Extreme hyperbilirubinemia:An indicator of morbidity and mortality in sickle cell disease
2019-04-23JohnPaulHaydekCesarTabordaRushikeshShahPreetiReshamwalaMorganMcLemoreFuadElRassiSaurabhChawla
John Paul Haydek,Cesar Taborda,Rushikesh Shah,Preeti A Reshamwala,Morgan L McLemore,Fuad El Rassi,Saurabh Chawla
John Paul Haydek,Department of Medicine,Emory University School of Medicine,Atlanta,GA 30322,United States
Cesar Taborda,Rushikesh Shah,Preeti A Reshamwala,Saurabh Chawla,Division of Digestive Diseases,Department of Medicine,Emory University School of Medicine,Atlanta,GA 30329,United States
Morgan L McLemore,Fuad El Rassi,Department of Hematology and Medical Oncology,Emory University School of Medicine,Atlanta,GA 30329,United States
Abstract
Key words:Sickle cell disease;Sickle cell hepatopathy;Liver diseases;Extreme hyperbilirubinemia;Mortality
INTRODUCTION
Sickle cell hepatopathy (SCH) encompasses a wide range of hepatic pathologies arising from variety of pathophysiologic insults[1,2]in patients with sickle cell disease(SCD).The hepatobiliary manifestations are most commonly seen in patients with hemoglobin SS (Hb SS) anemia as compared to patients with sickle cell trait,hemoglobin SC disease and hemoglobin S-beta thalassemia.Multiple pathways contribute to the development of SCH and result in a myriad of different conditions including hepatic sequestration[3,4],cholestasis and biliary obstruction[2,5],and complications related to the transfusions that patients with SCD frequently receive[6].
The impact of SCH on morbidity and mortality in SCD patients is often underrecognized.With evolving treatment strategies in SCD,improvements have been made in morbidity and mortality,resulting in higher longevity in SCD patients[7].As a result,some of the previously rare clinical scenarios,such as hepatobiliary complications of SCD,are more commonly encountered.Sickle cell related liver disease is associated with higher rates of morbidity.Previous studies have shown that factors such as hyperbilirubinemia,elevated ferritin,and alkaline phosphatemia are factors independently associated with mortality[8].However,several of these studied have been limited by small sample size.Mortality typically results due to complications related to sepsis or vascular complications.Some studies have estimated that acute liver failure was the primary cause of death for between 8%-10.7% of patients with SCD[9,10].Despite this,liver failure and end stage liver disease are seldom identified as the immediate cause of death[11-13].
Abnormal liver markers are frequently found in patients with SCD,but these are often limited to mild elevations in total bilirubin without rise in alanine aminotransferase (ALT) or aspartate aminotransferase (AST)[14].As compared to isolated rise in serum bilirubin,SCH has a variety of possible presentations and the absence of stable definitions of the individual conditions within the spectrum of SCH possesses a unique challenge in clinical management as well as research on SCH[1].
Our study aims to describe the prevalence of extreme hyperbilirubinemia (EH),one of the key indicators of severe SCH and its effect on morbidity,mortality and healthcare expenditures related to SCH.We also want to better understand the risk factors related to it in a large cohort of patients with SCD seen at the Grady Memorial Hospital Sickle Cell Clinic.Third,we aim to identify whether there is any correlation between SCD genotype and severe SCH identified through EH.
MATERIALS AND METHODS
Identification of cases and controls
This retrospective cohort study was performed using a database of patients with SCD treated at Grady Memorial Hospital between May 2004 and January 2017.With institutional review board approval,the database was queried for patients with EH(defined as total bilirubin above 13.0 mg/dL).A control group was identified from the same database with patients with total serum bilirubin ≤ 5.0 mg/dL.Patient inclusion criteria included adults older than 18 years old,hemoglobin electrophoresis confirmation of SCD,and absence of biliary obstruction identified on abdominal ultrasound.Exclusion criteria also included patients with known infection with hepatitis A,B or C;diagnosis of autoimmune hepatitis;alcoholism;cirrhosis of different etiologies;follow-up less than one year and patients for whom a complete set of required data was unavailable.
Data analysis
Associations between laboratory results,hydroxyurea dosing,quick Sequential Organ Failure Assessment (qSOFA) score[15]and rate of blood transfusions were assessed with two-sampleT-tests.Chi-square testing was performed to compare the frequency of sickle cell genotypes.Fisher's exact test was used to compare rates of death within 1 year.Level of significance for all tests was set at 0.05.Patients were identified as having EH if total bilirubin was chronically elevated over the course of a hospitalization or for at least 6 wk as an outpatient to levels > 13.0 mg/dL with direct bilirubin > 50% of total bilirubin.This level of hyperbilirubinemia was selected because of previous usage in the literature and findings that published cases in the literature all had levels greater than 13.0 mg/dL[16].
RESULTS
Patient populations
A total of 1172 patients with SCD were identified,out of which fifty-seven charts were found of patients with bilirubin greater than 13 mg/dL.4.8%(57/1172) of patients were identified to have severe SCH as defined by EH.The control group consisted of 99 patients.There were no demographic differences between patients with and without EH (see Table1).After data collection,15 patients were removed from the case-arm due to inadequate patient records,leaving 42 patients.
Lab Abnormalities
Patients with severe EH had increased levels of ALT (157.0 ± 266.2 IU/Lvs19.8 ± 21.3 IU/L,P< 0.001),AST (256.5 ± 485.9 U/Lvs28.2 ± 14.7 U/L,P< 0.001) total bilirubin(18.41 ± 6.74 mg/dLvs1.29 ± 0.19 mg/dL,P< 0.001) direct bilirubin (11.73 ± 6.03 mg/dLvs0.28 ± 0.07,P< 0.001) and alkaline phosphatase (AP;218.0 ± 176.2 IU/Lvs85.9 ± 68.4 IU/L,P< 0.001) compared to controls (see Table2).Given limited data,comparisons were not performed for prothrombin time or lactate dehydrogenase(LDH).There was insufficient data for comparison of prothrombin time or LDH.
Outcomes
Patients with EH had worse outcomes compared to the control group.They experienced higher rates of end organ failure measured with qSOFA scores (0.42 ±0.68vs0.01 ± 0.12,P< 0.001),increased need for blood products (63%vs5%,P<0.001),and exchange transfusions (10.5%vs1.3%,P= 0.022).There were 2 deaths in the EH arm and 0 deaths in the control arm,so Fisher's exact test was used.While the results trended towards significance,they were not significantly different (4.7%vs0%,P= 0.09).Two deaths occurred within the severe SCH group,and were due to acute chest syndrome and septic shock.
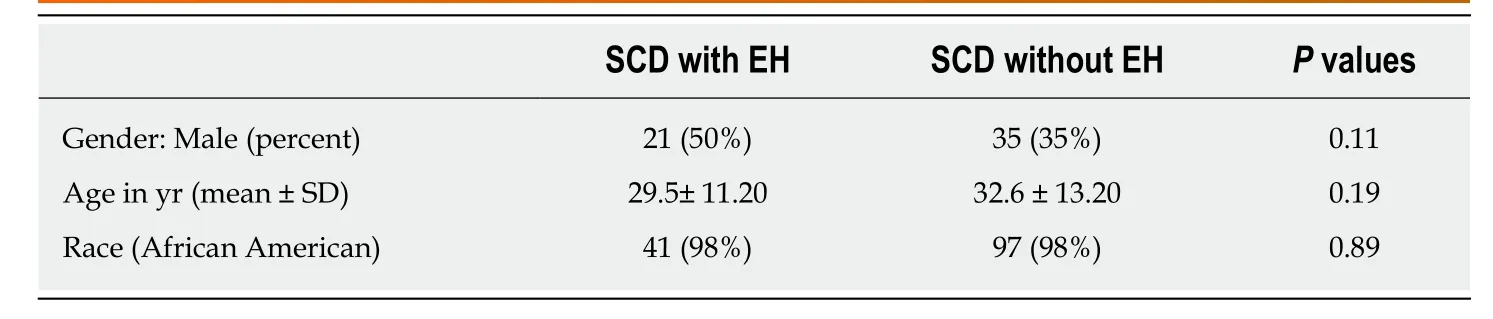
Table1 Demographics differences in sickle cell disease patients with and without severe extreme hyperbilirubinemia
Hydroxyurea usage
Usage and dosage of hydroxyurea was analyzed between the two groups.Prescribing rates (34%vs25%,P= 0.27) and average daily doses (278 ± 469 mgvs288 ± 602 mg,P= 0.95) were not different between the two groups.
Sickle cell genotypes
There were significant differences among the genotype breakdown between those that experienced EH and the control groups.There were five types of genotypes identified:Hb SS,hemoglobin S beta thalassemia,hemoglobin S beta null thalassemia,hemoglobin SC and hemoglobin S beta thalassemia status undetermined (see Table3).The EH group almost entirely consisted of Hb SS SCD,while the control group had a predominance of hemoglobin SC and sickle beta thalassemia.Fisher's exact test was done on the genotypes and showed significant differences between the two groups (P< 0.0001).
Correlations
There were weak correlations between total bilirubin levels and other liver enzymes.When plotted in relation to total bilirubin,Pearson coefficients werer= 0.28 for AP,r= 0.24 for ALT,r= 0.29 for AST,andr= 0.23 for LDH.
DISCUSSION
In this case-control study of sickle cell liver disease,we observed that patients with SCD who developed SCH as defined by EH had higher rates of other liver enzyme elevations as well as higher rates of morbidity,defined by end organ damage and need for blood transfusion.SCH is an under-diagnosed disease state,and one that will become more prominent in practice as patients with SCD live longer.It can often be difficult to diagnose because of the chronic hemolytic state that SCD patients are in,causing chronically elevated bilirubin levels and occasionally,mild elevations in transaminases.Previous studies[16]have used a total bilirubin level of 13 mg/dL as a specific cutoff for a condition termed “EH” and used as a metric for SCH.We chose to use this same level as a definition of EH to maximize specificity,at the expense of potentially excluding milder cases of SCH.
These findings are consistent with our hypothesis that severe SCH,like other secondary complications of SCD,is associated with higher rates of morbidity.Mortality was higher in the EH group but was not statistically significant between the two samples given the absence of death among the control group and low number of deaths among the EH group.Surprisingly,there were no differences between the groups in regard to hydroxyurea usage or duration.While there are very limited studies evaluating hyperbilirubinemia or SCH as a predictor of mortality,our findings are consistent with other small analyses that showed associations between direct hyperbilirubinemia and increased mortality[8,16].Our mortality rates are lower than that seen in Feldet al[8]although our length of follow-up was much shorter than used in their study.Additionally,Feldet al[8]did not perform subgroup analysis on patients with very high levels of hyperbilirubinemia.
The differences in genotype identified between the two groups were a finding that was not expected originally.AlthoughHb SSdisease is associated with more crises,Hb SCdisease is associated with higher rates of thromboembolic disease.The results may suggest that patients withHb SSSCD are at increased risk for SCH.However,it may also indicate that patients with lesser variants of SCD,includingHb SCor sickle thalassemia,experience more mild variants of SCH and would not be identified using a relatively specific EH cutoff.Further study is needed to identify whether hepatic markers other than EH are reliable identifiers of SCH.Additionally,creation of a large database that also includes laboratory data prior to the onset of SCH may help in identifying predictive factors that aid in diagnosis.
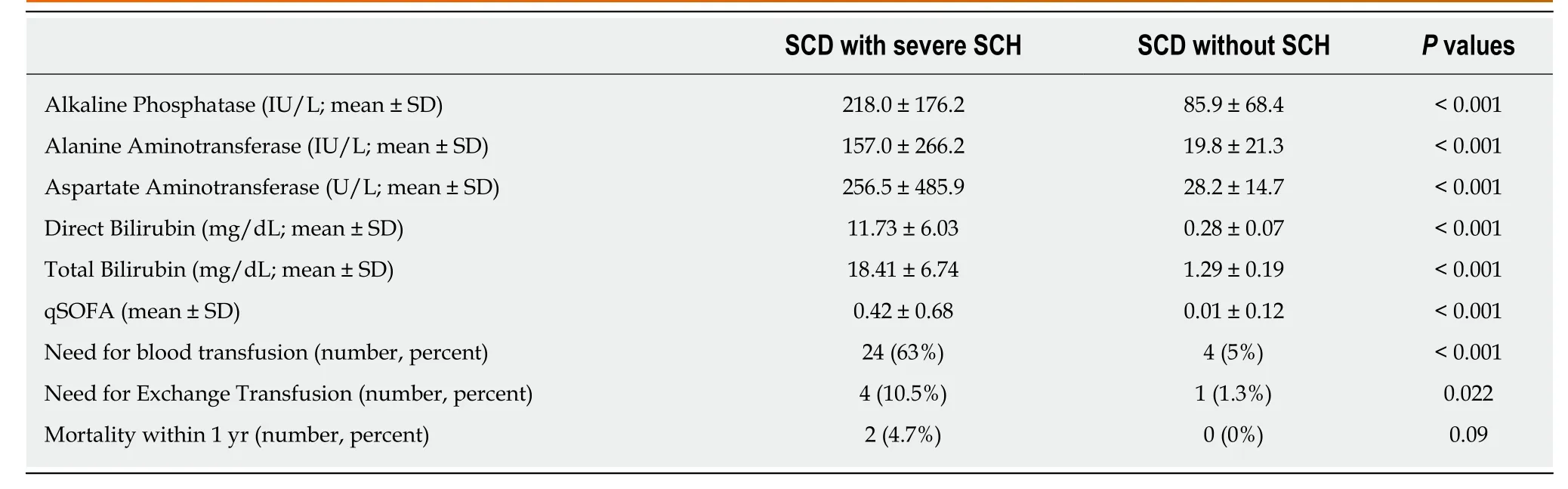
Table2 Lab values and outcomes in sickle cell disease patients with and without severe sickle cell hepatopathy
Among patients with SCD,hydroxyurea is the only approved disease modifying therapy[17].A large randomized controlled study that prompted the drug's approval,the Multicenter Study of Hydroxyurea for Sickle Cell Anemia[18],showed a significant reduction in rates of crises,rates of acute chest syndrome and need for blood transfusion.However,there was not a difference of rates of hepatic sequestration or hepatic failure between the groups,and it is unknown whether hydroxyurea use is protective against SCH.One case report showed improvement in chronic hepatic sequestration with long-term hydroxyurea use[19],but there is little else published regarding hydroxyurea use and liver function.In our study,we did not see a difference in hydroxyurea use between the two groups but we could not reliably track the compliance of hydroxyurea use in our patients.
Our study has several limitations including small sample size,lack of analysis by genotype,and lack of exclusion of outpatient visits.The use of both inpatient and outpatient encounters did not allow us to accurately compare length of stay between the groups,which was hypothesized to be longer among the EH group.These limitations are balanced by the strengths of this study,including the novelty of data about SCH and the large database queried for this study.
枸杞子药材样品中各有机酸类成分含量之间相关性分析显示,多种有机酸达到极显著正相关。中药的功效是多种成分共同作用的结果,与其不同成分的含量和比例相关,因此根据本研究结果中枸杞子药材中各有机酸类成分含量的相关性有助于进一步分析该类成分与复杂药效的关系。
In summary,our manuscript has identified SCH as a secondary complication of SCD that is associated with increased morbidity and higher healthcare utilization.Further study is needed to identify the longitudinal course of the disease,including whether there are predictive factors that precede the clinical presentation of SCH,whether sickle cell genotype is predictive of the likelihood of SCH,and whether there are protective factors that reduce the likelihood of developing SCH.
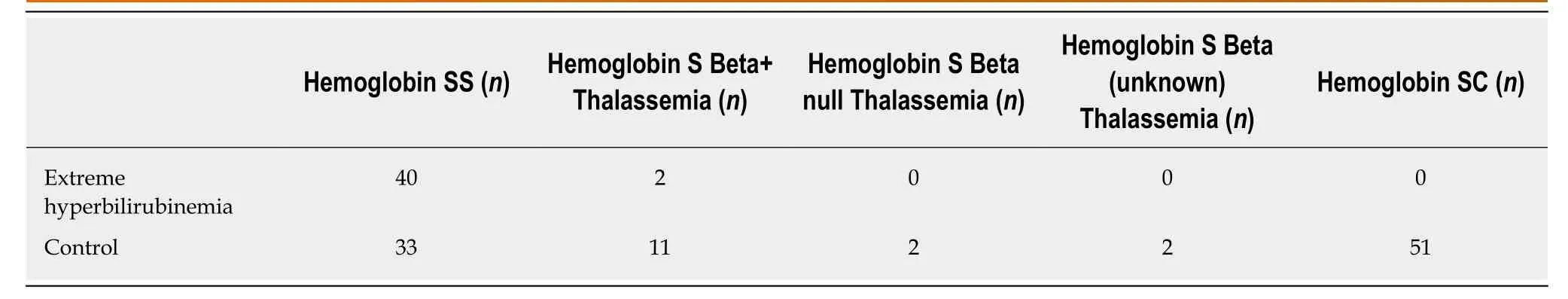
Table3 Hemoglobin genotype breakdown between the extreme hyperbilirubinemia and control groups
ARTICLE HIGHLIGHTS
Research background
Sickle cell hepatopathy is a category of pathologies that occur among patients with sickle cell disease,and has been rising in incidence as lifespan has increased.Additionally,based on autopsy studies,sickle cell hepatopathy is felt to be underreported and likely contributes to mortality in more cases than in realized.Previous studies have tried to identify risk factors associated with sickle cell hepatopathy but have been limited by small size.
Research motivation
With the increasing incidence of sickle cell hepatopathy,understanding risk factors and improving its recognition are important to its early diagnosis and treatment.
Research objectives
The main objectives of this study were to describe the prevalence of extreme hyperbilirubinemia,its effect on morbidity and mortality,and any association between sickle cell genotype and sickle cell hepatopathy.
Research methods
We used a retrospective observational cohort study to evaluate the epidemiology and outcomes behind extreme hyperbilirubinemia,a form of sickle cell hepatopathy.This was conducted at a hospital with a large population of patients with sickle cell disease.
Research results
About 5% of patients in our sickle cell disease database developed extreme hyperbilirubinemia.This cohort was associated with higher rates of systemic illness,measured by quick Sequential Organ Failure Assessment scores,higher rates of blood transfusions and higher rates of exchange transfusions.There was not a higher mortality rate in the extreme hyperbilirubinemia group.There were higher rates of patients with hemoglobin SS sickle cell disease among the extreme hyperbilirubinemia group compared to a control group,compared to other genotypes.Additionally,there were not significant differences in hydroxyurea use between groups.
Research conclusion
Our study highlights the increased morbidity and use of blood products seen among patients with extreme hyperbilirubinemia,a form of sickle cell hepatopathy.It also identifies different rates of sickle cell hepatopathy depending on the sickle cell genotype present.Finally,it shows that reported hydroxyurea doses did not have an effect on development of sickle cell hepatopathy.
Research perspective
Our study highlights the need for further study into types of sickle cell hepatopathy,whether strategies other than hydroxyurea can mitigate the risk of development of sickle cell hepatopathy,and whether there are any identifiable risk factors to increase rates of early diagnosis.
ACKNOWLEDGEMENTS
Special thanks are extended to Eugene Huang and Ziduo Zheng from the Emory Data Analytics and Biostatistics Core for assistance with statistical work.
猜你喜欢
杂志排行
World Journal of Hepatology的其它文章
- Update on management of gastric varices
- Hepatocellular carcinoma recurrence after liver transplantation:Risk factors,screening and clinical presentation
- Protective action of glutamine in rats with severe acute liver failure
- Angiogenesis of hepatocellular carcinoma: An immunohistochemistry study
- Preoperative immunonutrition in patients undergoing liver resection:A prospective randomized trial
- Intraperitoneal rupture of the hydatid cyst:Four case reports and literature review
