Personalized medicine in functional gastrointestinal disorders:Understanding pathogenesis to increase diagnostic and treatment efficacy
2019-03-22XiaoJingWangMichaelCamilleri
Xiao Jing Wang, Michael Camilleri
Abstract There is overwhelming evidence that functional gastrointestinal disorders(FGIDs) are associated with specific mechanisms that constitute important targets for personalized treatment. There are specific mechanisms in patients presenting with functional upper gastrointestinal symptoms (UGI Sx). Among patients with UGI Sx, approximately equal proportions (25%) of patients have delayed gastric emptying (GE), reduced gastric accommodation (GA), both impaired GE and GA,or neither, presumably due to increased gastric or duodenal sensitivity.Treatments targeted to the underlying pathophysiology utilize prokinetics,gastric relaxants, or central neuromodulators. Similarly, specific mechanisms in patients presenting with functional lower gastrointestinal symptoms, especially with diarrhea or constipation, are recognized, including at least 30% of patients with functional constipation pelvic floor dyssynergia and 5% has colonic inertia(with neural or interstitial cells of Cajal loss in myenteric plexus); 25% of patients with diarrhea-predominant irritable bowel syndrome (IBSD) has evidence of bile acid diarrhea; and, depending on ethnicity, a varying proportion of patients has disaccharidase deficiency, and less often sucrose-isomaltase deficiency. Among patients with predominant pain or bloating, the role of fermentable oligosaccharides, disaccharides, monosaccharides and polyols should be considered. Personalization is applied through pharmacogenomics related to drug pharmacokinetics, specifically the role of CYP2D6, 2C19 and 3A4 in the use of drugs for treatment of patients with FGIDs. Single mutations or multiple genetic variants are relatively rare, with limited impact to date on the understanding or treatment of FGIDs. The role of mucosal gene expression in FGIDs, particularly in IBS-D, is the subject of ongoing research. In summary, the time for personalization of FGIDs, based on deep phenotyping, is here;pharmacogenomics is relevant in the use of central neuromodulators. There is still unclear impact of the role of genetics in the management of FGIDs.
Key words: Gastrointestinal symptoms; Gastric emptying; Gastric accommodation;Diarrhea; Constipation; Irritable bowel syndrome; Bile acid diarrhea; Phenotypes;Pharmacogenomics; Prokinetics; Neuromodulators
INTRODUCTION
Functional gastrointestinal disorders (FGIDs) encompass a group of gastrointestinal(GI) conditions characterized by chronic or recurrent GI symptoms without biochemical or structural abnormalities[1]. The most widely known of the FGIDs include functional dyspepsia and irritable bowel syndrome (IBS), with other conditions such as functional constipation, abdominal bloating, and functional abdominal pain syndrome being increasingly recognized. FGIDs are highly prevalent,with IBS reported in about 10%-15% of the North America population, and with some studies showing up to 20% prevalence[2]. Similar prevalence rates (7.0%-20.4%) are reported for functional dyspepsia[3]. While the diseases are generally grouped based on focal primary digestive symptoms (i.e., functional dyspepsia based on upper GI symptoms), it is important to note that the intestinal tract functions as a unit, and disorders in a specific segment can produce symptoms in a separate area, for example,constipation leading to delayed gastric emptying[4]. Table 1 provides a summary of the disease phenotypes, characterized by the symptoms and pathophysiology, as well as their diagnosis and treatment. Table 2 summarizes pharmacological treatments(current or in development) for indications based on accurate phenotyping of GI disorders.
While these conditions generally do not contribute to mortality, they cause significant morbidity and often lead to extensive, often repetitive, diagnostic workups, incurring significant cost, as well as frustration for both patient and provider.Evaluation of a teaching hospital gastroenterology clinic showed that 34.9% of new patient referrals in a two-year period had a diagnosis of a FGID[5]. Preliminary data from our group show that patients undergo an average of three endoscopic procedures and 1.2 cross-sectional imaging tests [computed tomography (CT),magnetic resonance imaging (MRI) of abdomen and pelvis] prior to receiving a diagnosis of bile acid diarrhea. A large systematic review reported that up to 70%-80%of patients undergoing endoscopy for dyspepsia would be diagnosed with functional dyspepsia[6]. Similarly, in patients who met Rome I criteria for IBS, structural disease was found in only 2% by colonoscopy[7], suggesting that testing for FGIDs is over utilized.
Despite the prevalence of these conditions, diagnosis and management remain challenging due to their heterogenous nature. However, with improved diagnostic tools and increased understanding of the specific pathophysiologic mechanismsunderlying these conditions, it is possible to identify specific mechanisms among patients presenting with the same symptom complexes in the different categories of FGIDs, allowing for tailored therapy with increased chances of success.
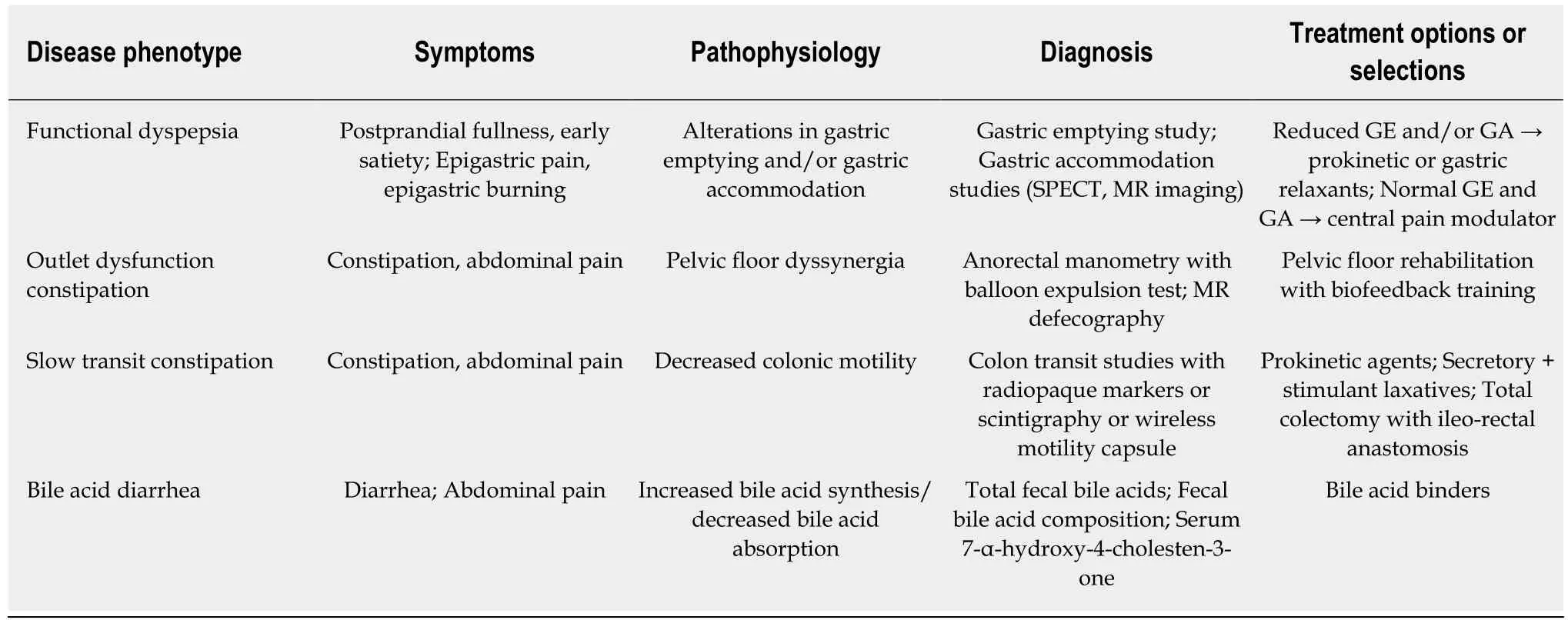
Table 1 Commonly encountered gastrointestinal diseases and their phenotypic presentations (symptoms and pathophysiology) and management principles
This review proposes an individualized approach to the management of FGIDs:understanding mechanisms that result in patients’ symptoms, utilizing appropriate diagnostic testing, and choosing targeted therapies to provide personalized care in the management of the FGID. Four decades ago, there was a plea to move towards positive symptom-based diagnosis of IBS; this led to profuse criteria for diverse symptom complexes, and the criteria have been revised and refined almost every decade since then[8]. As more specific diagnoses are identified, these disorders could be identified as specific diagnoses instead of being bundled under the “umbrella”diagnosis of FGIDs. For this review, we will follow the current convention of grouping these disorders as “functional” GI disorders, but we will also document specific phenotypes that call for specific, targeted treatments.
Understanding the pathophysiological mechanisms causing FGIDs and developing valid clinical diagnostic tests are the first steps in the process of positive disease diagnosis, moving these disorders from diagnoses of exclusion after extensive or limited evaluations to rule out organic diseases[9]. With increased recognition of the importance of peripheral mechanisms in the etiopathogenesis of IBS, there is a renaissance[10,11]in the field of FGIDs, which should lead from a hit-or-miss approach for symptom relief to the targeted, personalized treatment based on specific diagnosis and pharmacogenomics.
GASTRIC DYSFUNCTIONS AS A BASIS FOR TREATMENT IN FUNCTIONAL DYSPEPSIA
Functional dyspepsia is defined by Rome IV criteria as any combination of postprandial fullness, early satiety, epigastric pain, and epigastric burning occurring at least three days per week over the last three months, with an onset of at least six months prior to evaluation[12]. In the absence of alarm symptoms and signs, treatment can be initiated empirically without endoscopic evaluation. Functional dyspepsia is further subdivided into postprandial distress syndrome and epigastric pain syndrome, depending on whether the symptoms are associated with meal ingestion.Most patients have been treated with or tried anti-acid secretory medications by the time they see a gastroenterologist. The empiric choice follows a “hunch”, a perception by the clinician of the underlying cause of the patient’s symptoms. Indeed, it may be feasible to select a prokinetic for postprandial distress or a central neuromodulator for epigastric pain syndrome.
While there are many proposed mechanisms for the pathophysiology of functional dyspepsia, alterations in gastric function, as measured by gastric emptying (GE) and gastric accommodation (GA), have been correlated with symptoms and are potential targets for treatment. Among 1287 patients who underwent GE and GA studies,patients with delayed GE had more frequent nausea, vomiting, and weight loss, and less frequent bloating. Nausea, vomiting, and belching symptoms were significantly different among patients with normal, increased, or decreased GA. Vomiting was
more prevalent in patients with both abnormal GA and GE[13]. A meta-analysis of 25 studies showed significant associations between altered GE and nausea, vomiting,abdominal pain, and early satiety in patients presenting with upper GI symptoms[14].Importantly, a review of the current literature showed significant heterogeneity in GE and GA testing, with significant differences observed in the relationship of delayed GE with upper GI symptoms between studies that used optimal versus suboptimal methods. GE and GA testing should be conducted with appropriate meal and testing length in order to ensure accurate results[15].
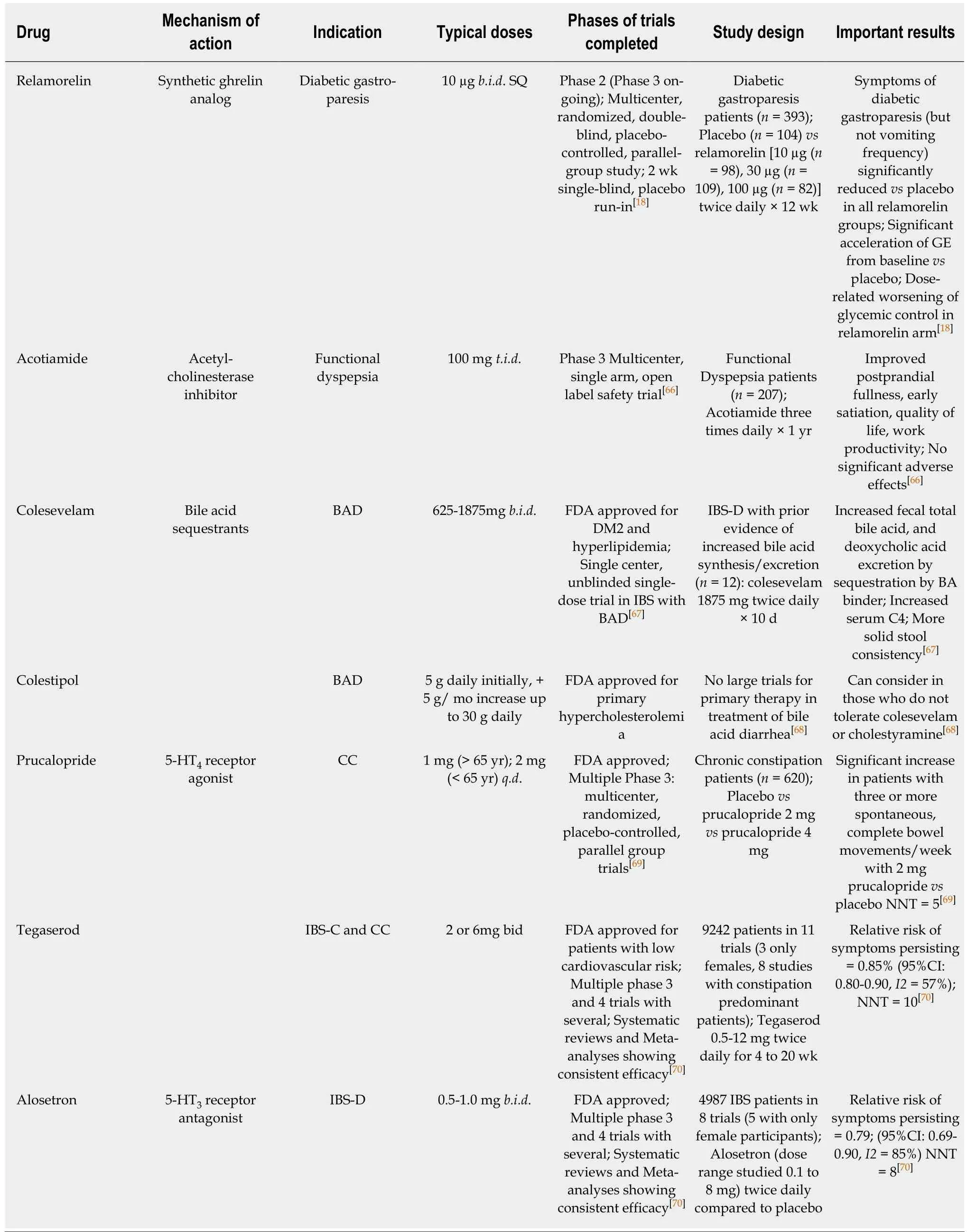
Table 2 Pharmacological treatments (current or in-development) for indications based on accurate phenotyping of gastrointestinal disorders
In patients with functional dyspepsia with altered GE and/or GA, treatments such as prokinetic medications or gastric relaxants, respectively, may be beneficial in symptom management. Conversely, in patients with upper GI symptoms, but no alteration in gastric functions, central pain modulators such as tricyclic antidepressants (nortriptyline, amitriptyline), a combination antidepressant that acts by antagonizing adrenergic α2-autoreceptors and α2-heteroreceptors as well as by blocking 5-HT2and 5-HT3receptors (mirtazapine), or an α2δ ligand (Pregabalin) may be more beneficial as initial therapy to treat duodenal hypersensitivity. It is important to note that these medications, particularly mirtazapine, also impact gastric function[16]and may provide relief by addressing underlying dysfunction as well as pain modulation.
However, there is a dearth of evidence from large phase 3 trials in the literature assessing this pathophysiology-centered approach in functional dyspepsia and a lack of effective treatments. The best proof-of-principle comes from phase 2 studies of relamorelin, albeit in patients with diabetes with gastroparesis, whose GE and symptoms improved[17,18], and from studies with acotiamide in less than 40 patients which showed concordant results between GA and symptoms[19].
MECHANISMS AND TREATMENTS OF FUNCTIONAL LOWER GI DISORDERS
Functional lower GI disorders include diarrhea-IBS (IBS-D), IBS-constipation (IBS-C),or IBS-mixed, as well as the overlapping disorders of functional diarrhea and functional constipation. The important distinguishing factor between IBS and the functional bowel alterations according to Rome IV criteria is the presence of pain associated with alteration of bowel habits with IBS diagnosis, that is, the presence of pain with alteration of bowel movements and relief of pain with defecation[20]. These“umbrella diagnoses” can be further characterized by mechanism or pathophysiology,leading to targeted treatment.
Outlet dysfunction constipation, colonic inertia and overlap with lower FGIDs with constipation
It is recognized that, among patients with lower FGIDs and constipation, at least 30%suffer from pelvic floor dyssynergia, causing outlet dysfunction constipation, and 5%from colonic inertia (with neural or ICC loss in myenteric plexus), causing slow transit constipation. Importantly, up to 50% of patients with outlet dysfunction constipation have slow transit constipation as a result of the evacuation disorder[21]. Therefore, the diagnostic assessment should begin with anorectal testing, including digital rectal exam, anorectal manometry and balloon expulsion testing. A digital rectal exam,performed by an experienced clinician, can correctly identify features such as high anal sphincter tone and paradoxical contraction of the pelvic floor that is associated with abnormal anal relaxation or abnormal rectoanal pressure differential. The balloon expulsion time of 60 seconds has a low sensitivity for identifying rectal evacuation disorder[22]. If, on digital rectal exam, there is concern about mucosal intussusception, pelvic organ prolapse, or descending perineum syndrome[23]which is increasingly recognized in Ehlers-Danlos syndrome[24], magnetic resonance defecography can be pursued to evaluate the rectal region during active evacuation[25].If anorectal evaluation is normal, evaluation for slow transit constipation can be considered, utilizing radiopaque markers, colonic transit scintigraphy, or wireless motility capsules[26].
In patients who show abnormal parameters on anorectal manometry or with failure to pass a rectal balloon in 60 s, treatment of pelvic dyssynergia should be undertaken with pelvic floor rehabilitation. The benefit of pelvic floor rehabilitation largely lies in biofeedback training, in which patients are taught to control their pelvic floor muscles and anal sphincters to reverse maladaptive learning including paradoxical movements or relax high pressures, depending on the manometric abnormality.Biofeedback training has been reported to improve more than 60% of patients with constipation due to pelvic floor dyssynergia; patients who used digital maneuvers and those with lower baseline levels of bowel satisfaction were more likely to have treatment success[27]. Home-based biofeedback retraining has been as effective as office-based retraining[28], which was previously shown to be superior to diet, exercise,and laxatives as standard therapy for constipation[29].
In patients with slow colonic motility alone who are refractory to treatment with laxatives, further testing can be undertaken with colonic manometry and barostat studies to evaluate colonic motor activity, including meal-induced gastrocolonic response and response to stimulant laxatives and cholinesterase inhibitors(neostigmine)[30,31]. If there is evidence of colonic motor activity in response to physiological and pharmacological stimuli, treatment with the oral cholinesterase inhibitor, pyridostigmine, can be considered[32]. Recently, the selective serotonin-4 (5-HT4) receptor agonist, prucalopride, which stimulates colonic peristalsis and enhances bowel motility, received FDA approval and can be considered in patients with evidence of reduced colonic motility. If there is no evidence of normal motor activity and no response to stimulation with neostigmine or supervised therapeutic trial,laparoscopic colectomy with ileorectal anastomosis can be considered.
Bile acid diarrhea
While bile acid diarrhea is usually recognized in patients with ileal disease or ileal resection, recent studies have documented that between 25% and 50% of patients with functional diarrhea or IBS-D have bile acid diarrhea, and have symptom improvement on bile acid sequestrants[33]. In primary or idiopathic bile acid malabsorption, also known as type 2 bile acid malabsorption, there is an increased fecal load of bile acids in the absence of ileal or other structural gastrointestinal diseases. While the etiology of the increase is unclear, the prevailing theories include a deficiency in feedback inhibition of bile acid synthesis by fibroblast growth factor (FGF)-19 causing excess hepatic production due to reduced ileal enterocyte mRNA expression[34], or genetic variants in the hepatocyte receptor or associated protein (KLB and FGFR4)[35]that are activated by FGF-19 to reduce CYP7A1, the rate-limiting enzyme in the synthesis of bile acids. These bile acids act in the colon to increase colonic mucosal permeability,water secretion, mucus production, and to accelerate colonic motility[36].
To assess patients for bile acid diarrhea, fecal bile acid load can be evaluated directly by measurement of total and individual fecal bile acids, with excretion of >2337 μmol per 48 h or > 10% primary bile acids (chenodeoxycholic acid, deoxycholic acid) as an indication of bile acid malabsorption. Mild elevations in total bile acids should be interpreted with caution, as increased colonic transit may lead to reduced passive absorption of bile acids in the colon and an increase in the fecal levels[37]. If available, serum C4 (7-alpha-hydroxy-4-cholesten-3-one) is a simple blood test measuring bile acid synthesis, with a sensitivity of 90% and specificity of 79% for the diagnosis of bile acid malabsorption[38]. This test should be performed on a fasting serum sample collected in the morning before 10:00 a.m., due to diurnal variability.
If diagnosed, bile acid diarrhea can be treated with intraluminal bile acid binders,cholestyramine and colestipol, though evidence of efficacy comes mainly from openlabel studies. These intraluminal bile acid binders have shown benefit in bowel symptoms and global symptoms in the treatment of patients with IBSD with evidence of bile acid malabsorption, but are limited by their poor palatability. Colesevelam is better tolerated and has shown efficacy in improvement in stool consistency, but its use may be limited by cost[36].
Disaccharidase malabsorption
Worldwide, about 65% of adults lose the ability to digest lactose, with ethnically determined prevalence ranging from less than 10% in Northern Europeans to over 90% in East Asians[39]. In the absence of adequate lactase at the intestinal brush-border,lactose is unable to be cleaved to monosaccharides (glucose and galactose) and, thus,it reaches the colon unabsorbed. In the colon, lactose is broken down by commensal bacteria, producing hydrogen gas and symptoms of abdominal pain, distension,borborygmi, flatus, and diarrhea[40]. Lactase deficiency can be evaluated with a simple hydrogen breath test following lactose load. While this diagnosis is commonly known, studies have found that symptoms in up to 25.8% of patients diagnosed with IBS-D were related to lactose deficiency, and 52% of patients were unaware of symptoms association with lactose ingestion[41]. Once diagnosed, most patients are able to tolerate lactose intake equivalent to 240 mL of milk without symptoms,particularly, if ingested in divided amounts rather than a single dose[42]. Otherwise,dietary avoidance or the use of digestive aids can provide adequate symptom control.
While sucrose-isomaltase deficiency is an uncommon congenital condition, the diagnosis is often not recognized, and children can present with unexplained signs and symptoms which persist into adulthood. Similar to undigested lactose, arrival of these non-absorbed disaccharides in the colon can lead to gas fermentation by bacteria, as well as osmotic diarrhea. Malabsorbed sugars, such as fructose and lactose, lead to clusters of gastrointestinal symptoms, rather than symptoms typically associated with brain dysfunction[43]. Other uncommon genetic carbohydrate intolerances include glucose-galactose malabsorption. These conditions can be severe enough to cause failure to thrive and malnutrition in children, but tolerance can improve as the children age. In patients with prolonged history of symptoms,particularly if related to meals, diagnostic evaluation can be pursued with disaccharidase activity assays on proximal small bowel biopsies[44].
Abdominal pain, bloating and the low fermentable oligosaccharides, disaccharides,monosaccharides and polyol diet
Among patients with predominant pain or bloating, the role of fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAPs) may be considered. As above, lactase insufficiency should first be evaluated prior to implementing the nutritionally-restrictive full low-FODMAP diet. Biologically,humans are unable to enzymatically cleave the fructose-fructose bonds needed to break down the oligosaccharides which compose fructans and galactans. Polyols, or sugar alcohols, are also incompletely absorbed and can reach the colon intact. These components can be fermented similar to undigested lactose and cause osmotic diarrhea, leading to symptoms of IBS-D. Monosaccharides and disaccharides are generally absorbed by brush border transporters and enzymes, and, in the absence of congenital deficiencies above, should not cause significant GI distress.
Once a low FODMAP diet is implemented, if symptoms are controlled, dietary components should be slowly reintroduced as tolerated in order to allow patients a larger variety of nutritional sources and improved quality of life. If symptoms continue to be uncontrolled or if patients manifest other features, concern for chronic pain syndrome and central neuromodulators would be indicated. Dietary fiber supplementation may be beneficial for patients with IBS-C or chronic constipation. In addition, prebiotics, ingredients unable to be digested by the human intestinal tract but that support the growth of intestinal microbiota, may play a role in improvement of the gut microbiome[45,46]. Conversely, ultra-processed foods may be associated with a higher risk of IBS[47]. Dietary fibers, as well as prebiotics, are often empirically utilized, and it is unclear whether phenotyping can identify the best candidates for these therapies.
Brain-gut permeability-microbiome interactions
An authoritative review in 2014 opined that it was unclear whether IBS symptoms are caused by alterations in brain signaling from the intestine to the microbiota or primary disruption of the microbiota, and whether they are involved in altered interactions between the brain and intestine during development[48]. Recent data support these interactions in part through increased intestinal permeability. This interaction likely underlies the strong association between FGIDs and psychological disorders, with up to 50%-94% of IBS patients carrying diagnoses of general anxiety disorder or major depression[49]. De Palma et al. showed that engraftment of fecal microbiota from IBS patients into germ-free mice led to development of not only increased GI transit and gut barrier dysfunction, but also anxiety-like behavior compared to those receiving fecal microbiota from control patients[50]. In addition to central neuromodulators, patients with concomitant psychological disorders may benefit from cognitive behavior therapy or hypnotherapy[51].
Studies in vitro of permeability of colonic mucosa[52]from patients with IBS suggested that there is increased paracellular permeability to51Cr-EDTA; these data confirm a significant literature documenting increased intestinal or colonic permeability in IBS using orally administered probe molecules, principally saccharides[53]. Bednarska et al[52]also showed increased transcellular permeability to live bacteria. Gaps among terminal ileal epithelial cells in IBS or among duodenal cells have also been documented in response to food allergens[54,55]. These data may provide the rationale for bacteria or their toxins impacting brain function, as demonstrated through correlations of permeability and brain structure and function[56]. A probiotic[57], B. infantis M-63, has seemed to be effective in improving mental health in patients who developed IBS after floods, and this may be due to restoration of microbial balance and the gut-brain axis.
Fecal microbiota transplantation has also been explored as a potential treatment of FGIDs, particularly IBS, with the intent of restoring the microbiome to a healthy state[58]. Further studies are needed to help determine the appropriate goal of the microbiota change and the composition of “healthy gut” microbiota. Rigorous trials need to be conducted to evaluate the safety of these transplants for use in FGIDs,which generally carry low mortality risk, as well as to evaluate the long-term durability of results.
For this field to advance, we require further validated measurements of permeability that are applicable noninvasively in clinical practice as an essential first step, followed by provision of evidence that interventions (dietary, probiotic,microbial transplant, or pharmacological) can restore barrier function to normal. At present, none of the three dimensions (intestinal permeability, microbiome or brain imaging) is applicable in the personalized medicine arena.
THE “-OMICS” AND PRECISION MEDICINE
Pharmacogenomics and drug pharmacokinetics
Pharmacogenomics evaluates the impact of changes in an individual patient’s genetic code on drug metabolism or on a therapeutic target. Genetic differences in drug metabolism can lead to increased or decreased response to a standard dose of medication in different patients and may lead to unintended toxicity or poor response, respectively. The cytochrome p (CYP) 450 enzymes are responsible for phase I metabolism of numerous drugs, and genetic variations in several of these enzymes have been implicated in response to treatment in FGIDs.
Central pain modulators, including the tricyclic antidepressants and the selective serotonin reuptake inhibitors (SSRIs), are frequently used to treat pain in patients with FGIDs. These drugs are metabolized by the CYP2D6 enzyme, which has more than 100 genetic variations that determine functionality of the enzymes. The number of functional CYP2D6 genes was shown to correlate with nortriptyline metabolism[59],but the clinical implications of this observation are still unproven in clinical trials or practice, except in individual patients.
CYP2C19 is responsible for inactivation of proton pump inhibitors, as well as the H2receptor antagonist, cimetidine. Increased activity variants of CYP2C19 can lead to poor response to proton pump inhibitors (PPIs) in patients with functional dyspepsia.In these cases, rabeprazole should be considered, as it is metabolized through the CYP3A4 system. The CYP3A4 system is also responsible for the metabolism of alosetron, a 5HT3receptor antagonist used in treatment of IBS-D. Decreased activity variants of CYP3A4 or concomitant use of benzodiazepines, which are also metabolized by the same enzyme, may lead to increased drug effects and higher risk of toxicity[60].
Mutations and genetic variants in FGIDs
While specific genetic variants have not been identified as therapeutic targets, there are several polymorphisms which alter GI transit and may influence the development of FGIDs. The serotonin-transporter protein (SERT) is located on a presynatic neuron and clears 5-HT from the synaptic cleft, limiting downstream activation of receptors that stimulate colonic transit. Allelic variants of the gene 5-HTTLPR, which determines SERT synthesis, can cause decreased SERT protein and increased serotonergic activation and accelerated colonic transit[61]. The presence of variations causing decreased SERT has also been seen to decrease the response to the 5HT3receptor antagonist, alosetron, and to increase the response to the 5HT4receptor agonist, tegaserod, both used in the treatment of IBS-C[62].
Mucosal gene expression and FGIDs
Several studies have now evaluated mucosal gene expression in FGIDs, particularly in patients with IBS. In the IBS-D cohort, prior studies have shown altered transcription of proteins involved in ion transport, barrier function, immune regulation, and mast cell activation in jejunal and colorectal mucosa[63,64]. Further study of these changes may allow improved understanding of the pathophysiology of IBS and potentially influence development of future therapeutic targets.
LIMITATIONS
Recommendations suggested in our review are limited by the lack of availability of“deep phenotyping”, even in specialty or academic centers. For example, nuclear medicine SPECT imaging and MRI for measurement of gastric accommodation are only available or offered in limited facilities. In addition, there is currently significant heterogeneity in testing protocols and interpretation of results which leads to lack of standardization, both in clinical data and in research. This is often observed in gastric emptying studies where different protocol meals are utilized, leading to different expected parameters. Similarly, balloon expulsion times in anorectal manometry have“normal” cut offs ranging from 60 s to up to 3 min in different centers. Lastly, there is currently a lack of robust evidence that understanding or deeply characterizing patient phenotype will lead to improved patient outcomes, partly due to lack of effective treatments available, particularly for gastroparesis and gastric dysaccommodation. However, we perceive that the future clinical practice will be enhanced by standardization of measurements in research and clinical practice and will facilitate development of new targeted therapies, and ultimately improve patient care.
CONCLUSION
In summary, the time for personalization of treatments for FGIDs, based on “deep phenotyping”, is here. FGIDs should no longer be considered diagnoses of exclusion following extensive structural work-up. Instead, after a thorough history, patients should receive targeted assessment and testing, depending on their symptom profile,to evaluate the likely subtypes of FGIDs, with subsequent targeted treatment. This shift in approach will improve patient compliance, decrease costs for work-ups[65], and potentially decrease both patient and provider frustration. Pharmacogenetics is currently clinically relevant in the use of central neuromodulators and PPIs, and evaluation for genetic variants should be considered in patients who are not responding as expected to treatment. The role of genetics in the management of FGIDs is still a maturing field. With greater understanding of the pathophysiology of these disorders and validation of clinically-applicable diagnostic tests, patient-based research will provide more personalization of diagnosis and management for patients with FGIDs. As the etiologies and pathophysiologies of these disorders are identified and symptoms are able to become classified under specific diagnoses, we anticipate that the umbrella category of “functional” GI disorders will ultimately be replaced by separate and specific diseases. The examples of slow transit constipation, rectal evacuation disorders and bile acid diarrhea already demonstrate the clinical relevance of these phenotypes to personalize medicine.
杂志排行
World Journal of Gastroenterology的其它文章
- Nutritional and vitamin status in patients with neuroendocrine neoplasms
- Quest for the best endoscopic imaging modality for computerassisted colonic polyp staging
- Short hairpin RNA-mediated knockdown of nuclear factor erythroid 2-like 3 exhibits tumor-suppressing effects in hepatocellular carcinoma cells
- MicroRNA-596 acts as a tumor suppressor in gastric cancer and is upregulated by promotor demethylation
- Performance of risk stratification systems for gastrointestinal stromal tumors: A multicenter study
- Utility of linked color imaging for endoscopic diagnosis of early gastric cancer
