长疗程应用尼可地尔对原发性稳定型微血管心绞痛临床疗效及冠脉血流的影响
2019-02-11马麟邓鑫
马麟 邓鑫

[摘要]目的 探討长疗程应用尼可地尔对原发性稳定型微血管心绞痛临床疗效及冠脉血流的影响。方法 选取2015年12月~2018年1月锦州医科大学附属第一医院、沈阳二四二医院、沈阳维康医院收治的178例原发性稳定型微血管心绞痛患者作为研究对象(剔除20例),根据随机数字表法分为观察组(75例)与对照组(83例)。两组患者均给予高危因素控制、抗血小板聚集、抗动脉硬化、控制心率、抑制交感神经等治疗。观察组患者加用注射用尼可地尔,6 mg/h,泵注,疗程为6 h,继之口服尼可地尔10 mg,3次/d,疗程为1年。观察两组患者每个月心绞痛发作次数、每次心绞痛持续时间、每个月硝酸甘油总剂量,比较两组患者ST段下移的最大值、ST段出现下移改变的起始时间、心绞痛发作起始时间、运动总时间及校正的TIMI帧数(CTFC)、TIMI心肌灌注帧数(TMPFC)。结果 两组患者治疗前每个月心绞痛发作次数、每次心绞痛持续时间、每个月硝酸甘油总剂量比较,差异无统计学意义(P>0.05);两组患者治疗后每个月心绞痛的发作次数少于治疗前,每次心绞痛持续时间短于治疗前,每个月硝酸甘油总剂量低于治疗前,差异均有统计学意义(P<0.05);观察组患者治疗后每个月心绞痛发作次数少于对照组,每次心绞痛持续时间短于对照组,每个月硝酸甘油总剂量低于对照组,差异均有统计学意义(P<0.05)。两组患者治疗前ST段出现下移改变的起始时间、心绞痛发作起始时间、运动总时间比较,差异无统计学意义(P>0.05);两组患者治疗后ST段出现下移改变的起始时间、心绞痛发作起始时间、运动总时间均长于治疗前,差异有统计学意义(P<0.05);观察组患者治疗后ST段出现下移改变的起始时间、心绞痛发作起始时间、运动总时间均长于对照组,差异有统计学意义(P<0.05)。两组患者治疗前的CTFC、TMPFC比较,差异无统计学意义(P>0.05);两组患者治疗后的CTFC、TMPFC少于治疗前,差异均有统计学意义(P<0.05);观察组患者治疗后的CTFC、TMPFC均少于对照组,差异有统计学意义(P<0.05)。两组患者治疗后均未发生严重的不良反应。结论 长疗程应用尼可地尔治疗原发性稳定型微血管心绞痛安全有效,并且可以改善冠脉血流。
[关键词]长疗程;尼可地尔;原发性稳定型微血管心绞痛;临床疗效;冠脉血流
[中图分类号] R285.5 [文献标识码] A [文章编号] 1674-4721(2019)12(c)-0008-04
Effect of long-term application of Nicorandil on the clinical efficacy and coronary blood flow of primary stable microangiocardia
MA Lin1 DENG Xin2
1. Department of Cardiology, Shenbei New District Central Hospital of Shenyang City, Liaoning Province, Shenyang 110000, China; 2. Department of Neurology, Shengjing Geriatrics Hospital of Liaoning Province, Shenyang 110000, China
[Abstract] Objective To investigate the effect of long-term application of Nicorandil on the clinical efficacy and coronary blood flow of primary stable microangiocardia. Methods A total of 158 patients with primary stable microvascular angina pectoris admitted to the First Affiliated Hospital of Jinzhou Medical University, Shenyang 242 Hospital and Shenyang Weikang Hospital from December 2015 to January 2018 were selected as the subjects (20 cases excluded). According to the random number table method, the patients were divided into the observation group (75 cases) and the control group (83 cases). Both groups were given high-risk factor control, anti-platelet aggregation, anti-arteriosclerosis, control of heart rate, inhibition of sympathetic nerve and other treatments. The patients in the observation group were treated with Nicorandil for injection (6 mg/h) and pump injection for 6 h, followed by 10 mg of oral administration of Nicorandil three times a day for 1 year. The number of angina pectoris attacks per month, duration of each angina pectoris and total dose of Nitroglycerin per month were observed in the two groups. The start time of ST segment down shift change, the start time of angina pectoris attack, the total time of exercise, the corrected TIMI frame number (CTFC) and TIMI myocardial perfusion frame number (TMPFC) were compared between the two groups. Results There was no significant difference between the two groups in the number of angina attacks per month, duration of each angina pectoris and total dose of nitroglycerin per month before treatment (P>0.05). After treatment, the number of angina attacks per month in the two groups was fewer than that before treatment, the duration of each angina pectoris was shorter than that before treatment, and the total dose of Nitroglycerin per month was lower than that before treatment, the differences were statistically significant (P<0.05). After treatment, the number of angina attacks per month in the observation group was fewer than that in the control group, the duration of each angina pectoris was shorter than that in the control group, and the total dose of Nitroglycerin per month was lower than that in the control group, the differences were statistically significant (P<0.05). There was no significant difference in the start time of ST segment down shift change, the start time of angina pectoris attack, the total time of exercise between the two groups before treatment (P>0.05). The the start time of ST segment down shift change, the start time of angina pectoris attack, the total time of exercise were longer than those before treatment, the differences were statistically significant (P<0.05). The the start time of ST segment down shift change, the start time of angina pectoris attack, the total time of exercise were longer than those in the control group, the differences were statistically significant (P<0.05). There was no significant difference in CTFC and TMPFC between the two groups before treatment (P>0.05). The CTFC and TMPFC in the two groups after treatment were lessr than those before treatment, the differences were statistically significant (P<0.05). After treatment, the CTFC and TMPFC in the observation group were less than those in the control group, and the differences were statistically significant (P<0.05). No serious adverse reactions occurred in both groups after treatment. Conclusion The long-term application of Nicorandil in the treatment of primary stable microvascular angina pectoris is safe and effective, which can improve coronary blood flow.
[Key words] Long course of treatment; Nicorandil; Primary stable microvascular angina pectoris; Clinical efficacy; Coronary blood flow
对于冠脉微血管疾病的研究,有着近40年的历史,1967年Lidoff首先报道了该类疾病特点[1],该病的命名先后经历了“X综合征”“微血管性心绞痛”[1-2]。2010年Lanza等[3]为了和继发于特定的某些微血管型心绞痛相区别,将其修正为原发性微血管心绞痛,并分为稳定型和不稳定型微血管心绞痛。2013年ESC将其列为冠心病的临床类型[4];2017年3月中华医学会心血管病学分会颁布了我国首部《冠状动脉微血管疾病诊断和治疗的中国专家共识》[5]。但该领域循证证据仍不充分,提出的诊疗建议也是初步的。既往研究证实,短期内静脉或冠脉内应用尼可地尔,可改善患者的慢血流、无复流,保护心肌[6],减少再灌注损伤[7],改善急性心力衰竭患者的症状和血流动力学[8]。然而目前长期应用尼可地尔对原发性稳定型微血管心绞痛的相关研究报道较少,本研究选取178例原发性稳定型微血管心绞痛患者作为研究对象,旨在探讨长疗程应用尼可地尔对原发性稳定型微血管心绞痛临床疗效及冠脉血流的影响,现报道如下。
1资料与方法
1.1一般资料
选取2015年12月~2018年1月锦州医科大学附属一院、沈阳二四二医院、沈阳维康医院收治的178例原发性稳定型微血管心绞痛患者作为研究对象,根据随机数字表法分为观察组(89例)与对照组(89例)。观察组中,男24例,女65例;年龄45~65岁,平均(51.0±6.5)岁;体重指数(BMI)(28.4±5.4)kg/m2;吸烟20例,高血压10例,糖尿病12例,高脂血症14例;剔除14例。对照组中,男22例,女67例;年龄44~67岁,平均(50.0±7.2)岁;BMI(29.1±6.2)kg/m2;吸烟18例,高血压11例,糖尿病10例,高脂血症13例;剔除6例。两组患者的一般资料比较,差异无统计学意义(P>0.05),具有可比性。本研究已经医院医学伦理委员会批准,患者均签署知情同意书。
纳入标准:①患者年龄18~75岁;②患者符合原发性稳定型微血管心绞痛的诊断[5]。排除标准:①心功能Ⅲ~Ⅳ级者;②妊娠或哺乳妇女;③肝肾功能异常者;④变异性心绞痛者;⑤其他心脏疾病引起的心源性胸痛者;⑥非心源性胸痛者。剔除标准:①未按规定用药累积2周者;②未按规定复诊或随访者。
1.2方法
对照组患者给予高危因素控制;阿司匹林(拜耳医药保健有限公司,生产批号:BJ30875)100 mg,1次/d,抗血小板聚集;阿托伐他汀钙片(辉瑞制药有限公司,生产批号:W52364)20 mg,1次/d,抗动脉硬化;琥珀酸美托洛尔缓释片(阿斯利康制药有限公司,生产批号:UDUM)47.5 mg,1次/d,控制心率及抑制交感神经,疗程为1年。
观察组患者在对照组的基础上给予注射用尼可地尔(北京四环科宝制药有限公司,生产批号:15100945)6 mg/h,泵注,疗程为6 h,继之口服尼可地尔(西安汉丰药业有限责任公司,生产批号:1506091)10 mg,3次/d,疗程为1年。
两组患者治疗前后均行心电图(ECG)、运动负荷试验(采用修正的Bruce运动平板方案)、冠脉造影(CAG)、肝肾功能、血尿便常规、凝血四项检查。其中冠脉血流评价指标由相同2名具有10年介入经验的医生独立阅片,取平均值。
1.3观察指标
1.3.1临床疗效评价指标 每个月通过微信或电话随访的方式随访,记录每个月心绞痛发作次数、每次心绞痛持续时间、每个月使用的硝酸甘油总剂量。
1.3.2运动负荷试验指标 ST段出现下移改變的起始时间、心绞痛发作起始时间、运动总时间。
1.3.3冠脉血流评价指标 校正的TIMI帧数(CTFC)[9]、TIMI心肌灌注帧数(TMPFC)[10]。
1.3.4安全性评价指标 血压、心率、血尿便常规、肝功能、肾功能、凝血四项。
1.4统计学方法
采用SPSS 22.0统计学软件对数据进行分析,计量资料以均数±标准差(x±s)表示,采用t检验,计数资料以率(%)表示,采用χ2检验,以P<0.05为差异有统计学意义
2结果
2.1两组患者治疗前后临床疗效指标的比较
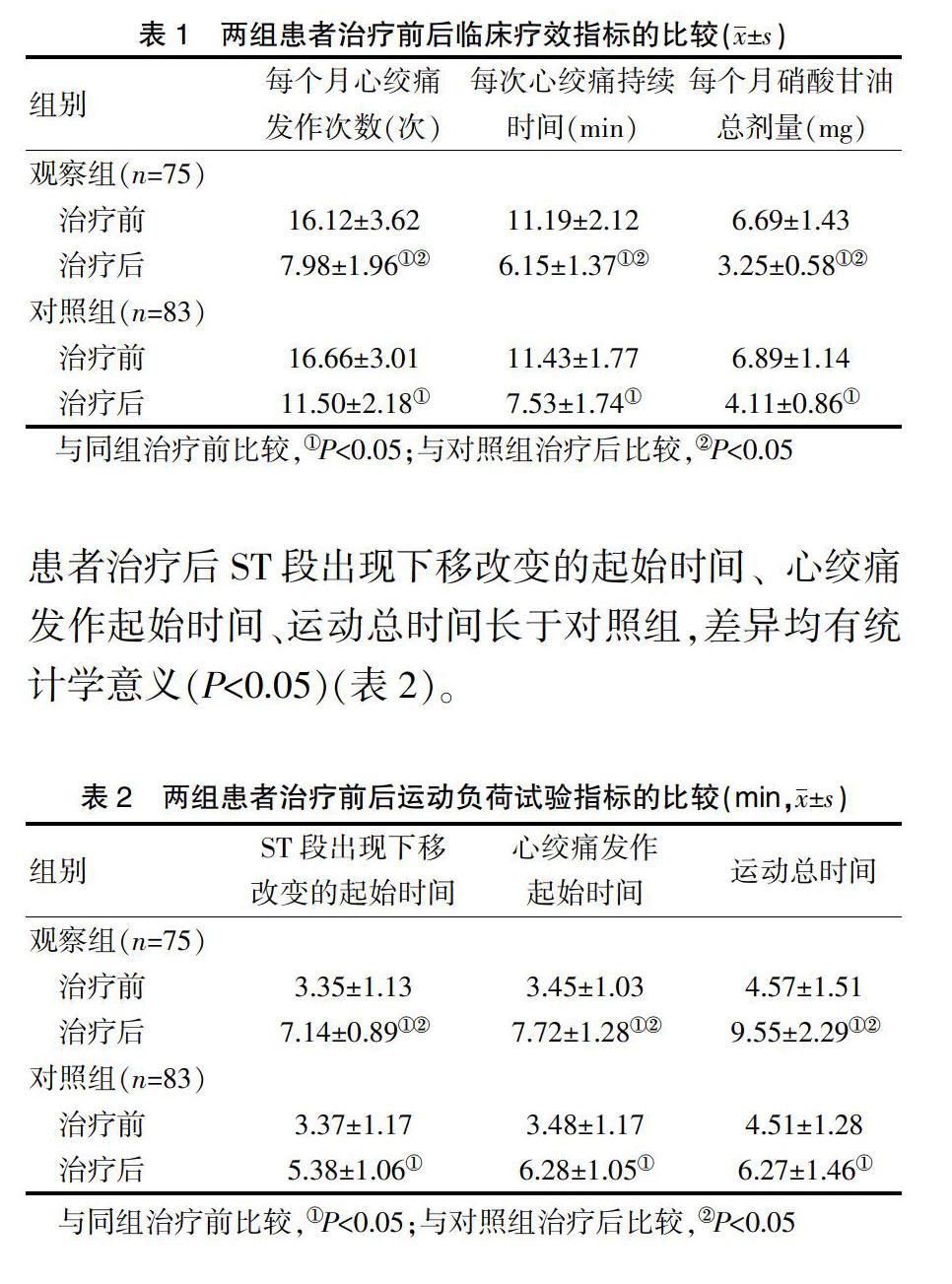
两组患者治疗前每个月心绞痛发作次数、每次心绞痛持续时间、每个月硝酸甘油总剂量比较,差异无统计学意义(P>0.05);两组患者治疗后每个月心绞痛的发作次数少于治疗前,每次心绞痛持续时间短于治疗前,每个月硝酸甘油总剂量低于治疗前,差异均有统计学意义(P<0.05);观察组患者治疗后每个月心绞痛发作次数少于对照组,每次心绞痛持续时间短于对照组,每个月硝酸甘油总剂量低于对照组,差异有统计学意义(P<0.05)(表1)。
2.2两组患者治疗前后运动负荷试验指标的比较
两组患者治疗前ST段出现下移改变的起始时间、心绞痛发作起始时间、运动总时间比较,差异无统计学意义(P>0.05);两组患者治疗后ST段出现下移改变的起始时间、心绞痛发作起始时间、运动总时间长于治疗前,差异均有统计学意义(P<0.05);观察组患者治疗后ST段出现下移改变的起始时间、心绞痛发作起始时间、运动总时间长于对照组,差异均有统计学意义(P<0.05)(表2)。
2.3两组患者治疗前后冠脉血流指标的比较
两组患者治疗前的CTFC、TMPFC比较,差异无统计学意义(P>0.05);两组患者治疗后的CTFC、TMPFC少于治疗前,差异均有统计学意义(P<0.05);观察组患者治疗后的CTFC、TMPFC少于对照组,差异均有统计学意义(P<0.05)(表3)。
2.4两组患者的不良反应发生情况
两组患者治疗后均未发生严重的不良反应。
3讨论
尼可地尔是一种钾离子通道开放剂,本研究结果显示,观察组患者治疗后每个月心绞痛发作次数少于对照组,每次心绞痛持续时间短于对照组,每个月硝酸甘油总剂量低于对照组,差异均有统计学意义(P<0.05),提示长疗程应用尼可地尔可减少原发性稳定型微血管心绞痛患者每个月心绞痛发作的次数、每次心绞痛持续时间及每个月硝酸甘油的使用总剂量。本研究结果还显示,观察组患者治疗后ST段出现下移改变的起始时间、心绞痛发作起始时间、运动总时间均长于对照组,CTFC、TMPFC均少于对照组,差异有统计学意义(P<0.05),提示长疗程应用尼可地尔可延迟ST段出现下移改变的起始时间及心绞痛的发作时间,增加运动总时间,可减少CTFC、TMPFC帧数,加快冠脉血流流速。究其原因,可能有如下几个方面。
现认为原发性稳定型微血管心绞痛的发病机制可能与冠脉微血管内皮损伤、冠脉的微血管功能异常、心脏自主神经功能紊乱、雌激素水平减低、钙离子超载、血管痉挛、栓塞等有关[11]。其中多种动脉粥样硬化危险因素通过血管内皮细胞依赖性和非依赖性机制导致微血管功能异常、冠状动脉微血管阻力增高引起冠脉血流应答障碍,出现无法用心外膜冠状动脉缺血解释的心肌灌注不足或冠脉内慢血流而发生心绞痛症状[12-13]。
尼可地尔是首个应用于临床的ATP敏感性钾通道开放剂[14],其主要由烟酰胺基本骨架和硝酸基团构成[15],具有类硝酸酯作用[16]。其可通过以下3种途径扩张外周及冠脉血管,减轻心脏压力负荷,减少心肌耗氧量,解除冠脉痉挛,加快冠脉血流流速,改善微血管功能,减低冠状动脉微血管阻力,达到减少心绞痛发作次數、缩短心绞痛每次发作时间、提高运动负荷试验的耐受量、改善冠脉血流的作用。一是通过开放血管平滑肌细胞膜的K+-ATP通道,ATP敏感性升高,对K+的通透性升高,K+外流使细胞膜超极化,关闭T型电压依赖型钙离子通道,减少Ca2+内流,抑制血管平滑肌的收缩[16];二是通过K+-ATP型通道的调节,降低微血管阻力,从而改善微循环障碍[17];三是通过依赖和不依赖NO途径激活鸟苷酸环化酶,激活钙离子泵,将Ca2+排出细胞外,降低Ca2+浓度[16],同时可降低收缩蛋白对Ca2+的敏感性[18]。
综上所述,长疗程应用尼可地尔治疗原发性稳定型微血管心绞痛安全有效,且可改善冠脉血流,值得推广应用。
[参考文献]
[1]Melikian N,Broyne BD,Fearon WF,et al.The pathophysiology and clinical course ofthe normal coronary angina syndrome(cardiac syndrome x)[J].Prog Cardiovasc Dis,2008,50(4):294-310.
[2]Cannon RO 3rd.Microvascular angina and the continuing dilemma of chest pain with normal coronary angiograms[J].J Am Coll Cardiol,2009,54(10):877-885.
[3]Lanza GA,Crea F.Primary coronary mierovascular dysfunction:clinical presentation pathophysiology and management[J].Circulation,2010,121:2317-2325.
[4]Task Force Members,Montalescot G,Sechtem U,et al.2013 ESC guidelines on the management of stable coronary artery disease:the task force on the management of stable coronary artery disease of the European society of cardiology[J].Eur Heart J,2013,34:2949-3003.
[5]中华医学会心血管病学分会基础研究学组,中华医学会心血管病学分会介入心脏病学组,中华医学会心血管病学分会女性心脏健康学组,等.冠状动脉微血管疾病诊断和治疗的中国专家共识[J].中国循环杂志,2017,32(5):421-430.
[6]Iwakura K,Ito H,Okamura A,et al.Nicorandil treatment in patients with acute myocardial infarction:a meta-analysis[J].Circ J,2009,73(5):925-931.
[7]冯力,邱健,马骏,等.缺血-再灌注不同时间点给予尼可地尔对犬心肌梗死范围的影响[J].中国危重病急救医学,2005,17(3):157-160.
[8]Harada K,Yamamoto T,Okumura T,et al.Intravenous nicorandil for treatment of the urgent phase acute heart failure syndromes:a randomized,controlled trial[J].Eur Heart J Acute Cardiovasc Care,2017,6(4):329-338.
[9]Ge H,Ding S,An D,et al.Frame counting improves the assessment of post reperfusion microvascular patency by TIMI myocardial perfusion grade:evidence from cardiac magnetic resonance imaging[J].Int J Cardiol,2016,203:360-366.
[10]Sestito A,Lanza GA,Di Monaco A,et al.Relation between cardiovascular risk factors and coronary microvascular dysfunction in cardiac syndrome X[J].J Cardiovasc Med (Hagerstown),2011,12:322-327.
[11]李一凡.微血管性心绞痛发病机制的研究进展[J].心血管病学进展,2014,35(5):291-294.
[12]Kamlesh K,Bairay Meiz CN.Mierovascular coronary dysfunction in women pathophysiology,diagnosis,and management[J].Curr Probl Cardiol,2011,36(8):291-318.
[13]Zimarino M,Affinito V.The prognosis of periprocedural myocardial infarction after percutaneous coronary interven-tions[J].Cardiovasc Revasc Med,2013,14(1):32-36.
[14]吴杰华.尼可地尔在冠心病治疗中的临床应用进展[J].中西医结合心血管病电子杂志,2018,6(15):17-18.
[15]李江.尼可地尔治疗冠心病心绞痛的疗效观察[J].中国医学创新,2012,9(22):43-44.
[16]Kostic J,Djordjevic-Dikic A,Dobric M,et al.The effects of nicorandil on microvascular function in patients with ST segment elevation myocardial infarction undergoing primary PCI[J].Cardiovasc Ultrasound,2015,13:26.
[17]Iwaki F,Amano H,Ohura K.Nicorandil inhibits osteoclast differentiation in vitro[J].Eur J Pharmacol,2016,793:14-20.
[18]Li W,Wu N,Shu W,et al.Pharmacological preconditioning and postconditioning with nicorandil attenuates ischemia/reperfusion-induced myocardial necrosis and apoptosis in hypercholesterolemic rats[J].Exp Ther Med,2015,10(6):2197-2205.
(收稿日期:2019-10-23 本文編辑:闫 佩)
