Predictive factors of histological response of colorectal liver metastases after neoadjuvant chemotherapy
2019-04-24ChloSerayssolCharlotteMaulatFlorenceBreibachFatimaZohraMokraneJanickSelvesRosineGuimbaudPhilippeOtalBertrandSucEmilieBerardFabriceMuscari
Chloé Serayssol,Charlotte Maulat,Florence Breibach,Fatima-Zohra Mokrane,Janick Selves,Rosine Guimbaud,Philippe Otal,Bertrand Suc,Emilie Berard,Fabrice Muscari
Abstract
Key words: Colorectal liver metastasis;Tumor regression grade;Neoadjuvant chemotherapy;Liver surgery;Histological response;Hepatectomy
INTRODUCTION
Colorectal cancer is the third most common cancer in men and the second most common in women worldwide[1-6].Almost a third of the patients have or will develop colorectal liver metastases (CRLMs)[2,7,8].Only 20% of these patients are amenable to curative treatment by liver resection and/or thermo-ablation[7,9,10].According to the most recent series,when combined with chemotherapy,this can result in a 5-year survival rate of up to 60%[6,11-13].
Neoadjuvant chemotherapy (NAC) has recently become nearly systematic prior to surgical management of CRLMs[7,14-16].It can be administered to patients who are initially considered to be non-resectable,and to patients with liver disease that is at the limit of resectability[14,17-19],while it is also used in cases of CRLMs that are initially resectable[20,21].The response to NAC is evaluated by radiological imaging,according to morphological criteria such as RECIST,mRECIST,and CHOI[22-28].Surgery is mostly indicated in the case of liver lesions that are responsive to NAC,or for lesions that remain stable.Indeed,progression of the disease is a poor prognostic factor,and sometimes results in a temporary postponement of liver ablation surgery[15,28,29].More recently,the response to NAC has also been evaluated based on histological criteria of the resected specimen.Rubbia-Brandt and Blazer scores indicate that histological regression correlates with the overall and disease-free survival (DFS) of patients after resection[13,30,31].The most commonly used score in the world is the one established by Rubbia-Brandt and his team[31].It reflects the tumor regression grade (TRG),which takes into account the level of necrosis and fibrosis,as well as the number of viable tumor cells.Few studies to date have documented the influence of TRG on patient survival,and these were mostly published by the authors of the scoring systems.This explains why the histological regression score of CRLM specimens is rarely used in current practice[15,32].Therefore,at present,analysis of the histological response (HR)by the TRG has no influence on whether or not adjuvant chemotherapy is administered.To our knowledge,no study has attempted to identify the predictive factors of HR after NAC.
This study aimed to analyze the HR,according to the Rubbia-Brandt TRG,on CRLM surgery performed after NAC.It also sought to identify independent predictive factors of a good response,and to analyze the influence of this response on DFS and overall.
MATERIALS AND METHODS
Patient inclusion
From January 2006 to December 2013,patients who underwent surgery for CRLMs after NAC in our department were included.They were retrospectively analyzed with regard to their pre-treatment characteristics.Patients for whom the primary tumor was resected or who had chemotherapy at another center were also included.
Patient groups
The patients were separated into two groups based on their HR,according to Rubbia-Brandt TRG.Based on their TRG,each patient was either assigned to the responder(R) group (TRG 1,2,and 3) or to the non-responder (NR) group (TRG 4 and 5).
Data collected
For each patient,the following preoperative parameters were included prospectively:Age,body mass index,American Society of Anesthesiologists’ score,history of liver surgery or a liver procedure (e.g.,portal vein embolization or drainage),date when the metastases were discovered,the existence of extra-hepatic metastases,NAC (e.g.,the number of treatment sessions and the types of chemotherapy),associated targeted therapy and type,radiological evaluation (e.g.,the morphological criteria of the response to NAC according to RECIST,mRECIST or CHOI criteria[22-28]),two-stage hepatectomy,the surgical strategy proposed by the multidisciplinary team meeting,the location of the primary,the treatment date,and the lymphatic status of the primary tumor.Perioperative parameters included:The types of procedures and number of segments resected.The postoperative parameters included:The length of hospitalization,occurrence of a severe or mild (according to the Clavien-Dindo classification) medical or surgical complication,mortality at 30 d,repeat procedures,initiation of postoperative chemotherapy,and the type of chemotherapy.The histological data comprised:The TRG,number of lesions on the resected specimens,resection margins (a resection was considered to be R0 when the smallest microscopic margin was more than or equal to 1 mm),presence of emboli,tumor differentiation grade,and size of the largest metastasis.The follow-up data comprised:The most recent update and status,date of death (if applicable),date of recurrence (if any) and its location.
Multidisciplinary team meeting
The patients’ records were assessed at a multidisciplinary team meeting that included at least one radiologist,one liver surgeon,one digestive oncologist and one pathologist.
Surgical treatment
The minimal time period between the end of NAC and the surgery was 4 to 6 wk.Surgical resections were anatomical or non-anatomical (atypical resections),and combined or not combined with perioperative radiofrequency ablation (RFA)according to the rules regarding size and localization for this method.Surgical resections were performed in one or two steps irrespective of the strategy chosen (i.e.,conventional,liver-first,or combined).Surgical resections were most often performed by laparotomy,and occasionally by laparoscopy if the anatomical and oncological conditions suited this approach.A perioperative ultrasound scan was systematically carried out to explore the liver disease,and it was used to guide the identification of the hepatectomy cuts in order to obtain an adequate margin.In the case of RFA,this was done perioperatively by two of our hospital's experienced radiologists.Ultrasound with a contrast agent (SonoVue) was sometimes used in case of difficulty viewing the anatomical area.
Histological analysis
All of the histology slides were re-evaluated in a blind manner by the same specialized pathologist.The slides had already been fixed,embedded in paraffin,cut,spread,and colored according to standard pathology methods.These slides were microscopically analyzed according to the Rubbia-Brandt TRG score.For the resected specimens that had several tumors,and in case of a dissociated response,the worst TRG was taken into account.The following criteria were also analyzed:The existence of a “dangerous halo”,thickness of the invasive front,ablation margin,degree of tumor differentiation,and presence of vascular emboli.
Ethics statement
Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Statistical analysis
The search for factors predictive of the response rate was based on percentage comparison tests (chi-squared or Fisher’s exact tests,according to the theoretical sizes)for the qualitative variables,and on comparison of means (Student’st-test,in case of normalcy and equality of the variances) or distribution tests (the Mann-Whitney nonparametric test) for the quantitative variables.The predictive factors associated with the response at a threshold of 20% in the univariate analysis were introduced in this logistic regression model.The final model including the variables that were significantly and independently associated with the response rate was obtained by stepwise regression.The intermediate nested models were compared using the likelihood ratio test.The interactions between the independent variables of the final model were identified (they were all non-significant).The adequacy of the model for the data was tested.The degree of significance was set asP< 0.05.Firstly,the analysis of TRG impact on overall survival (OS) was based on a bivariate comparison of Kaplan-Meier survival curves using the log-rank test.The survival curves were described with the use of the survival median (and the interquartile range) and hazard ratio (confidence interval at 95%) based on a Cox model.Secondly,the analysis of the independent influence of TRG on OS was based on a Cox model adjusted according to other predictive factors.The predictive factors (excluding recurrence) associated with OS at the threshold of 20% in the univariate analysis were jointly introduced with the TRG in this Cox model.The final model,including the variables that were significantly and independently associated with OS,was obtained by the stepwise regression method.The intermediate nested models were compared using the likelihood ratio test.The interactions between the TRG and the independent variables of the final model were identified (in particular,the interaction between the TRG and postoperative chemotherapy was identified and,if necessary,this was done during the stepwise regression procedure).The level of significance was set at 5% (P<0.05).The conditions for application (log-linearity and proportional risks) of the Cox model were verified.The quantitative variables were dichotomized by the median.
RESULTS
Between January 2006 and December 2013,521 liver resections for CLRM were carried out in our department.During this period,150 patients underwent a liver resection for synchronous colon or rectal cancer liver metastases after NAC.Of these 150 patients,74 (49%) were responders (R) and 76 (51%) were non-responders (NR) based on the resected specimen.
Preoperative characteristics
As shown in Table 1,75% of the patients had synchronous liver metastases.Sixtythree percent of the patients had a bilobar distribution of the lesions,with an average of 4 ± 3 lesions.The location of the primary tumor had a significant influence on the HR,which was better for the tumors of rectal origin:47.3%vs25%.The presence of a radiological response to NAC was significantly associated with a good HR.In 94% of the cases,NAC included 5-fluorouracil,in 72% it included irinotecan,and for 43% of the patients it included oxaliplatin.In the majority of cases (69%),chemotherapy was combined with a targeted therapy,without this having any statistically significant effect on the HR.However,when the type of targeted therapy was examined,it was noted that the use of bevacizumab led to a greater HR:58%vs43%.The number of NAC treatment sessions was significantly related to the HR,and the patients who were classified as R had a median number of six treatment sessions,which is fewer than for the NR patients.The patients for whom the treatment strategy comprised a liver-first procedure (i.e.,the liver resected first in case of synchronous liver metastases with the primary tumor left in place) had a significantly better HR rate.However,the patients who underwent repeat liver resections were more often histologically non-responsive.
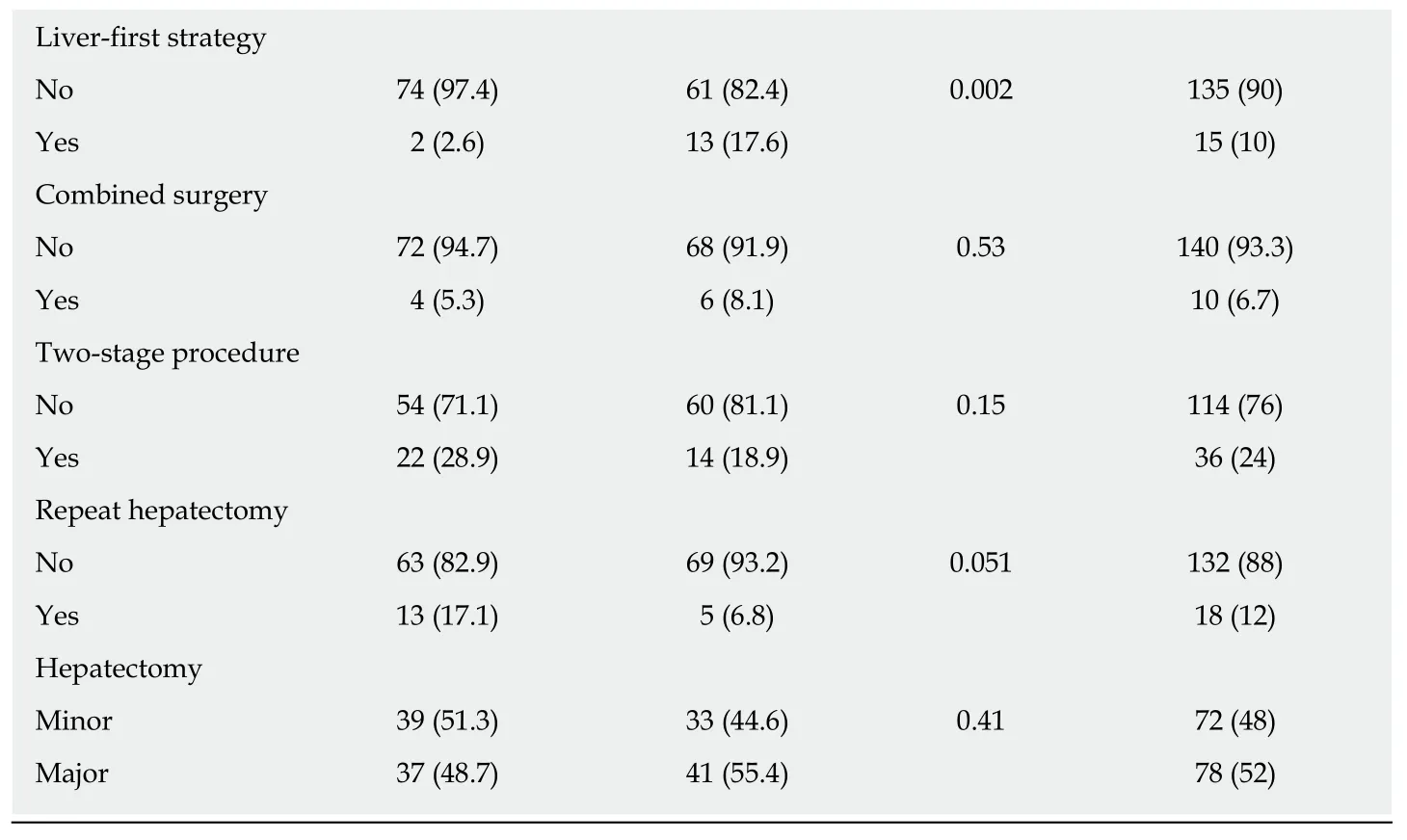
Pathological characteristics
The median number of lesions found on the resected specimens was three (1.0–4.0).The rate of resection with healthy margins (R0) was 78%.There were multiple lesions in 72% of the cases.In the group of patients classified as R,there were significantly more homogeneous HR,fewer R1 resections,and fewer vascular neoplastic microemboli (VNME) (Table 2).
实践证明,采用该方法更换蝶阀简便易行,效果良好,能够方便、迅速地在现场更换漏油的蝶阀,在缩短检修周期、降低成本方面效果显著,具有推广价值。
Postoperative characteristics
The postoperative mortality was 0.7% (one patient died of hepatocellular insufficiency),with a complication rate of 38% (Table 3).The average length of the hospital stay was 12.5 ± 7 d.Postoperative chemotherapy was administered to 55% of the patients,and in 83% of these cases,the chemotherapy protocol was similar to the one administered preoperatively.There was no significant difference between the R group and the NR group in terms of the choice of chemotherapy type.Regardless of the location,the tumor recurred in 89% of the cases.NR patients had significantly more recurrences in the liver.
Predictive factors of the histological response
The multivariate analysis identified five predictive factors of HR.Three were predictive of non-response (NR):More than seven NAC sessions,the absence of a radiological response after NAC,and a repeat hepatectomy.Two were predictive of a good response (R):Rectal origin of the primary tumor and liver-first strategy (Table 4).
Survival and prognostic factors
The median survival of the patients was 6 yr (ranging from 4–7.5 yr).
Overall survival:The OS rates at 3 yr and 5 yr were 57% and 36%,respectively.These OS rates were significantly better for patients with an HR (the R group):65% and 45%,respectively,vs47% and 26%,respectively,for the NR group (Figure 1).The identification of independent prognostic factors of OS (Table 5) revealed that the effect of HR was dependent on the presence or absence of VNME.In patients without VNME,HR was an independent prognostic factor of OS,while this was no longer the case in the presence of VNME upon analysis of the ablated specimen.Other factors that were prognostic of poor OS were:Male gender,preoperative targeted therapy,a two-stage hepatectomy protocol,and a N+ status of the primary tumor.
DFS:The DFS rates at 3 yr and 5 yr were 14% and 11%,respectively.These DFS survival rates were significantly better for patients with HR (the R group):19% and 11%,respectively,vs9% and 5%,respectively,for the NR patients (Figure 2).The search for independent prognostic factors of DFS identified one good prognostic factor,which was the presence of HR with NAC (the R group,P=0.013),and four poor prognostic factors:NAC with targeted therapy (P=0.004),more than three preoperative metastases (P=0.001),R1 resection (P=0.022),and a size greater than 3 cm for the largest metastasis (P=0.011).
DISCUSSION
Our work demonstrates that the HR of CRLMs operated on after NAC has a significant influence on OS and DFS,as evaluated by the Rubbia-Brandt score.In this population,the OS rate at 5 yr was equivalent to that stated in the literature,which varies from 18%-58%[8,10-13,33-40].However,the DFS in this population was at the lowerlimit of that reported in the literature,which varies from 11%-37%[10,35-39].This can likely be explained by the particularly severe liver disease in our population of selected patients.Indeed,75% of our patients had synchronous metastases,while in the literature this rate varies from 15%-50%[2,7,8,38].We noted HR in 49% of the patients(TRG 1 to 3),including five patients (7%) with complete tumor regression (TRG1).In research published in 2007,the Rubbia-Brandt team found a good HR rate of 27%-82%,which varied according to the chemotherapy protocol[31].Viganòet al[13]had figures similar to ours,with a good HR (TRG 1 to 3) for 44% of the patients and complete tumor regression (TRG1) for 8% of the patients,as was the case with the series reported by Loupakiset al[41],with HR for 48% and complete tumor regression(TRG 1) for 14% of the patients.We used the Rubbia-Brandt score,as it was the first to define standardized histological criteria of response to NAC in cases of CRLMs,and also because of its use in the management of rectal cancers[42].
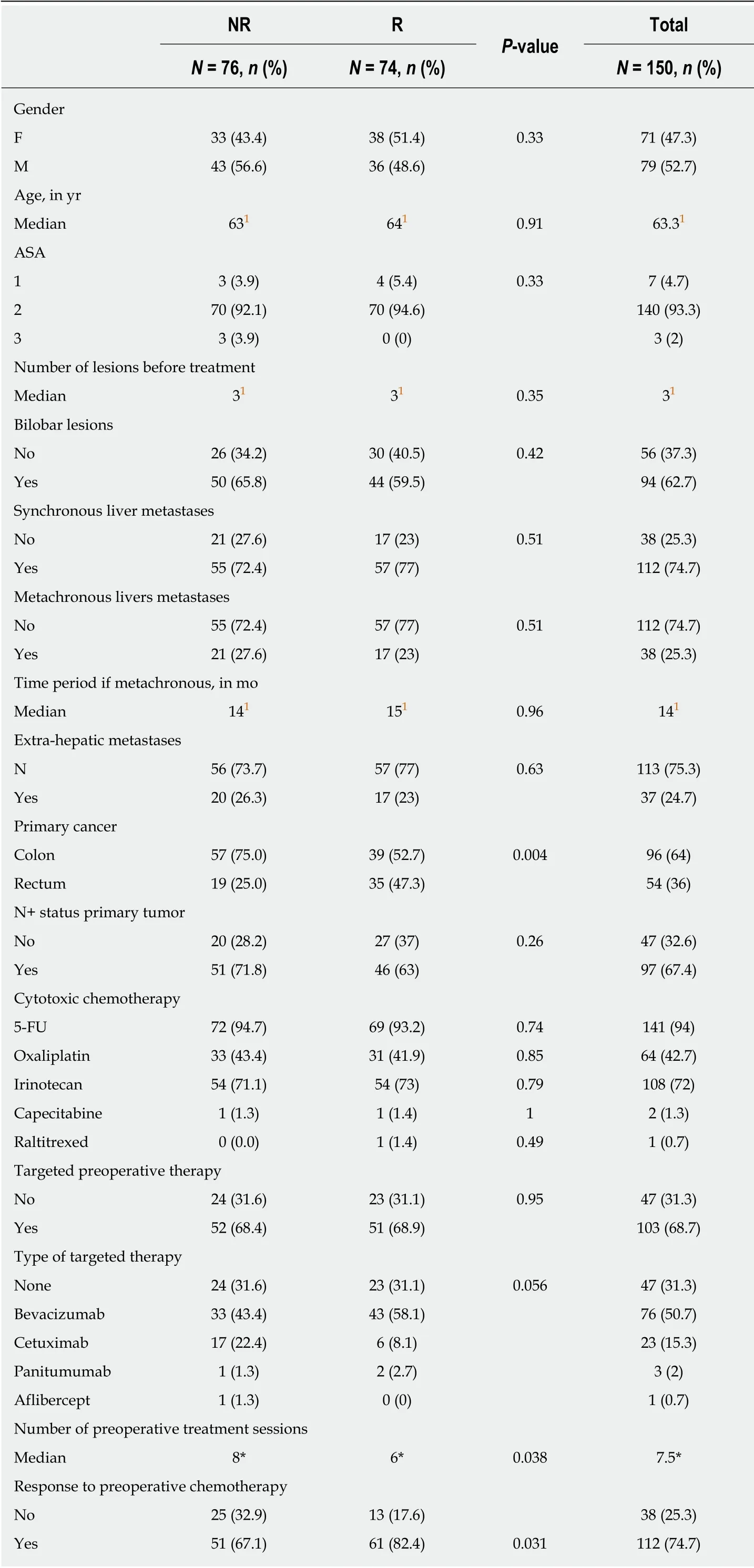
Table 1 Preoperative criteria
1Median.NR:Non-responders;R:Responders;F:Female;M:Male;ASA:American Society of Anesthesiologist’s score;5-FU:5-Fluorouracil.
We identified five independent predictive factors of HR after NAC.Three factors were predictive of the absence of HR (more than seven NAC treatment sessions,the absence of a radiological response after NAC,and repeat hepatectomy).The high number of NAC treatment sessions is probably a reflection of tumor chemotherapy resistance.This factor likely indicates that the earlier the response (evaluated radiologically) (i.e.,before the first seven treatment sessions),the greater the chances of a good associated HR.In the study by Viganòet al[13],the number of treatment sessions also appeared to be a predictive factor of HR based on multivariate analysis,with a better HR when there were fewer than six chemotherapy treatment sessions.The absence of a radiological response (i.e.,stability or progression) after NAC is recognized as a major factor for cancelling or delaying surgery after NAC[20,43-45].The influence of a repeat hepatectomy on HR has not been reported in the literature to date.One of the explanations,aside from the actual severity of a liver recurrence after the first hepatectomy,could be a change in the chemotherapy sensitivity of the recurring tumor.In our series,rectal origin of the primary tumor was associated with a three-fold greater probability of having a good HR.We found two studies in the literature for which this location of the primary tumor was a poor prognostic factor of OS[46,47].It has also been reported that a primary tumor that originated in the ascending colon is a poor prognostic factor[48-53].A liver-first strategy in case of synchronous CRLMs was a factor predictive of a good HR.This can probably be explained by the fact that only the patients who were radiological responders after NAC have access to this strategy.To our knowledge,only two studies in the literature,namely Viganòet al[13]and Pietrantonioet al[54],have examined the factors predictive of a HR of CRLMs,based on multivariate analysis involving 323 and 93 patients,respectively.Viganòet al[13]were able to identify four predictive factors of a good response,which were the combination of oxaliplatin and irinotecan,the radiological response,the largest lesion ≤ 5 cm,and a carcinoembryonic antigen level≤ 5 ng/mL.
OS was influenced by the HR according to whether or not there were VNME on the resected specimen.In fact,in the absence of VNME,the HR is an independent factor of a good prognosis for OS.Although the impact of the HR on OS has already beenreported in the literature[13,41,54],this is the first time that it has been shown that its influence is abrogated by the presence of VNME on the resected specimen,which is a known factor of poor prognosis.Therefore,tumor aggressiveness as reflected by VNME appears to be a more significant determining factor than the HR for the OS prognosis of patients.Four other independent factors of poor prognosis for OS were identified:Male gender,use of targeted therapy,two-stage hepatectomy,and N+status of the primary tumor.Male gender[40,46,47,55-58]and a positive lymphatic status of the primary tumor[34,58-61]are prognostic factors that have been reported in the literature.The administration of NAC with a targeted therapy,which was identified in our analysis,can be explained by the fact that bevacizumab was typically used(74% of the targeted therapies).This is the treatment of choice for mutant RAS tumors,which carry worse prognoses[59,61-67].In terms of the two-stage hepatectomies,this can be explained by the fact that 13% of our patients did not undergo the second stage of surgery due to progression of the tumor after the first procedure.These figures are comparable to those presented in the literature,which vary from 15%-31%[68-73].
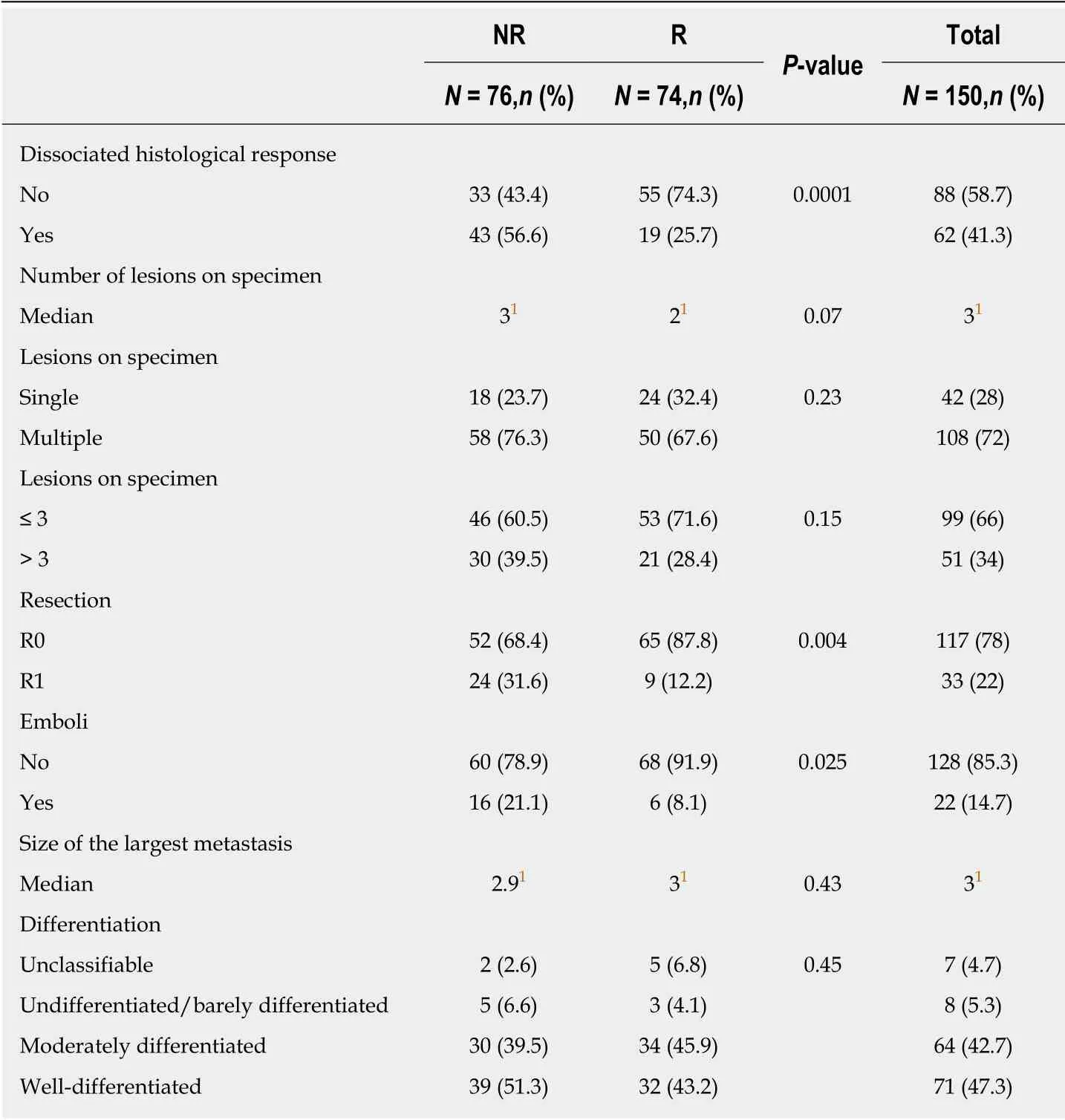
Table 2 Pathological criteria
DFS was significantly influenced by the HR,with 17% survival at 5 yr for the responders compared to 5% for the non-responders.A similar difference in DFS was found in the study by Rubbia-Brandtet al[31],with a three-fold better survival for the responders compared to the non-responders.Four independent factors of poor prognosis were identified:Use of neoadjuvant targeted therapy,more than three preoperative lesions,metastasis with a size greater than 3 cm,and R1 resection.The number and size of metastases[13,35,36,38,58,74],and R1 resection[35,36,38,75-77]are the typical factors of poor prognosis found in the literature.
In conclusion,this study confirmed that the HR of CRLMs after NAC has an influence on survival and,hence,warrants attention.We found,however,that this influence on OS was lacking in cases of particularly aggressive disease,with microscopic vascular invasion in the histological analysis.Two simple criteria enable the prediction of HR after NAC:More than seven treatment sessions and the absence of a radiological response.
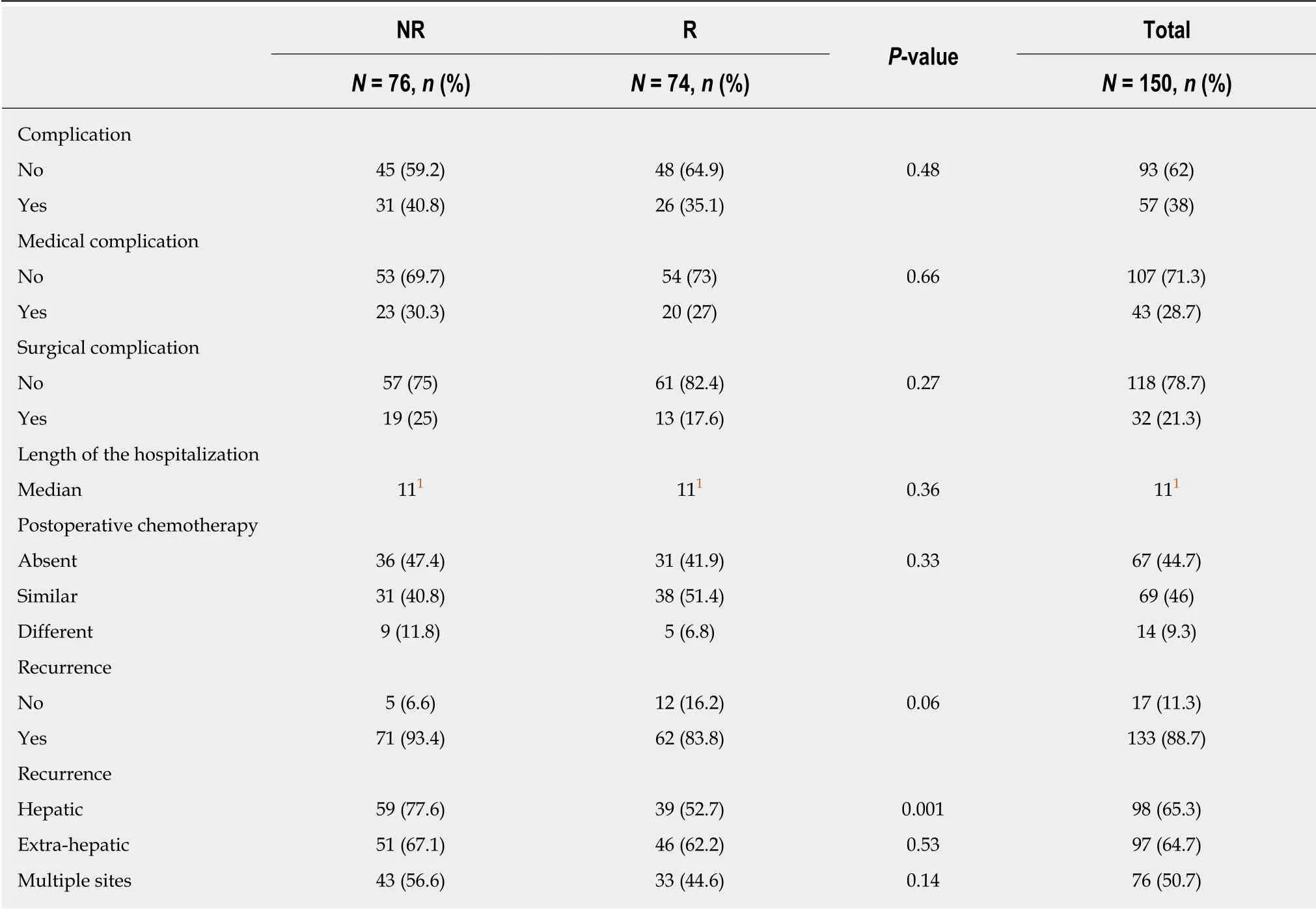
Table 3 Postoperative criteria
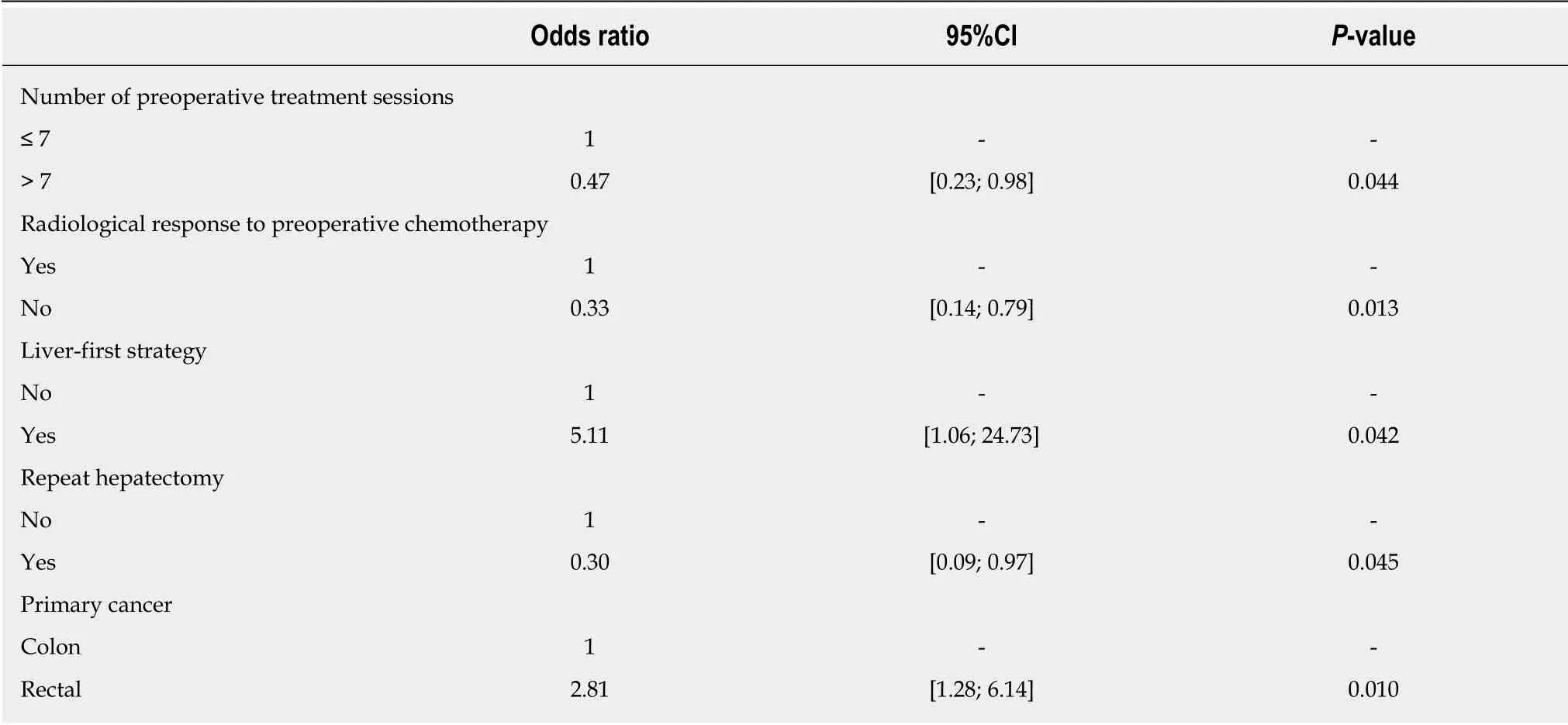
Table 4 Predictive factors of the histological response
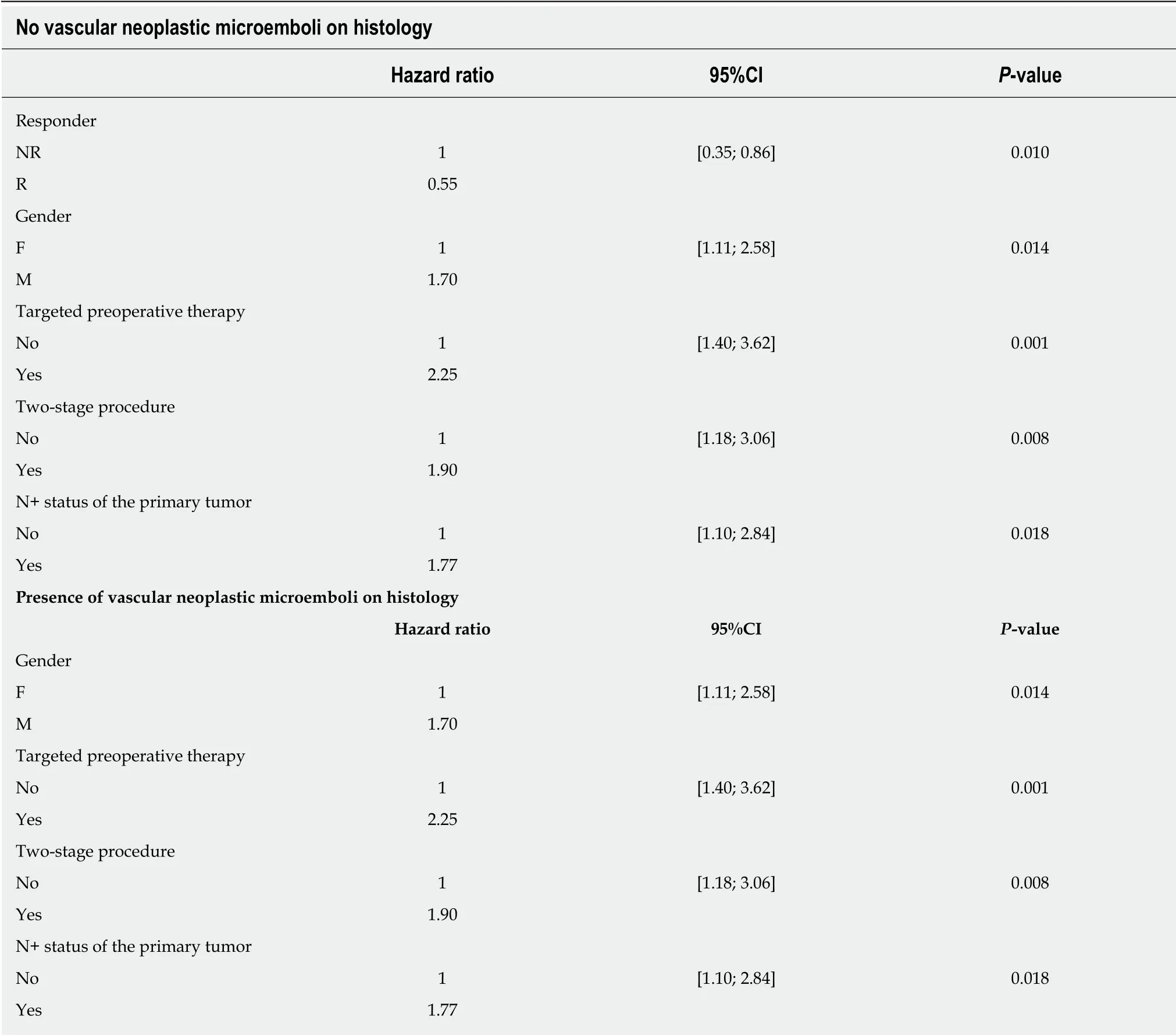
Table 5 Prognostic factors of overall survival
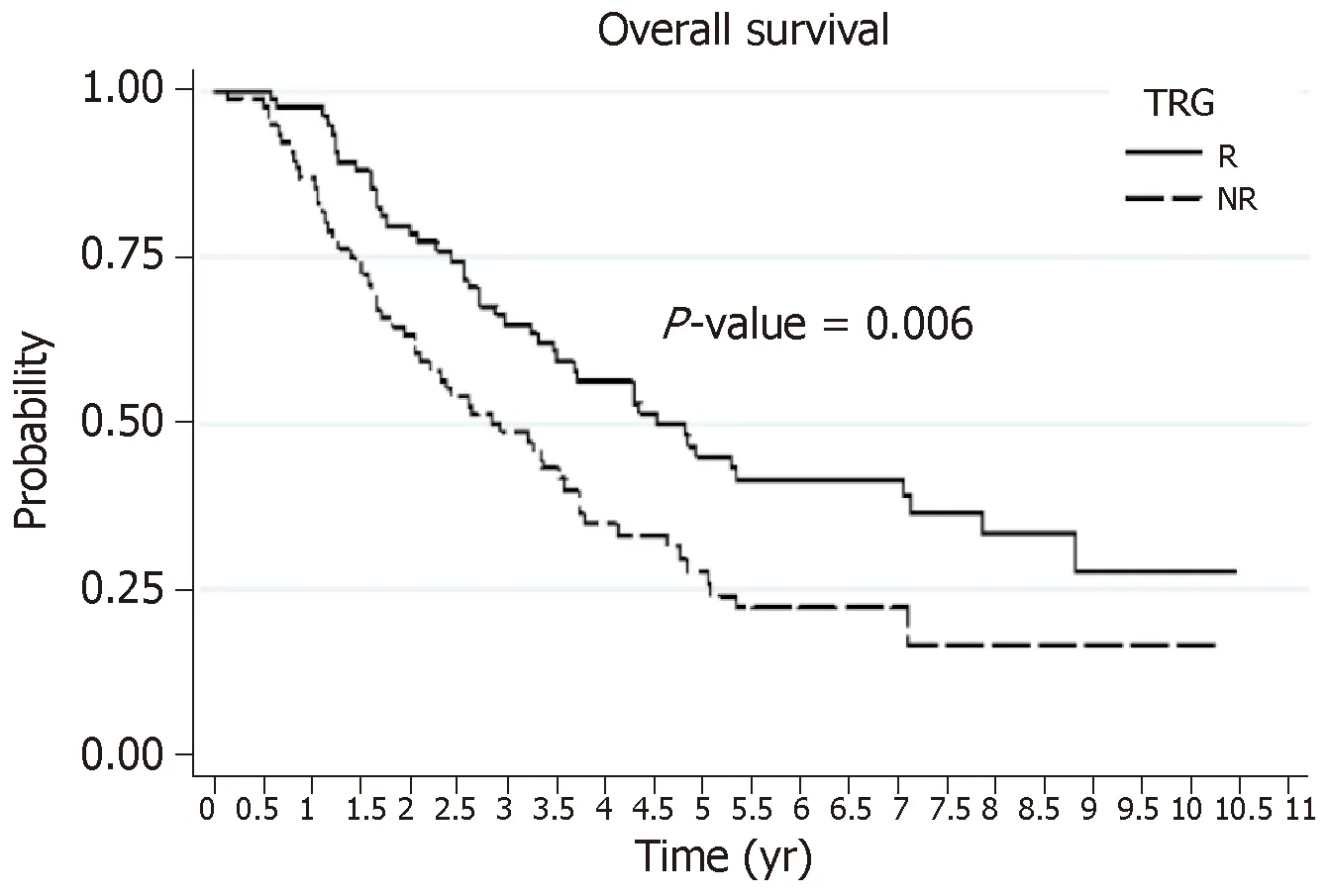
Figure 1 Influence of the histological response on overall survival.
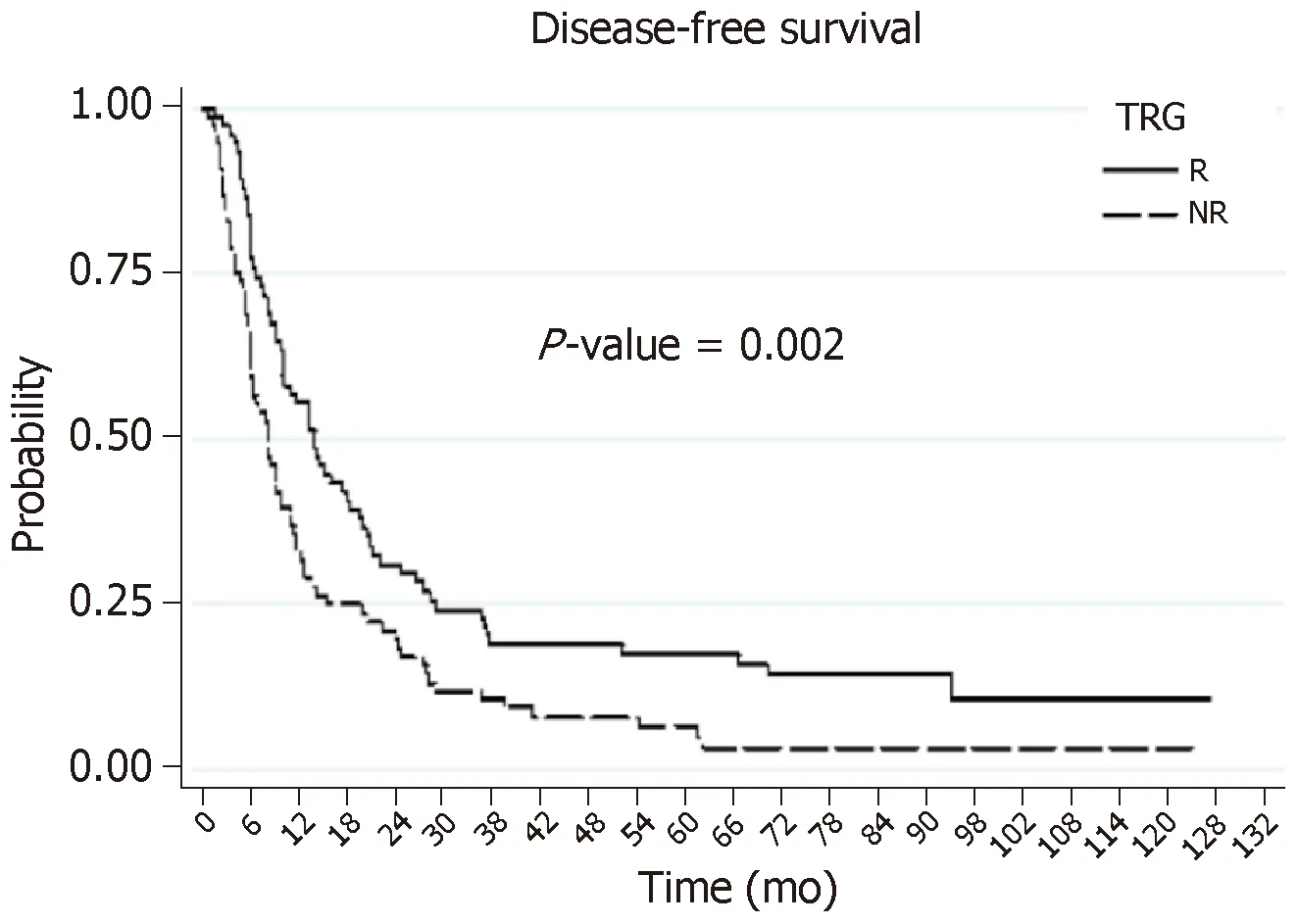
Figure 2 Influence of the histological response on disease-free survival.
ARTICLE HIGHLIGHTS
Research background
Colorectal cancer is the third most common cancer in men and the second most common in women worldwide.Almost a third of the patients has or will develop liver metastases.Neoadjuvant chemotherapy (NAC) has recently become nearly systematic prior to surgery of colorectal livers metastases (CRLMs).The response to NAC is evaluated by radiological imaging according to morphological criteria.More recently,the response to NAC has been evaluated based on histological criteria of the resected specimen.The most often used score is the tumor regression grade (TRG),which considers the necrosis,fibrosis,and number of viable tumor cells.
Research motivation
Few studies to date have documented the influence of TRG on patient survival,and they were mostly published by the authors of the scoring systems.This explains why the histological regression score of CRLM specimens is rarely used in current practice[15,32].Therefore,at present,analysis of the histological response by the TRG has no influence on whether or not adjuvant chemotherapy is administered.To our knowledge,no study has attempted to identify the predictive factors of histological response after NAC.
Research objectives
Our research aimed to analyze the histological response,according to the Rubbia-Brandt TRG,on CRLM surgery performed after NAC.It also sought to identify independent predictive factors of a good response,and to analyze the influence of this response on overall and disease-free survival.
Research methods
From January 2006 to December 2013,150 patients who had undergone surgery for CRLMs after NAC were included.The patients were separated into two groups based on their histological response,according to Rubbia-Brandt TRG.Based on their TRG,each patient was either assigned to the responder (R) group (TRG 1,2,and 3) or to the non-responder (NR) group (TRG 4 and 5).All of the histology slides were re-evaluated in a blind manner by the same specialized pathologist.Univariate and multivariate analyses were performed.
Research results
Seventy-four patients were classified as responders and 76 as non-responders.The postoperative mortality rate was 0.7%,with a complication rate of 38%.Multivariate analysis identified five predictive factors of histological response.Three were predictive of non-response (NR):More than seven NAC sessions,absence of a radiological response after NAC,and repeat hepatectomy(P < 0.005).Two were predictive of a good response (R):Rectal origin of the primary tumor and a liver-first strategy (P < 0.005).The overall survival was 57% at 3 yr and 36% at 5 yr.The diseasefree survival rates were 14% at 3 yr and 11% at 5 yr.Factors contributing to a poor prognosis for the DFS were:No histological response after NAC,largest metastasis > 3 cm,more than three preoperative metastases,R1 resection,and the use of a targeted therapy with NAC (P < 0.005).
Research conclusions
The histological response of CRLMs after NAC has an influence on survival,hence warranting consideration.We found,however,that this influence on overall survival was lacking in cases of particularly aggressive disease,with microscopic vascular invasion upon histological analysis.
Research perspectives
Two simple criteria enable the prediction of a histological response after NAC:More than seven treatment sessions and absence of a radiological response.
猜你喜欢
杂志排行
World Journal of Gastrointestinal Oncology的其它文章
- Significance of HER2 protein expression and HER2 gene amplification in colorectal adenocarcinomas
- Validated model for prediction of recurrent hepatocellular carcinoma after liver transplantation in Asian population
- Iodine-125 implantation with transjugular intrahepatic portosystemic shunt for main portal vein tumor thrombus
- Up-regulation of tumor necrosis factor-α pathway survival genes and of the receptor TNFR2 in gastric cancer
- Identification of genomic features associated with immunotherapy response in gastrointestinal cancers