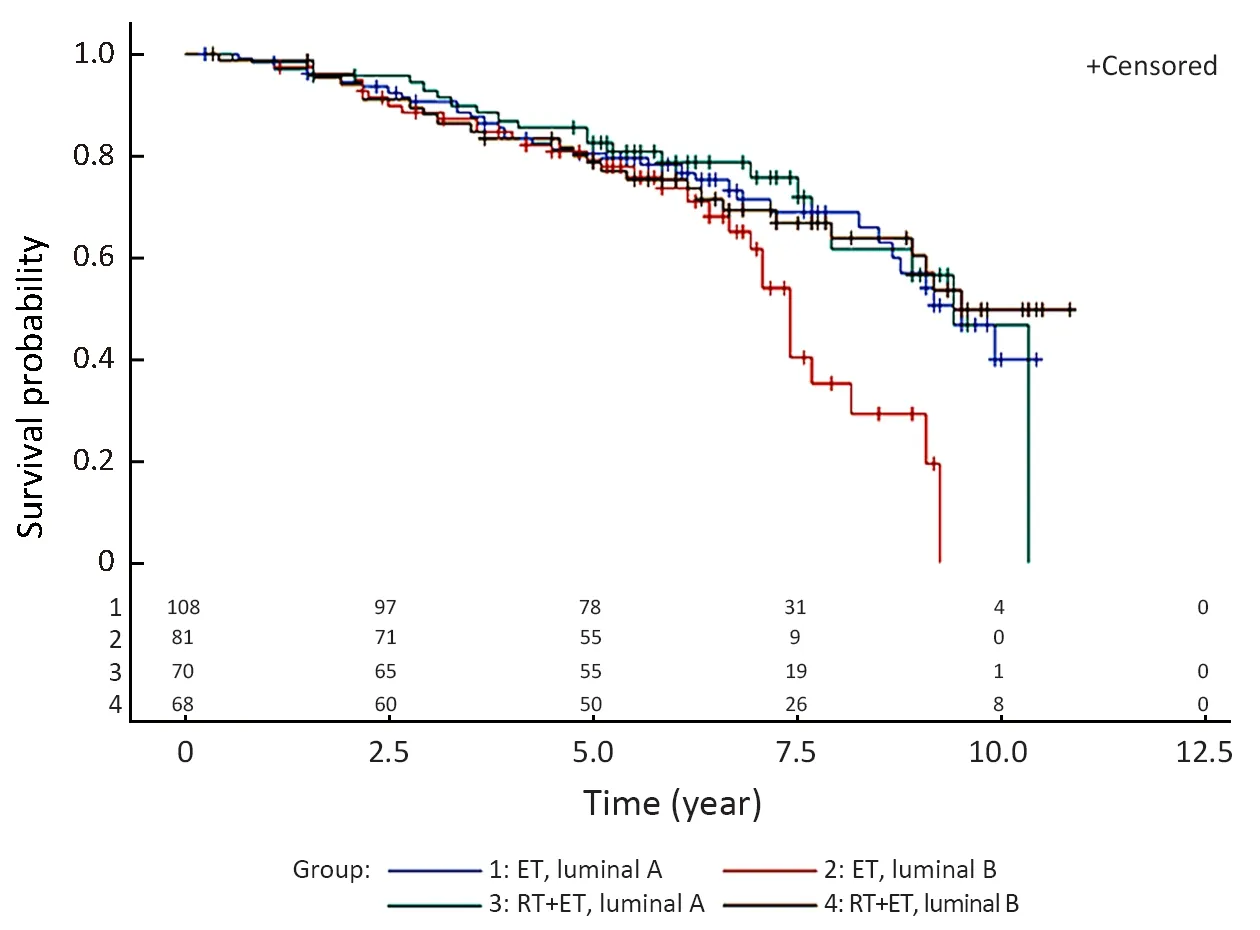
Figure 5 Overall survival (OS) of four groups. Luminal A type[hazard ratio (HR)=1.08; 95% confidence interval (95% CI),0.62-1.85; P=0.793). Luminal B type (HR=1.75, 95% CI,1.01-3.05; P=0.048). Endocrine therapy (ET) group (HR=1.76,95% CI, 1.07-2.91; P=0.026).
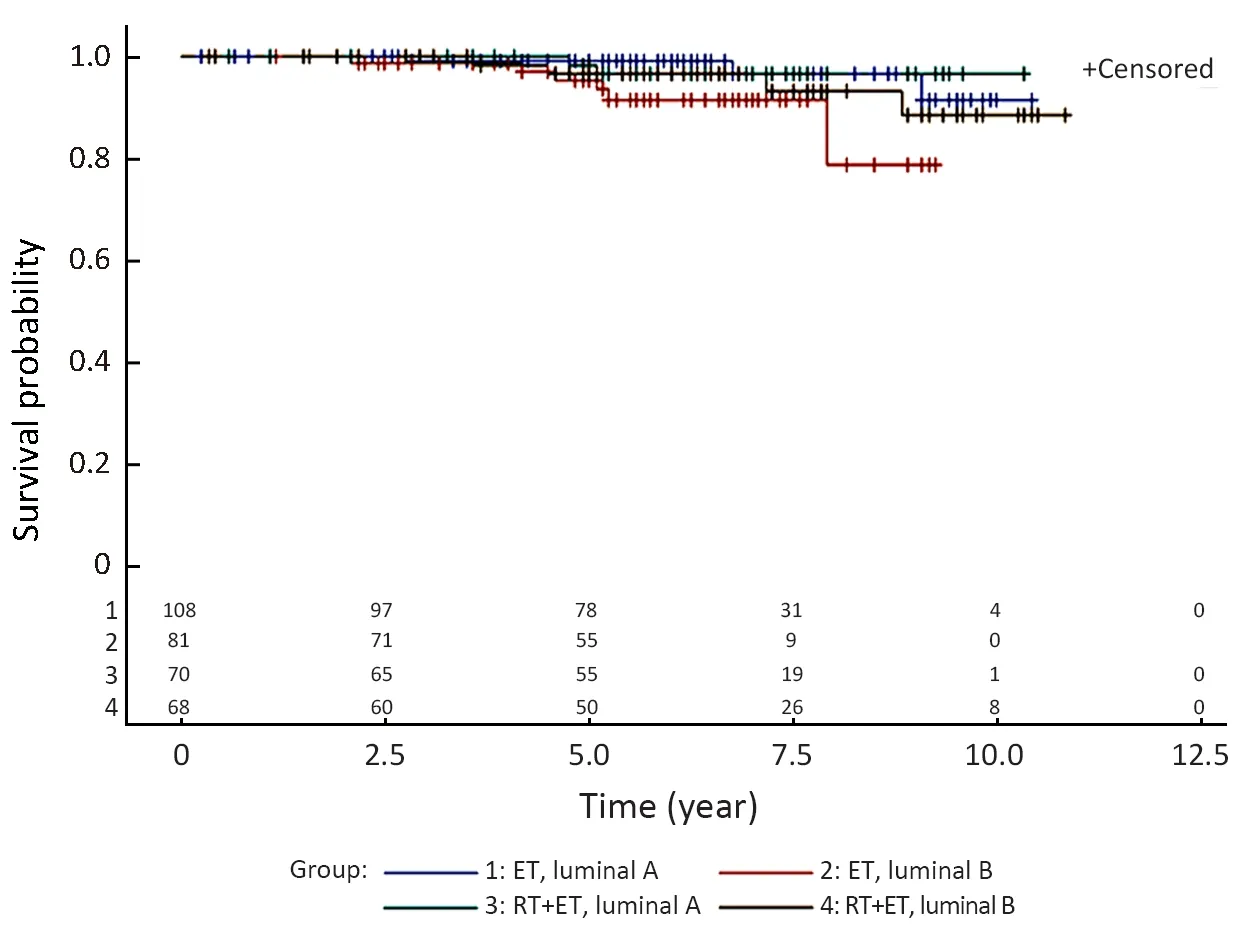
Figure 6 Distant metastasis rate (DMR) of four groups. Luminal A type [hazard ratio (HR)=0.99, 95% confidence interval (95%CI), 0.16-5.93; P=0.988). Luminal B type (HR=2.00, 95% CI,0.53-7.52; P=0.307). Endocrine therapy (ET) group (HR=3.87,95% CI, 0.92-16.20; P=0.064).
Unlike several internationally important studies, our study performed subgroup analysis according to luminal type, and investigated the effects of radiotherapy on elderly patients with luminal B type or luminal A type, which provided more specific conclusions. In addition, the results of luminal A type and luminal B type were not consistent,suggesting that the appropriate treatment can be selected according to luminal type for elderly hormone receptorpositive patients. The study results also showed that luminal A patients have better DFS and OS than luminal B patients after breast-conserving surgery without radiotherapy. These findings were consistent with those of several international trials. Anderson et al. (17), Liu et al.(18) and Chen et al. (19) found that luminal A patients have a better prognosis, with the lowest LRR compared with other subtypes.
Many international studies used TAM as the endocrine drug. However, in the last few decades, third-generation AIs including non-steroidal AIs (anastrozole, letrozole) and steroidal AIs (exemestane) were approved, and a large number of trials comparing third-generation AIs with TAM concluded that in postmenopausal breast cancer patients, AIs are considerably more effective than TAM. A study (20) showed that the efficacy of letrozole and anastrozole is superior to that of TAM for postmenopausal patients in terms of prolonging time to treatment failure,increasing DFS, and decreasing the metastatic rate.Another study (21) showed that the combination regimen of chidamide plus exemestane is generally well tolerable for hormone receptor-positive patients, and progress has been made in endocrine therapy.
The NCIC CTG MA.27 trial (22) established the status of third-generation AIs as first-line treatment for postmenopausal patients with ER+ breast cancer. On the other hand, TAM has certain side effects that increase the risk of discontinuation. Owusu et al. (23) showed that 49%of patients discontinue TAM before the completion of 5 years, with an increase in the Charlson comorbidity index and an increase in the number of cardiopulmonary comorbidities at 3 years. Compared with TAM, the most obvious side effect of AIs is loss of bone mineral density and fracture. Therefore, our medical center adds bisphosphonate to endocrine therapy and evaluates endocrine drug compliance and side effects. No patients discontinued AIs before the completion of 5 years.
Common factors affecting breast cancer prognosis include age, lymph node status, TNM, histological grade,axillary procedure, pathological type, HER2 status,molecular type, and other factors. We used the Cox proportional hazard regression model to analyze the factors affecting the DFS, LRR, OS and DMR.
In Tianjin Cancer Hospital, approximately 15,000 patients received modified radical mastectomy between 2008 and 2013. Approximately 3,000 patients received breast-conserving surgery, among which approximately 20% are patients aged ≥65 years. This may be related to a lower inclination to receive breast-conserving surgery for elderly patients. Doctors need to choose the appropriate treatment according to the patients’ preference.
In the present study, 189 patients did not receive radiotherapy for many reasons. The most important reasons were the side effects and high cost of radiotherapy,which made patients’ compliance poor. The “standard mode” of postoperative breast-conserving radiotherapy is characterized by a total treatment time of 6—7 weeks.Studies have shown that radiotherapy can cause radiationinduced heart damage, such as radiation pericarditis,cardiomyopathy, valvular insufficiency, and angiosarcoma(24). Especially in the elderly, the cardiopulmonary basic conditions are poor, and can easily lead to heart and lung disease, which leads to deterioration of health. EBCTCG(25) statistically analyzed approximately 40,000 women in 400 randomized trials, indicating that a 30% increase in heart disease mortality offsets the beneficial effects of radiotherapy, most of which are caused by ischemic heart disease. Moreover, radiotherapy can affect the aesthetics of postoperative breasts (26), such as acute radiation-induced skin reactions and toxic side effects of radiotherapy related to uneven dosing. Breast pain and skin fibrosis are more severe in women who have received radiotherapy. In the ET+RT group, 21 patients developed skin reactions after radiotherapy, 5 patients showed a significant volume reduction in the affected breast after radiotherapy, and 16 patients suffered from heart damage. While, the ET group did not show these complications. However, other studies suggest that radiotherapy is feasible and well tolerated in elderly patients with early breast cancer. Fiorentino et al.(27) reported that patients have a low risk of acute and late radiotherapy-related side effects, and it also showed (28)the feasibility of simultaneous integrated boost and intensity modulated radiation therapy (SIB-IMRT) in early-stage breast cancer elderly patients. Dispinzieri et al.(29) confirmed comorbidity after hypofractionated wholebreast radiotherapy has limited influence. Further prospective studies assessing the effects of radiotherapy on elderly women with breast cancer are necessary.
Older patients have poor physical conditions and frequently have underlying diseases, such as cardiovascular and cerebrovascular diseases, hypertension, diabetes, and other diseases. The probability of death due to other diseases in elderly patients is greater than that in younger women, and the elderly women have shorter lifespans than younger women. Therefore, the risk of recurrence is lower in elderly breast cancer patients. In the present study, there were more patients who died from other diseases or accidents (98 patients, 30.0%) than those who died of breast cancer (15 patients, 4.6%). Patnaik et al. (30)suggested that comorbidities are associated with survival to the extent that early-stage patients with comorbid conditions have survival rates similar to or worse than those of late-stage patients with no comorbidities. Therefore,assessing the risk of comorbidities is particularly important for elderly breast cancer patients.
Conclusions
The results of the present study indicated that radiotherapy combined with endocrine therapy after breast-conserving surgery can reduce the LRR and improve the DFS and OS of luminal B elderly patients. Luminal A type elderly patients with early breast cancer rarely benefit from radiotherapy. The study also showed that luminal A type patients have a better DFS and OS than luminal B type patients without radiotherapy. The National Comprehensive Cancer Network (NCCN) guidelines (31)recommend that patients who are over 70 years old,T1N0M0, and hormone receptor-positive patients, and who receive endocrine therapy after breast-conserving surgery may be able to reduce radiotherapy. As the World Health Organization and Medicare define the elderly as individuals older than 65 years, this population was the target of the present study. For patients 65 years or older,with stage I-II, luminal A type, endocrine therapy without radiotherapy can be considered. In luminal B type, the patient’s condition needs to be considered, and radiotherapy should be indicated when appropriate.
Acknowledgements
This study was supported by the Chinese National Natural Sciences Foundation (No. 81672623 and No. 81502306).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
杂志排行
Chinese Journal of Cancer Research的其它文章
- Mutant p53 increases exosome-mediated transfer of miR-21-3p and miR-769-3p to promote pulmonary metastasis
- Hexokinase II promotes the Warburg effect by phosphorylating alpha subunit of pyruvate dehydrogenase
- Adjuvant hormone therapy after radical prostatectomy in highrisk localized and locally advanced prostate cancer: First multicenter, observational study in China
- Cancer IgG, a potential prognostic marker, promotes colorectal cancer progression
- Burden of colorectal cancer in China, 1990-2017: Findings from the Global Burden of Disease Study 2017
- Impact of crizotinib on long-term survival of ALK-positive advanced non-small-cell lung cancer: A Chinese multicenter cohort study