Operative complications and economic outcomes of cholecystectomy for acute cholecystitis
2019-02-12ChristopherRiceKrishnamurthyVaishnaviCeliaChaoDanielJupiterAugustSchaefferWhitneyJensonLanceGriffinWilliamMileski
Christopher P Rice, Krishnamurthy B Vaishnavi, Celia Chao, Daniel Jupiter, August B Schaeffer,Whitney R Jenson, Lance W Griffin, William J Mileski
Abstract
Key words: Acute cholecystitis; Tokyo guidelines; Cholecystectomy; Complications;Delayed cholecystectomy
INTRODUCTION
Recent recommendations for early or same admission (SA) cholecystectomy[1-8]have become standard practice based mainly on a shorter hospital stay and thus a presumed economic benefit[9]. However, patients who present with acute cholecystitis are a heterogeneous population and for some patients, emergent cholecystectomy may result in complications that might be mitigated if the procedure were delayed.The Tokyo Guidelines (TG) were developed to guide the treatment of acute cholecystitis and to use clinical parameters at presentation to predict risk of complications associated with disease severity. TG defines the criteria for a clinical diagnosis of acute cholecystitis and disease severity grading[10]. The guidelines, first published in 2007, have been revised in 2013 and most recently in 2018. The grading system for TG13 is the same as TG18: Mild cholecystitis (Grade 1) refers to acute cholecystitis in a healthy patient with mild inflammatory changes in the gallbladder,fever and or elevated white blood cell count (WBC), and no organ dysfunction.Moderate cholecystitis (Grade 2) is associated with complaints > 72 h, a WBC ≥ 18K,signs of marked local inflammation (e.g., gangrenous or emphysematous cholecystitis,pericholecystic or hepatic abscess, biliary peritonitis) or a palpable tender mass in the right upper quadrant of the abdomen. Severe cholecystitis (Grade 3) is defined by concurrent organ system dysfunction. TG13/18 severity grading has been shown to correlate with hospital length of stay, conversion to open cholecystectomy, and higher morbidity and mortality[10].
The World Society of Emergency Surgery (WSES)[1]acknowledges that there are no validated clinical scores to guide clinicians for the evaluation of surgical risk for early operative intervention of acute calculus cholecystitis. For example, one criticism of the TG is that either drainage or cholecystectomy can be performed for severity Grade 2[11], without specific practice guidelines indicating which therapeutic option is better.Nonetheless, the TG grading correlates with morbidity and mortality[10,12]. Further validating the preoperative value of TG grading, Ambeet al[13]demonstrated that increasing severity Tokyo grades significantly correlated worse disease with histologic criteria.
Using the TG severity of the disease grading system, we compared the outcomes of patients operated on during the SAvsdelayed. Since patients with a higher grade of disease (Grades 2 and 3) are expected to have a greater rate of complications and longer length of hospital stay (compared to Grade 1), we hypothesized that the economic benefit of early cholecystectomy in the setting of complications would be negated.
MATERIALS AND METHODS
Under an Institutional Review Board-approved protocol, we retrospectively reviewed 2118 medical charts of all patients who underwent a cholecystectomy over an 8.5-year period (February 2010 to August 2018) at the University of Texas Medical Branch(UTMB Health) - a tertiary referral center located in Galveston, Texas. Patient information was retrieved using the UTMB Health databases for acute care surgery,billing, and Revenue Cycle Operations. Patient medical charts were reviewed directly from UTMB Health's electronic medical records (EMR, Epic Hyperspace 2017, Epic Systems Corporation). A total of 26 faculty surgeons performed the cholecystectomies during this time period.
Inclusion criteria for each acutely ill patient consisted of a diagnosis of acute cholecystitis upon presentation to any UTMB Health emergency department with admission or direct admit to the hospital. All patients underwent a cholecystectomy performed either during their index admission (i.e., SA) or electively after presenting with acute disease (i.e., delayed cholecystectomy). For comparison only, we also abstracted the charts of all patients who underwent an elective cholecystectomy (nonacute) for a diagnosis of sub-acute conditions (e.g., chronic cholecystitis (biliary colic),cholelithiasis, biliary dyskinesia, porcelain gallbladder, or gallbladder polyp).Exclusion criteria were acutely ill patients without a diagnosis of acute cholecystitis and patients < 18 years of age. We also excluded 27 patients who had a diagnosis of acute cholecystitis but underwent preoperative cholecystotomy tube placement because these patients were deemed to be poor operative candidates initially and were temporized with a drainage procedure first.
We collected information on baseline patient characteristics including demographics, insurance status, comorbidities, diagnoses, health behaviors, dates of presentation, body temperature at presentation, hospital lengths of stay, laboratory values at presentation, complications. Outcome calculations were rates of cholecystectomy on index admission, complication rates, readmission rates, and charges.
We identified data regarding charges incurred for each case from UTMB Health Revenue Cycle Operations using Current Procedural Terminology (CPT) codes,International Classification of Diseases (ICD) codes, medical record numbers of the 1882 patients involved in the study, and the operative dates between April 2013 to August 2018 (hospital charges prior to April 2013 were not activated in our electronic medical record system). The CPT codes used were 47562, 47563, 47600, 47605, 47480,47564, 47490, and 47570, which represent laparoscopic and open cholecystectomies(with or without an intraoperative cholangiogram), percutaneous or open cholecystostomies (with or without exploration, drainage, or removal of calculus), and cholecystenterostomies, respectively. The ICD-10 included were K81.9, K81.2, K81.1,K81.0, K80.80, K80.60, K80.50, K80.44, K80.20, K80.18, K80.12, K80.10, and K80.00 along with the corresponding ICD-9 (that matched the aforementioned ICD-10) codes.These ICD codes represent combinations of acute and chronic, obstructive and nonobstructive cholecystitis, cholelithiasis, cholangitis, and choledocholithiasis. All charges (which include any admission, clinic visit, urgent care visit, related procedures) were captured for each patient after April 2013 (i.e., we were unable to obtain charge data for 23.5% of the cohort).
Patients were diagnosed with acute cholecystitis and stratified by severity using the latest TG18 criteria[10]. The diagnosis is based on local signs of inflammation (e.g.,Murphy's sign or right upper quadrant mass, pain, or tenderness), systemic signs of inflammation (e.g., fever or elevated WBC), and characteristic imaging findings. TG18 categorizes acute cholecystitis by Grades 1, 2, and 3 representing mild, moderate, and severe, respectively.
Statistical analysis
We conducted our evaluation by means of descriptive statistics using univariate and bivariate analyses of continuous and categorical variables. Bivariate comparison between the groups was analyzed using the Student'st-tests, one-way ANOVA, Chisquared tests, and Fisher's exact tests, where appropriate. We constructed a multivariate model on the covariates potentially predictive of complications with aPvalue on bivariate comparison of ≤ 0.2. APvalue of < 0.05 was considered statistically significant. Patient data was exported into a comma-separated value format to be imported in to R for analysis; all analyses were executed in the R statistical package(R, Developmental, Core, Team. R: A Language and Environment for Statistical Computing 2015; available at http://www.R-project.org).
RESULTS
Five hundred fifty-four patients met criteria and were included in the study. Four hundred eighty-six (87.7%) underwent an SA cholecystectomy while 68 patients(12.3%) received delayed operative management. Table 1 shows the demographics and patient characteristics of the two groups. Age, gender, race, ethnicity, body mass index, preexisting comorbidities, alcohol use, smoking status, and rates of planned or convert-to-open cholecystectomy were not significantly different between the SA and delayed cholecystectomy groups.
The cohort was stratified by the severity of acute cholecystitis based on the Tokyo grading system (Table 2). There were no differences in severity of disease between the SA and the delayed cholecystectomy groups.
Complication rates were significantly increased for SA compared to Delayed cholecystectomy for a diagnosis of acute cholecystitis (18.5%vs4.4%, respectively,P=0.004; Table 3). Although complications in mild (Grade 1) and severe (Grade 3) acute cholecystitis were not significant, patients with moderate disease (Grade 2)experienced significantly more complications during SA compared to the delayed group (16.1%vs0.0%,P< 0.001). When we compared the complication rate of patients undergoing a delayed cholecystectomy, we found that the postoperative complication rate was similar to the rate for elective cholecystectomy for chronic cholecystitis (4.4%vs6.2%,P= 0.557). As expected, the overall complication rate of acute cholecystitis(combining both SA and delayed) was significantly greater than that of an elective cholecystectomy (16.8%vs6.2%,P< 0.001).
Table 3 also shows the types of complications. A significantly increased rate of subtotal cholecystectomy was performed for the SA patients compared to delayed(7.6%vs0.0%,P= 0.016). Since a subtotal cholecystectomy was not the intended operation, we considered the performance of a subtotal cholecystectomy as a complication. Subtotal cholecystectomy, which is essentially a drainage procedure,was only performed in the SA group, suggesting that subtotal cholecystectomy is a surrogate for operative difficulty. A total of 37 patients underwent subtotal cholecystectomies; eight patients were Grade 1, 27 were Grade 2, and two patients were Grade 3. If we excluded subtotal cholecystectomies as a “true” complication, the complication rate was still statistically significant: 13.4%vs4.4% (SAvsdelayed,respectively,P= 0.03). Mortality rates among all patients were 0.6%vs0.0% for SA and delayed, respectively. All three patients who died had cholecystectomy within 24 h of admission from the emergency department. The first death occurred in a 90-yearold with Grade 3 disease. The second patient had Grade 1 disease and a history of congestive heart failure. The third had Grade 2 disease and unrecognized cardiac ischemia postoperatively. Notably, there were no common bile duct injuries in either group (Table 3). All other complication types identified were similar between the groups, including bile leak, retained stone, cholangitis, biliary stenosis, infection,hernia, and complications involving the cardiovascular, respiratory, or gastrointestinal systems.
The time between initial admission and operative intervention for the delayed cholecystectomy group was 48.3 ± 76.3 d (Table 4). Postoperative readmission rates were similar between the groups (22.2%vs21.2%,P= 0.854). In comparison to the delayed cases, the SA group had significantly longer total lengths of hospital stay (3.8± 5.5vs1.6 ± 2.0,P< 0.001).
SA cholecystectomy hospital charges were higher compared to Delayed intervention for acute cholecystitis ($44500 ± $59000vs$35300 ± $16700,P= 0.019,Table 4). Hospital charges for elective cholecystectomies performed on chronic conditions were the lowest at $23000 ± $10300 (P< 0.001, 1-way ANOVA comparing all three).
There were no differences in complication rates based on insurance status for SA(17.0% insuredvs14.1% uninsured,P= 0.127) or Delayed cholecystectomy (0.7%insuredvs0% uninsured,P= 1). As expected, the vast majority of delayed cholecystectomies (97.1%) were insured compared to a lower number for SA patients(71.2%;P< 0.001).
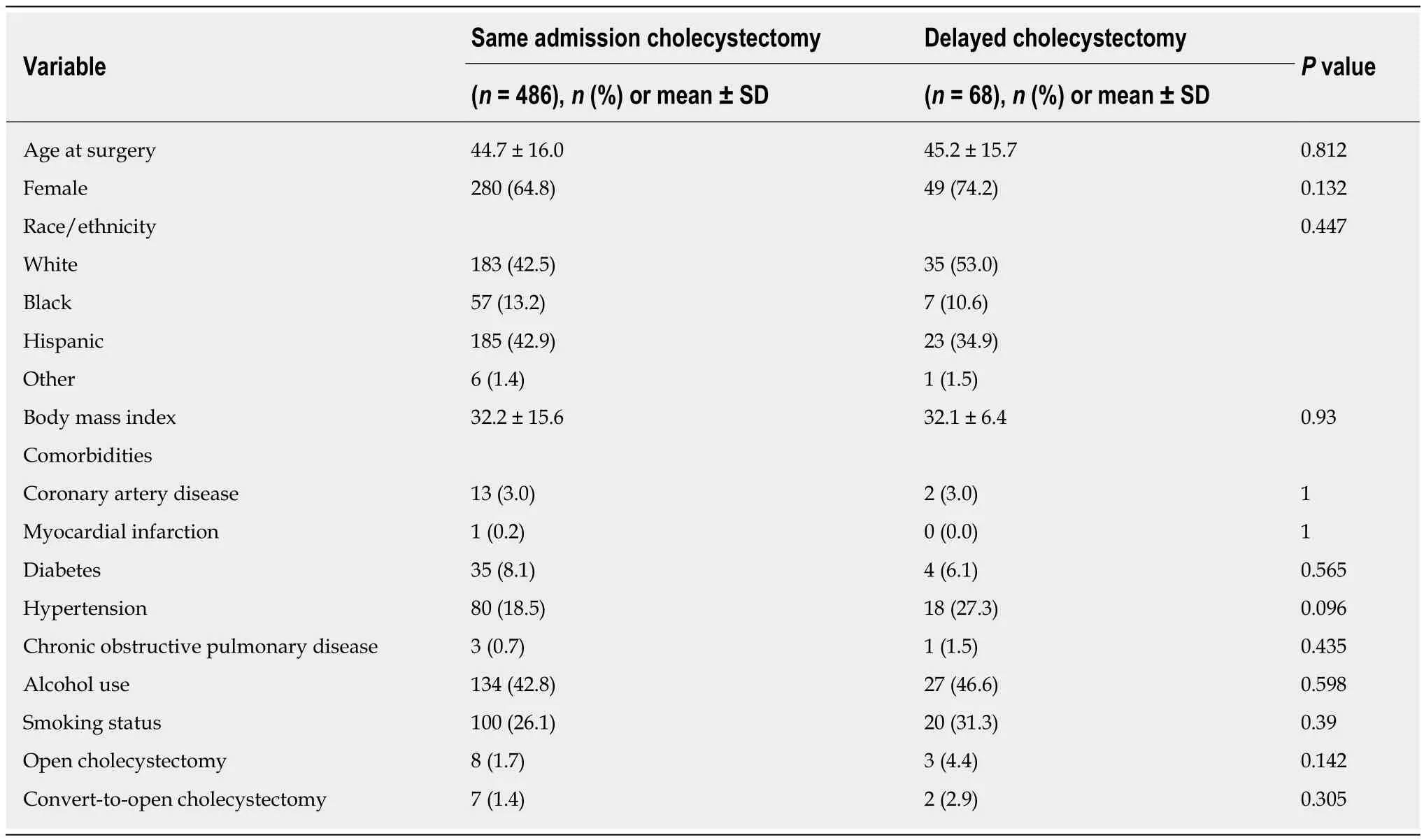
Table 1 Demographics and patient characteristics
A logistic regression analysis was performed to determine if there are any independent variables that can predict a higher risk of complications. We stratified disease severity by TG13/18 and found that complication rates were only significantly different with the Grade 2 subset (Table 5). The odds of any complication occurring was 2.1x greater in patients with Grade 2 disease compared to those with Grade 1(95%CI: 1.2-3.7,P= 0.007, Table 5). The odds of any complication occurring in Grade 2 or 3 was 2.3x greater in males compared to female patients (95%CI: 1.0-5.1,P= 0.047).
Risk analysis (Table 6) of developing a complication in the SAvsdelayed groups demonstrated a relative risk of 4.2x (95%CI: 1.4-12.9) and attributable risk of 14.1%(95%CI: 4.6-23.6). Number needed to harm (NNH) analysis indicated that, among eight patients (95%CI: 5.0-12.3) with acute cholecystitis undergoing SA cholecystectomy, one patient will suffer a complication. Notably, the attributable and NNH for Grades 2 or 3 patients were 28.3% (95%CI: 12.3-44.4) and 4 (95%CI: 2.9-4.6),respectively.
DISCUSSION
Historically, the timing of performing cholecystectomy for a diagnosis of acute cholecystitis has been very controversial. A Cochrane systematic review with metaanalysis of six randomized clinical trials (1998-2003) compared earlyvsdelayed laparoscopic cholecystectomy for patients with acute cholecystitis and concluded no significant difference between the groups with regards to immediate postoperative mortality, bile duct injuries, other serious adverse events, or rates of conversion to open cholecystectomy[14]. The only significant clinical outcome in favor of early cholecystectomy was a shorter hospital length of stay by four days. Multiple publications support early (SA) over delayed (interval) cholecystectomy based on equivalent morbidity and mortality, and an overall better economic profile[1-8,15-17].However, the data from our institution over the past 8.5 years show that for the subset of Grade 2 patients, there is greater risk of morbidity and mortality with SA cholecystectomy. When a complication does occur, we found a concomitant longer length of hospital stay with an associated increase in hospital costs. When Grade 2 patients undergo delayed cholecystectomy, the rate of complications decreases to thatof elective cholecystectomies for subacute diagnoses (e.g., biliary colic, gallbladders polyps). Due to the small sample size in Grade 3 patients, the logistic regression analysis (Table 5) did not identify Grade 3 patients at risk for greater complications and death when comparing operative timing. Although we cannot make definitive statements about Grade 3 patients in our study, multiple investigators with larger sample sizes do validate the highest morbidity and mortality for the highest grade of disease severity[12,18,19].
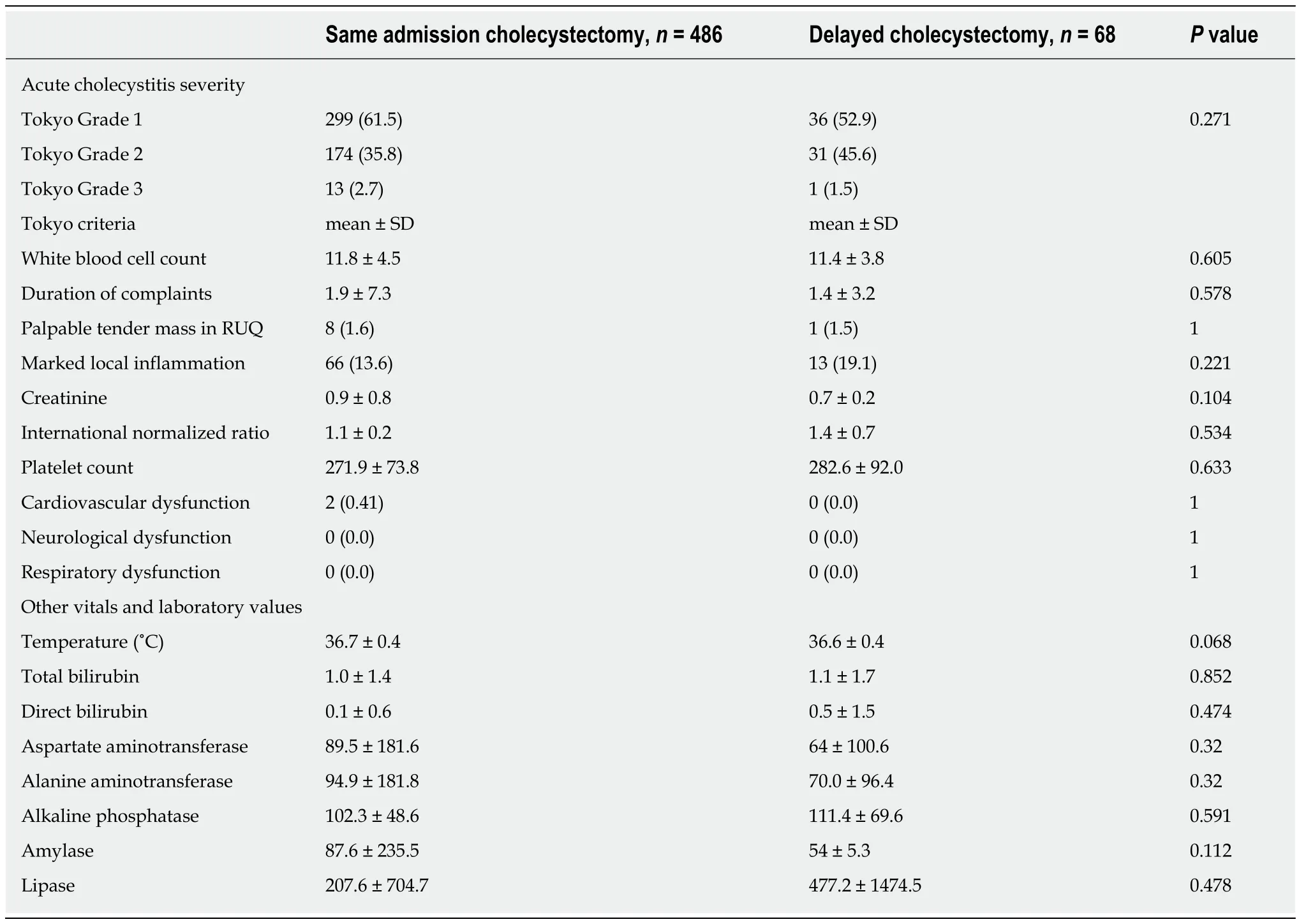
Table 2 Stratification by disease severity using 2013/18 Tokyo guidelines, n (%)
Hernandezet al[18]validated TG13 grading among a cohort of 443 patients at the Mayo Clinic in Rochester, MN. The odds of postoperative complications For TG grade 2 and 3 were 1.8 times and 4.9 times the risk compared to grade 1 patients. Their finding for Grade 2 patients is similar to our study where Grade 2 patients had an odds ratio of 2.1 for complications compared to Grade 1 patients. Chenget al[20]compared complication rates between 103 patients with acute cholecystitis of either Tokyo Grades 1, 2, or 3. Similar to our work, they noticed an increased surgical complication rate in Grade 2 (25.0%) compared to Grades 1 (5.6%) and 3 (0.0%). The low complication rate for Grade 3 patients in both Chen and our data are due to low sample size. Also in agreement with our findings, the literature has demonstrated an excess risk of complications in males undergoing cholecystectomy for acute cholecystitis[21-23]although the reason for the association between gender and complication risk with cholecystectomy remains unclear.
In our study, among the SA cholecystectomy patients, the mean time from admission to operation was 2.2 ± 14.2 d, with an overall mortality rate of 0.6%. In a recent population-based study the 30-d operative mortality for all cholecystectomies(elective and emergent) performed for gallstone disease was 0.15% (72 deaths out ofn= 47912 patients)[24]. They report that the risk of death for “acute” surgery compared with “planned” surgery was 10-fold higher (95%CI: 2.41-41.95). Patients with perioperative complications were 3.3-fold higher (95%CI: 1.74-6.15) for risk of death.Furthermore, patients between ages 50-70 and > 70 had a 2.12 (95%CI: 0.67-6.74) and a 7.04 (95%CI: 2.23-22.26) fold increase risk of death compared to patients < age 50,respectively. Among the three patients in our study who died postoperatively, twowere in their 5th decade of life and one patient was in the 9th decade of life.
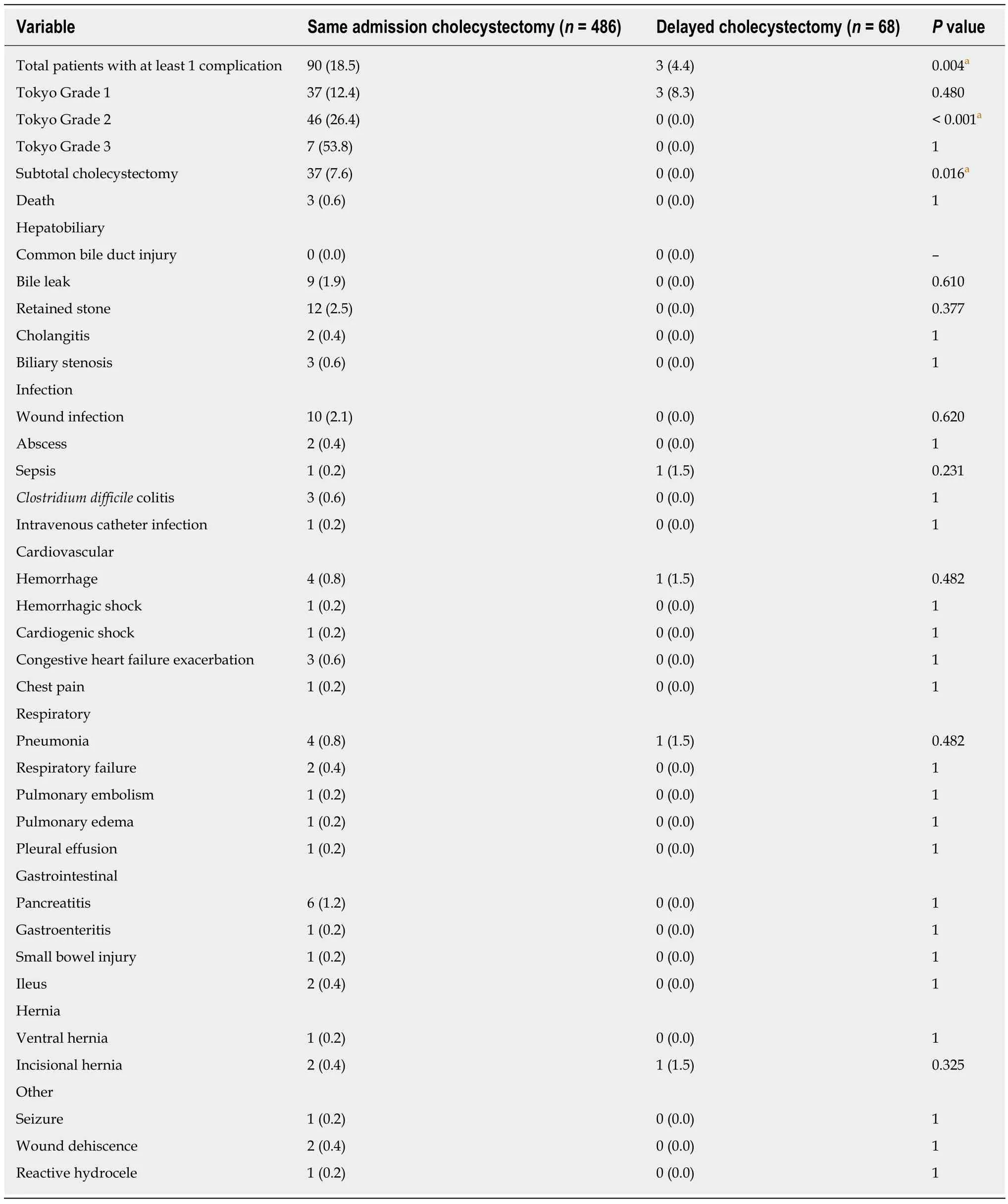
Table 3 Complication rates and types, n (%)
In a study by Zafaret al[25]using Nationwide Inpatient Sample data from 2005-2009,a multivariate analysis demonstrated that the odds of complications and death increased when cholecystectomy was performed between days 2-5 [mortality OR 1.26(95%CI: 1.00-1.58)] and 6-10 d [mortality OR = 1.93 (1.38-2.69)] after admission,compared to days 0-1 (OR = 1). Based on this large dataset of withn> 95500 patients,the authors determined that the optimal time to perform cholecystectomy was less than 48 h, and that if the timing exceeds 48 h, the delay would result in highermorbidity and mortality. Guttet al[16]found that cholecystectomy within 24 h (mean 0.6 d) of admission had the lowest morbidity compared to delayed cholecystectomy 7-45 d (mean 25 d) after presentation; mortality was equivalent with one death in each group (0.33%). However, Brookset al[26]did not find an association between the timing of SA operation (0 d, 1 d, 2 d, 3 d and ≥ 4 d from admission) with 30-d morbidity and mortality after risk adjustment when analyzing data from the American College of Surgeons National Surgical Quality Improvement Program database; this result may be due to a smaller sample size compared with Zafar's dataset. Although our cohort of patients generally underwent cholecystectomy close to the 48-h time-frame, it is noteworthy that all three deaths were operated on within 24 hours of admission. The mortality rates in Zafar's study were 0.2%, 0.6% and 1.7% for 0-1 d, 2-5 d and 6-10 d,respectively. Interestingly, while Zafaret al[25]advocate early cholecystectomy within 48 hours of admission, they note that the mortality rate for day 0 was higher at 0.42%;they hypothesized that some patients may be under-resuscitated at day 0 and therefore at higher risk for death.
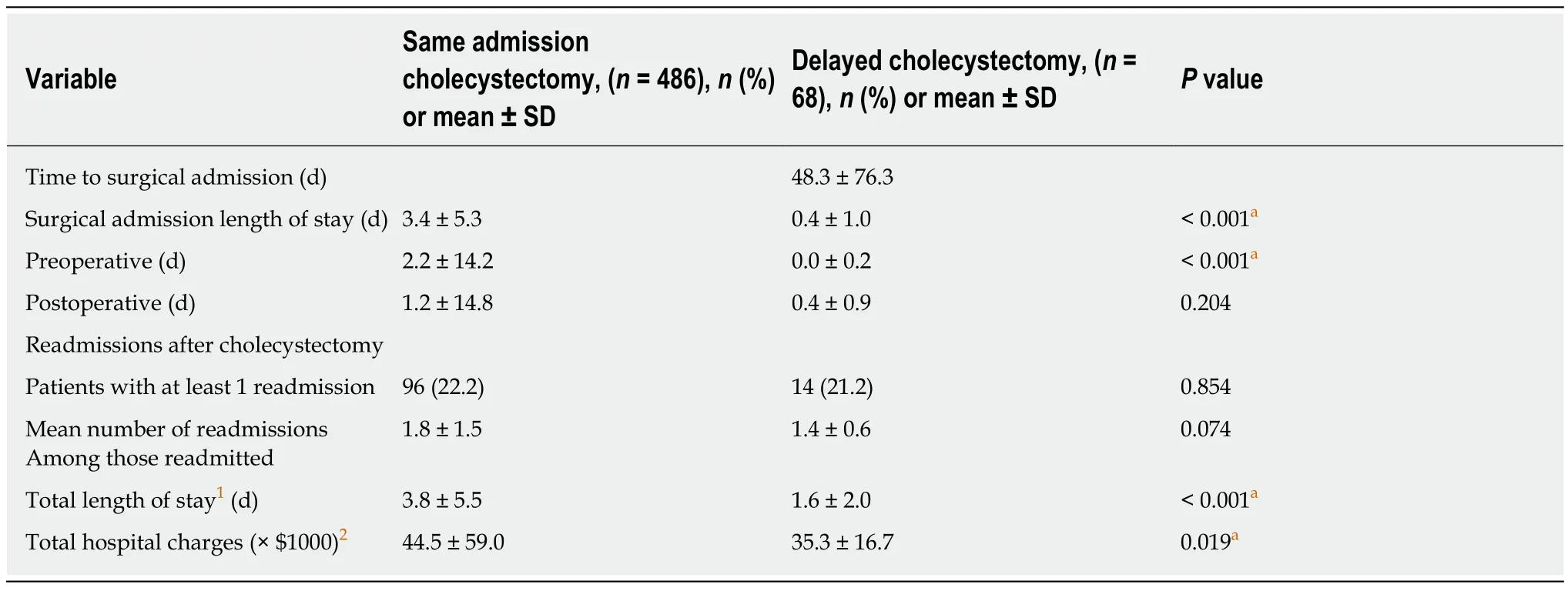
Table 4 Hospital length of stay, postoperative readmissions, and charges
In a large retrospective study from Japan and Taiwan, the 30-d mortality rate for among 2947 patients undergoing primary cholecystectomy for TG grades 1, 2, and 3 of acute cholecystitis were 0.3%, 0.4%, and 4.1%, respectively[19]. Josephet al[27]presented contemporary data (n= 857) from a single institution and noted no mortality in Tokyo Grade 1 patients, 8 (0.5%) deaths in Grade 2 patients and 6 (1.8%) deaths in Grade 3 patients. Their patient population is a heterogeneous mix, with only 51% who had an elevated WBC and 45% with no ultrasonographic signs of acute cholecystitis. They included a significant number of patients categorized as having “acute on chronic”disease, who do not meet the TG clinical criteria for acute cholecystitis. Although their thesis was that the Tokyo criteria were not sensitive for acute cholecystitis, the inclusion a significant number of patients with normal WBC implies that they had a larger denominator in their reported mortality rate. The mortality rate would be higher with a smaller denominator (if only patients who meet the TG criteria for acute cholecystitis were included). The increase in death rate among the SA group in our study was not statistically significant when compared to the delayed group due to our small sample size; however, postoperative death for a benign condition concerns us sufficiently to revisit the optimal timing of surgical intervention for acute cholecystitis.
To manage “difficult” gallbladders, the WSES recommends subtotal cholecystectomy especially in the acute setting or a delayed cholecystectomy 45 d from symptom onset. We defined a delayed cholecystectomy for acute cholecystitis as a procedure occurring after discharge electively after stabilization of acute disease.However, the literature does not have an agreed upon definition of a “delayed”cholecystectomy and ranges from 1 d to 6 wk after symptom onset, diagnosis, or index presentation. On average, patients in this study received a delayed, elective cholecystectomy 48.3 d from index presentation of acute disease. Our work supports the 2016 WSES recommendations for subtotal cholecystectomies and delayed time frame[1].
A limitation of this study is the retrospective nature of our data; there is selectionbias especially for Grade 3 patients, where the small sample size precluded definitive conclusions. Since we did not include preoperative percutaneous cholecystostomy tubes, we likely excluded a significant number of Grade 3 patients from this study.Additionally, hospital charge data for the SA and delayed represent 78.4% and 69.1%of the total patients, respectively. Financial comparisons were made on the majority of patients, but would be more reliable if we could obtain all of the data. Finally, this study represents the experience at one academic, teaching institution with 26 faculty members performing the cholecystectomies. The faculty members are board-certified general surgeons with competency for laparoscopic and open cholecystectomy; only a few self-identify as having specific hepatobiliary or advanced laparoscopic expertise.We have a general surgery training program and all surgeons and surgical residents on these cases have earned Fundamentals of Laparoscopic Surgery-certification. The applicability of this study may not be generalizable in all practice settings.
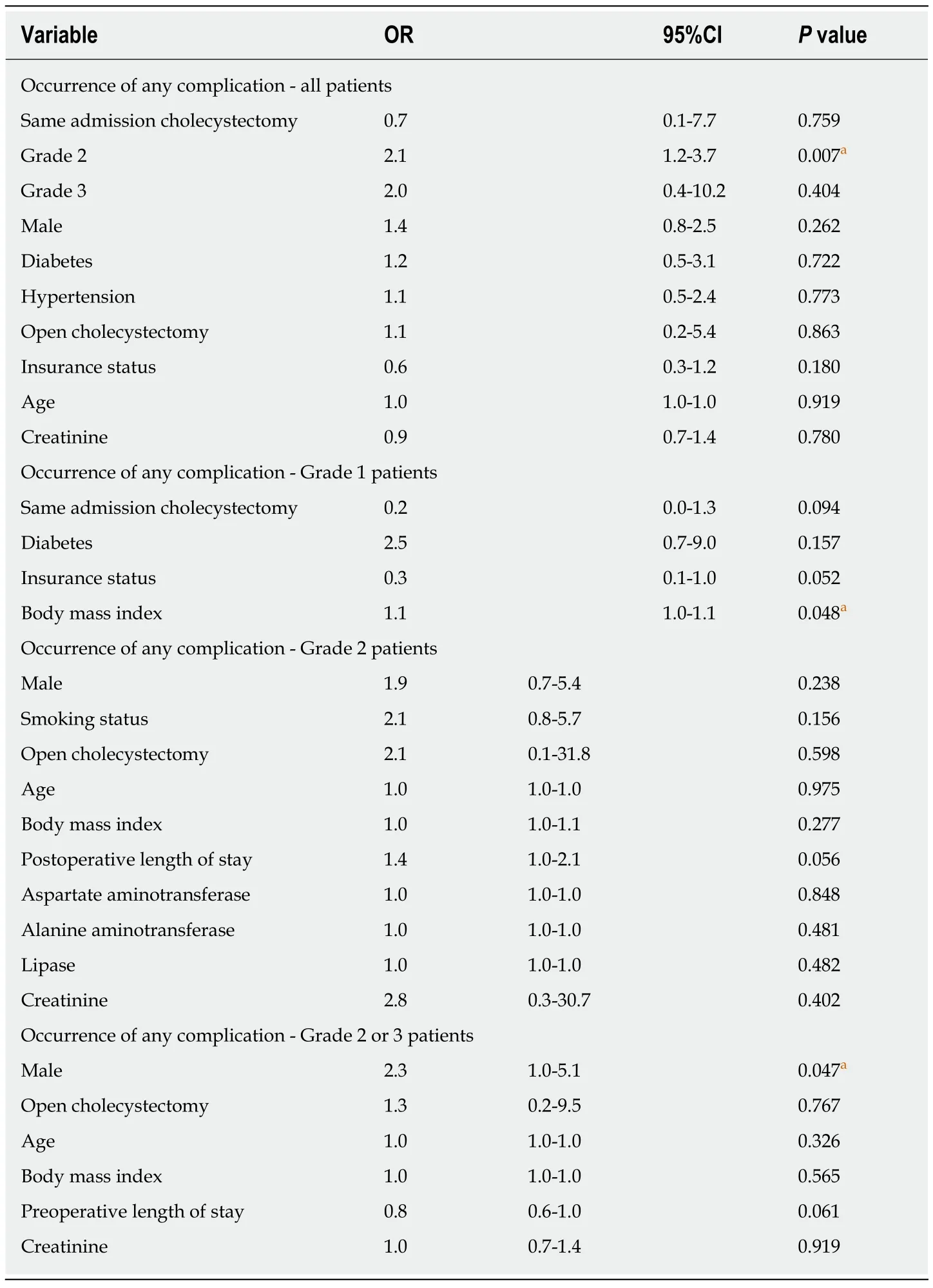
Table 5 Logistic regression analysis
Our work supports the 2018 TG for the management of Grades 1 and 2 acute cholecystitis[10]. Specifically, if a patient has significant co-morbidities and/or is a high-risk surgical candidate, conservative management with antibiotics, fluid resuscitation, and pain control should be followed by elective cholecystectomy. If thepatient does not improve clinically with conservative management, percutaneous cholecystotomy can be performed to drain the septic source. In this study, we have compared the clinical and economic outcomes of SA cholecystectomy with delayed cholecystectomy for acute cholecystitis. Early cholecystectomy for Tokyo Grades 2 and 3 patients should be considered with care. The risks of complications are higher in these patient groups, leading to greater cost. Future studies are needed to confirm our findings and also should focus on strategies to avoid mortality in these high-risk groups.
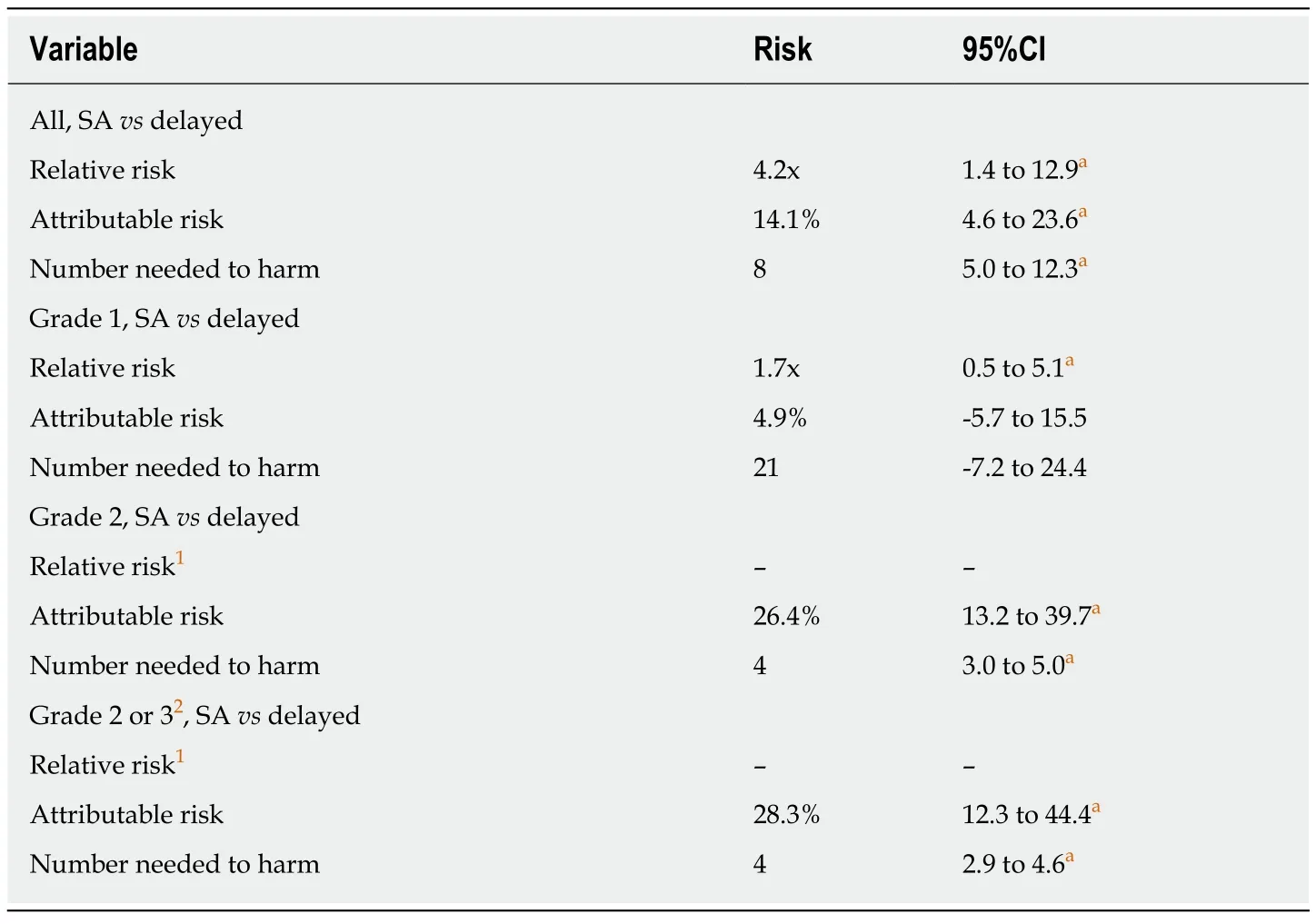
Table 6 Relative risk, attributable risk, and number needed to harm analysis
In conclusion, patients presenting with acute cholecystitis Tokyo Grade 2 developed more complications and incur increased charges when undergoing SA cholecystectomy compared to a delayed approach. This data supports a selective approach to surgery for patients with acute cholecystitis; Tokyo Grade 2 patients have a lower complication rate when cholecystectomy is delayed.
ARTICLE HIGHLIGHTS
Research results
SA cholecystectomy patients had an overall complication rate of 18.5% compared to Delayed cholecystectomy patients with a complication rate of 4.4% (P= 0.004). For the Tokyo Grade 2 patients (moderate disease), SA and delayed cholecystectomy complication rates were 16%vs0%, respectively (P< 0.001). SA cholecystectomy hospital charges were higher compared to Delayed cholecystectomy (P= 0.019) due to an increase in cost from the management of complications. There were no significant differences in clinical outcomes for Tokyo Grade 1 patients (mild disease). We did not have sufficient numbers of patients with Tokyo Grade 3(severe disease) for meaningful comparisons.
Research conclusions
Our study demonstrates that SA cholecystectomy patients have higher complication rates with associated higher costs. The data supports a selective approach to operative intervention for acute cholecystitis; Tokyo Grade 2 patients have a lower complication rate when cholecystectomy is Delayed. Risk factors for complications include Tokyo Grade 2 severity of disease. In a risk analysis, among eight patients with acute cholecystitis undergoing SA cholecystectomy, one patient will suffer a complication.
Research perspectives
This study suggests that SA cholecystectomy does not always afford an economic advantage,especially if there are complications. Future studies are needed to confirm our findings since this study is limited because the data was collected retrospectively from a single institution.
ACKNOWLEDGEMENTS
We thank Eileen Figueroa for her assistance with manuscript preparation, and Chad Allen and Winston Chan for their assistance with data acquisition. This paper was presented, in part, at the Surgical Forum in San Francisco on October 30, 2019, and at the 77thAnnual Meeting of the AAST/4thWorld Trauma Congress in San Diego on September 27, 2018.
杂志排行
World Journal of Gastroenterology的其它文章
- Wrap choice during fundoplication
- Pulmonary tumor thrombotic microangiopathy of hepatocellular carcinoma: A case report and review of literature
- Significance of postoperative follow-up of patients with metastatic colorectal cancer using circulating tumor DNA
- Hepatitis C virus eradication with directly acting antivirals improves health-related quality of life and psychological symptoms
- Diagnostic and prognostic value of lncRNA cancer susceptibility candidate 9 in hepatocellular carcinoma
- Comprehensive multi-omics analysis identified core molecular processes in esophageal cancer and revealed GNGT2 as a potential prognostic marker
