In vivo imaging of structural, metabolic and functional brain changes in glaucoma
2019-02-13AnishaKasiMuneebFaiqKevinChan
Anisha Kasi, Muneeb A. Faiq, Kevin C. Chan,
1 NYU Langone Eye Center, Department of Ophthalmology, NYU School of Medicine, NYU Langone Health, New York University, New York, NY, USA
2 Department of Radiology, NYU School of Medicine, NYU Langone Health, New York University, New York, NY, USA
3 Center for Neural Science, Faculty of Arts and Science, New York University, New York, NY, USA
Abstract Glaucoma, the world's leading cause of irreversible blindness, is a condition for which elevated intraocular pressure is currently the only modifiable risk factor. However, the disorder can continue to progress even at reduced intraocular pressure. This indicates additional key factors that contribute to the etiopathogenesis. There has been a growing amount of literature suggesting glaucoma as a neurodegenerative disease of the visual system. However, it remains debatable whether the observed pathophysiological conditions are causes or consequences. This review summarizes recent in vivo imaging studies that helped advance the understanding of early glaucoma involvements and disease progression in the brains of humans and experimental animal models. In particular, we focused on the non-invasive detection of early structural and functional brain changes before substantial clinical visual field loss in glaucoma patients; the eye-brain interactions across disease severity; the metabolic changes occurring in the brain's visual system in glaucoma; and, the widespread brain involvements beyond the visual pathway as well as the potential behavioral relevance. If the mechanisms of glaucomatous brain changes are reliably identified, novel neurotherapeutics that target parameters beyond intraocular pressure lowering can be the promise of the near future,which would lead to reduced prevalence of this irreversible but preventable disease.
Key Words: glaucoma; intraocular pressure; eye-brain-behavior relationship; irreversible blindness; magnetic resonance imaging; metabolic brain changes; sensitivity; disease progression
An Unmet Need for Glaucoma Detection and Treatment in the Brain
Glaucoma is the leading cause of irreversible blindness with around 70 million sufferers worldwide to date, up to an estimated 111.8 million by 2040 (Tham et al., 2014). It is a condition for which elevated intraocular pressure is currently the only modifiable risk factor. While intraocular pressure-lowering medications and surgeries are clinically approved options for glaucoma treatment, the disorder can continue to progress even at reduced intraocular pressure(Susanna et al., 2015). This indicates other unexplored key factors that contribute to the disease onset and progression.These factors may range from stress and gene expression derangements to hormonal imbalance, inflammatory markers, aging processes and cardiovascular dysfunction. Apart from the systemic correlates, glaucoma has recently been considered a neurodegenerative disease of the visual system.Since the first case report in 2006 showing volumetric loss in the optic nerve, lateral geniculate nucleus and visual cortex of an advanced glaucoma patient (Gupta et al., 2006), there is a growing amount of literature suggesting that glaucoma affects not only the eye, but also the brain trans-synaptically (Sponsel et al., 2014; Lawlor et al., 2018). However, it remains debatable whether there is early involvement of the brain in glaucoma, how the brain interacts with the eye across disease severity, and whether these brain changes are a cause or a consequence (Lawlor et al., 2018). These questions have defined the goal of recent neuroimaging studies that aim at unveiling the structural, metabolic and functional aspects of glaucomatous brain damages in different disease stages (Figures 1 and 2). If early glaucomatous brain changes and their underlying mechanisms of disease progression can be reliably identified, then novel neurotherapeutics that target parameters beyond intraocular pressure lowering may be the promise of the near future, which would lead to reduced prevalence of this irreversible but preventable disease.
Brain Involvements in the Early Stages of Glaucoma
In order to investigate whether glaucoma involves the brain early, recent studies have combined the use of advanced neuroimaging and statistical modeling to evaluate the structural and functional brain changes in patients with different degrees of vision loss. For example, by applying segmented regression analysis onto functional magnetic resonance imaging (MRI) and standard automated perimetry in glaucoma patients and healthy subjects, we found that reduced visual cortex activity occurred before patients showed substantial visual field impairment (Murphy et al., 2016). This indicates that clinical visual performance remains at a steady level even as cortical activation begins to diminish in glaucoma,whereas visual field loss becomes detectable when reduction in visual cortex activation advances beyond a tipping point.Interestingly, a recent diffusion tensor MRI study also revealed similar segmented relationships between white matter structural abnormalities and visual field functional loss in normal tension glaucoma (Wang et al., 2018). Taken together,these observations suggest that glaucoma deterioration is already present in the brain before substantial vision loss can be detected clinically using currently available testing methods.Such evidence is important as it opens up new opportunities to examine and target early changes in the brain apart from the eye before clinical symptoms emerge and worsen in the later stages. Given that glaucoma is, as of now, an irreversibly blinding disorder, combining brain imaging with ophthalmic imaging assessments such as retinal nerve fiber layer (RNFL)and macular ganglion cell-inner plexiform layer (GCIPL)thickness measurements may also help develop algorithms for more accurate glaucoma prediction to guide timely interventions for substantial rescue of vision in glaucoma.
Interactions between Eye and Visual Brain Across Glaucoma Disease Severity
Despite the identification of a threshold and the interphase dynamics between neuroimaging and visual field measurements, the glaucomatous mechanisms underlying the reported biomarkers have not been clearly determined. For example, possible explanations for the decreased activation of the visual cortex include decreased visual input from the retina, synaptic loss in the lateral geniculate nuclei, degeneration in the visual cortex, or some combination thereof. In order to investigate the characteristics of eye-brain interactions in glaucoma etiopathogenesis, recent studies have examined initially the specificity of multi-parametric imaging assessments at various stages of the disease. When comparing visually evoked brain activity in functional MRI to segmented retinal layer thickness obtained by optical coherence tomography, the primary visual cortex exhibited stronger associations and more severe functional deficits than higher-order visual brain areas in glaucoma (Murphy et al., 2016). This suggests impaired bottom-up processing of the visual cortex in glaucomatous neurodegeneration. Additionally, using linear mixed effects modeling, a tighter fit was obtained when comparing between visual cortex activity and macular GCIPL thickness than between visual cortex activity and peripapillary RNFL thickness, indicative of a stronger association between visual cortex activity and macular GCIPL in contributing to visual field loss (Murphy et al., 2016).Such differences in association strength may be attributed to the larger proportion of sensory input from the macula to the visual brain due to cortical magnification as compared to a more diffuse input from the surroundings of the optic nerve head in peripapillary measurements. In contrast, volumetric analysis of the anterior visual pathway from anatomical MRI showed a reverse pattern, whereby shrinkage of the optic nerve and optic chiasm in glaucoma was significantly associated with retinal thinning in peripapillary RNFL, but not macular GCIPL (Trivedi et al., 2018). The severity of white matter abnormalities in diffusion tensor MRI also correlated with RNFL thickness (Wang et al., 2018). It may,therefore, be speculated that peripapillary RNFL, volumetric MRI of the optic nerve and optic chiasm, and diffusion tensor MRI may reflect global changes in glaucomatous neurodegeneration along the visual pathway over a wider visual field, whereas macular GCIPL and task-evoked functional MRI may represent localized changes corresponding to the central vision. Since glaucomatous visual field defect often starts from the periphery and affects the center gradually as disease progresses, multi-parametric imaging analysis of different anatomical locations in the eye and the brain may be useful for monitoring the sequences of the pathological events within the visual system. Apart from early glaucoma detection, progressive RNFL changes from advanced to endstage glaucoma are often undetectable due to the intrinsic limitation of the floor effect in optical coherence tomography. Measuring macular GCIPL thickness and the visual cortex activity may help better reveal the process of retinal ganglion cell dysfunction before the remaining central visual field deteriorates irreversibly. Such an approach is crucial in both patient management and vision preservation.
Metabolic Brain Changes in Glaucoma
To identify neurochemical changes occurring in the brain's visual system in glaucoma, recently, proton magnetic resonance spectroscopy and positron emission tomography have been used across different species. Consistent with our preclinical proton magnetic resonance spectroscopy study in an experimental rat model of chronic glaucoma (Chan et al., 2009), we identified that cholinergic and glutamatergic abnormalities may be involved in the mechanisms of vision loss in the visual cortex of glaucoma patients (Murphy et al.,2016). Positron emission tomography studies also demonstrated glial activation and glucose hypometabolism in the brains of glaucoma patients and non-human primate models (Shimazawa et al., 2012; Murai et al., 2015). Cholinergic stimulation has been shown to alleviate clinical symptoms,reduce glial activation and enhance functional brain responses to visual tasks in other neurodegenerative diseases such as Alzheimer's disease. Overall, these results merit further investigations on the role of cholinergic stimulation in glaucoma.Intervention with choline supplements (van der Merwe et al., 2016) and insulin (Faiq and Dada, 2017) may be potential candidates of such treatment approach to improve visual brain responses and visual outcomes in glaucoma.
Widespread Brain Changes and Behavioral Relevance in Glaucoma
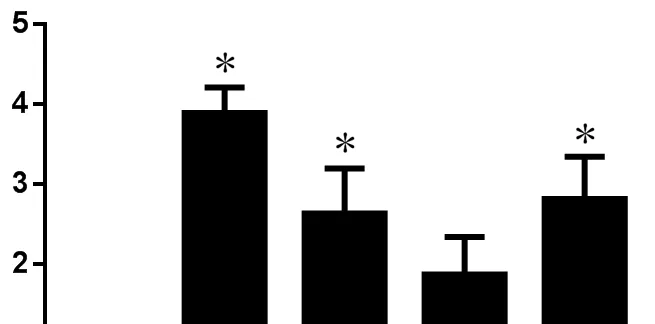
Figure 1 Structural brain magnetic resonance imaging (MRI) in early and advanced glaucoma using anatomical MRI (A-F) and diffusion tensor MRI (GJ).

Figure 2 Blood-oxygenation-level-dependent (BOLD) functional magnetic resonance imaging (MRI) in glaucoma.
MRI is non-invasive with no depth limitation, which allows multi-parametric monitoring of glaucomatous changes throughout the whole brain. Apart from the visual system,increasing evidence suggests that glaucoma may be associated with widespread changes in the brain (Frezzotti et al., 2016; Murphy et al., 2016; Wang et al., 2018); however,its causes and the potential clinical and behavioral effects remain unclear. It is known that patients with glaucoma are at an increased risk of falling, while the brain processes needed for the integration of sensory information relevant for balance require attention-related resources, which may be altered in glaucoma (Nuzzi et al., 2018). With this premise, we attempted to probe how glaucoma may impair the brain structurally and functionally within and beyond the visual pathway, and whether the brain changes in glaucoma are associated with balance and mobility impairments.Our preliminary results suggest that patients with advanced glaucoma may have difficulty prioritizing balance during challenging postural conditions, whereas brain connectivity alterations in patients with glaucoma may be related to the attentional control of standing balance (Cham et al., 2018).These findings are pivotal in getting a pragmatic insight into the central mechanisms of visuomotor impairments in glaucoma and may ultimately guide interventions related to postural diffiiculties to individual patients.
Conclusion and Future Perspectives
The preliminary findings described in this article can impact future development and applications of neuroimaging techniques for identifying early glaucoma mechanisms,detecting and monitoring pathophysiological events and determining eye-brain-behavior relationships over the natural history of the disease. Currently, most glaucoma neuroimaging studies are cross-sectional and toward later stages,with a limited number of studies spanning across disease severity. Therefore, it has not been confirmed whether the observed structural and functional brain changes were caused by glaucoma. Also, it remains inconclusive to directly infer the onset threshold of glaucoma from the determined tipping points in segmented regression modeling between imaging and perimetry. It is also likely that the clinical visual field loss becomes detectable only after reaching a certain threshold due to differences in sensitivity across measuring modalities.More sensitive clinical visual testing is needed to determine the early functional changes and the corresponding contributions from the eye and the brain. Since glaucoma is a chronic disease that progresses slowly over years, longitudinal measurements of a large sample over time are essential to determine the temporal characteristics and causal relationships between biomarkers in the brain and glaucoma with suffiicient statistical power. Such longitudinal studies and the testing of targeted neurotherapeutics can also be performed preclinically in well-controlled experimental glaucoma models,which are currently on the go (Yang et al., 2018). Advanced and higher-order neuroimaging modalities such as diffusion kurtosis imaging, chemical exchange saturation transfer,magnetization transfer MRI, arterial spin labeling, and dynamic contrast-enhanced MRI can be used in conjunction to conventional structural and functional MRI at higher spatial and temporal resolutions to determine the pathophysiology of brain in glaucoma with improved specificity. Other non-MRI neuroimaging modalities, such as fluorescence imaging of apoptosis and second harmonic generation microscopy of microtubule cytoskeleton disruption have also been recently used to provide specific imaging biomarkers for detecting glaucomatous neurodegeneration in the retinal ganglion cell axons in vivo. It is also possible that the sites of injury and pathogenic mechanisms of glaucoma are not only restricted to brain tissues, but also involving organic and subtle etiologies. Therefore, additional systemic and psychogenic factors may need to be investigated along with brain changes. In the future, if the mechanisms of glaucomatous brain changes are reliably identified, new neurotherapeutic approaches can be developed to prevent, slow down or even restore functional loss in glaucoma. Intensified research efforts on glaucoma neuroimaging are, therefore, warranted to help reduce the global prevalence and burden of the disease.
Acknowledgments:We thank all collaborators who contributed to our research papers upon which the present commentary is based.
Author contributions: Manuscript concept: KCC; literature search and initial manuscript preparation: AK and KCC; critical revision and final approval of the manuscript: AK, MAF and KCC.
Conflicts of interest: None declared.
Financial support:This work was supported by the National Institutes of Health R01-EY028125 (Bethesda, MD, USA) (to KCC); BrightFocus Foundation G2013077 and G2016030 (Clarksburg, MD, USA) (to KCC);and Research to Prevent Blindness/Stavros Niarchos Foundation International Research Collaborators Award (New York, NY, USA) (to KCC).
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Plagiarism check:Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Open access statement: This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Non-Commercial-ShareAlike 4.0 License, which allows others to remix, tweak,and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
杂志排行
中国神经再生研究(英文版)的其它文章
- The role of Epstein-Barr virus in multiple sclerosis:from molecular pathophysiology to in vivo imaging
- The metabolome identity: basis for discovery of biomarkers in neurodegeneration
- Neuroinflammation as a target for glaucoma therapy
- Basics on the use of acid-sensing ion channels'inhibitors as therapeutics
- Role of axon resealing in retrograde neuronal death and regeneration after spinal cord injury
- Rehabilitation following spinal cord injury: how animal models can help our understanding of exerciseinduced neuroplasticity
