Differential hepatic features presenting in Wilson disease-associated cirrhosis and hepatitis B-associated cirrhosis
2019-01-29HaoJieZhongHuanHuanSunLanFengXueEileenMcGowanYuChen
Hao-Jie Zhong, Huan-Huan Sun, Lan-Feng Xue, Eileen M McGowan, Yu Chen
Abstract BACKGROUND Cirrhosis is a chronic late stage liver disease associated with hepatitis viruses,alcoholism, and metabolic disorders, such as Wilson disease (WD). There are no clear markers or clinical features that define cirrhosis originating from these disparate origins. We hypothesized that cirrhosis is not one disease and cirrhosis of different etiology may have differential clinical hepatic features.AIM To delineate the liver features between WD-associated cirrhosis and hepatitis B-associated cirrhosis in the Chinese population.METHODS In this observational study, we reviewed the medical data of consecutive inpatients who had WD-associated cirrhosis or hepatitis B-associated cirrhosis from January 2010 to August 2018, and excluded patients who had carcinoma,severe heart or pulmonary diseases, or other liver diseases. According to the etiology of cirrhosis, patients were divided into two groups: WD-associated cirrhosis group (60 patients) and hepatitis B-associated cirrhosis group (56 patients). The liver fibrosis degree, liver function indices, and portal hypertension features of these patients were compared between the two groups.RESULTS No inter-group differences were observed in the diagnostic liver fibrosis markers,however, clinical features clearly defined the origin of cirrhosis. WD-associated cirrhosis patients (16-29 years) had lower levels of alanine transaminase,aspartate transaminase, and bilirubin, lower prothrombin time, lower incidence of hepatic encephalopathy, and lower portal vein diameter (P < 0.05), compared to cirrhosis resulting from hepatitis B in older patients (45-62 years). Importantly,they had decreased risks of progression from Child-Pugh grade A to B (odds ratio = 0.046, 95% confidence interval: 0.006-0.387, P = 0.005) and of ascites (odds ratio = 0.08, 95% confidence interval: 0.01-0.48, P = 0.005). Conversely, WD-associated cirrhosis patients had a higher risk of splenomegaly (odds ratio = 4.15,95% confidence interval: 1.38-12.45, P = 0.011).CONCLUSION WD-associated cirrhosis presents a higher risk of splenomegaly associated with leukopenia and thrombocytopenia, although revealing milder liver dysfunction and portal hypertension symptoms, which recommends WD patients to be monitored for associated complications.
Key words: Chronic hepatitis B; Cirrhosis; Hepatic feature; Liver function; Portal hypertension; Wilson disease
INTRODUCTION
Wilson disease (WD), also named hepatolenticular degeneration, is an autosomal recessive disease of copper metabolism caused by mutations in ATP7B, which encodes a copper transporting ATPase[1,2]. Dysfunction of this ATPase causes copper overload in the liver, brain, and other organs. Depending on the organs affected, WD has a wide spectrum of clinical symptoms, including hepatic, neurological, psychiatric, and ophthalmological manifestations[2]. As the liver is the primary organ for copper metabolism and has the highest expression level of copper transporting ATPase,hepatic changes are usually the earliest and most frequent manifestations in WD patients[2-4]. Although the prevalence of symptomatic WD is low worldwide (about 1/30000), the frequency of this disease is much higher in the Chinese population(about 5.87/100000)[2,5]. Cirrhosis is a common manifestation in WD patients compared to inpatients with other types of liver diseases[6,7].
Cirrhosis is the 11thmost common cause of death globally, accounting for 3.5% of all-cause mortalities[8]. Therefore, it is important to understand the clinical features of cirrhosis for prevention and treatment of these manifestations and complications. A meta-analysis that investigated data from 12 studies estimated that the prevalence of cirrhosis was 34% in WD patients[9]. Clinical symptoms of WD, especially hepatic manifestations, often present in the first decade of life, and most occur between the ages of 5-35[10]. As a result, WD frequently causes cirrhosis in children and young adults[9]. In some areas of Iran and India, WD was found to be the primary cause of cirrhosis in children[11,12]. Generally, cirrhosis is characterized by portal hypertension and hepatic dysfunction, leading to esophageal varices, splenomegaly, ascites, and liver injury[13]. However, cirrhosis caused by WD in children and young adults differs from non-alcoholic fatty liver disease and chronic hepatitis B. As the etiology and onset age of WD-associated cirrhosis are different from those of other kinds of liver cirrhosis, WD-associated cirrhosis may involve a different liver injury pathogenesis.Unfortunately, the hepatic features of cirrhosis in WD patients are less well reported.
Hepatitis B virus (HBV) infection, as the most common chronic viral infection, is the main cause of cirrhosis worldwide[6,13]. Globally, nearly 257 million people are living with HBV, and one third of them live in China[14,15]. About 10%-20% of Chinese patients with chronic hepatitis progress to cirrhosis within 5 years[16], making HBV the leading cause of cirrhosis in the Chinese population[17]. Therefore, we performed this study to delineate the liver features between WD-associated cirrhosis and hepatitis B-associated cirrhosis in the Chinese population.
MATERIALS AND METHODS
Study populations
In this observational study, we retrospectively reviewed the medical data of consecutive inpatients who were diagnosed with cirrhosis caused by either WD or HBV presenting from January 2010 to August 2018 at the First Affiliated Hospital of Guangdong Pharmaceutical University. The patients were excluded from the study if they met any of the following criteria: (1) Carcinoma; (2) severe heart or pulmonary diseases; (3) fatty liver disease, alcoholic liver disease, autoimmune liver disease,drug-induced liver injury, or hepatic parasitic infection; and (4) incomplete medical data. Patients who were hospitalized more than once were recorded only once. This study was performed with the approval of the Ethical Committee of the First Affiliated Hospital of Guangdong Pharmaceutical University. All patients in the study were de-identified.
Data collection
The following medical data were extracted from the subjects' electronic medical records: demographic characteristics, history of smoking and alcohol drinking,medical history (diabetes, hypertension, and liver disease), disease duration,manifestations of cirrhosis, imaging examinations, and laboratory test results including alanine transaminase (ALT), aspartate transaminase (AST), serum albumin(ALB), bilirubin, prothrombin time (PT), total cholesterol (TC), triglyceride, lowdensity lipoprotein (LDL), high-density lipoprotein, white blood cell (WBC) count,red blood cell (RBC) count, platelet count, procollagen type III N-terminal propeptide(PIIINP), type IV collagen, laminin, and hyaluronic acid.
In addition, disease duration was calculated based on the onset age of WD or HBV infection. Child-Pugh classification was assessed as previously described[18].Leukopenia was defined as a WBC count < 4.0 × 109/L. Erythropenia was defined as an RBC count < 4.0 × 1012/L for males or 3.5 × 1012/L for females. Thrombocytopenia was defined as a platelet count < 100 × 109/L. The indication for splenectomy was hypersplenism, characterized by splenomegaly, leukopenia, erythropenia, and thrombocytopenia[19]. Smokers were defined as patients who have smoked at some stages in their lifetime. Alcohol consumption was defined when patients drank more than 140g of alcohol per week.
In China, diagnosis of WD is based on the classic criteria: Age of onset; family history; low serum ceruloplasmin (< 200 mg/L); elevated urinary copper excretion (≥100 μg/24 h); elevated liver copper (> 250 μg/g dry weight); and elevated urinary copper excretion after challenge with 2 × 500 mg D-penicillamine (> 1600 μg/24 h)[20].Chronic hepatitis B was diagnosed based on the clinical manifestations and serological and virological examinations[21].
Statistical analysis
The statistical analyses were performed using IBM SPSS statistics software, version 22(IBM Corp., Armonk, NY, United States). Normally distributed continuous variables are presented as the mean ± standard deviation. Non-normally distributed continuous variables are presented as medians and interquartile ranges. Categorical variables are presented as frequencies and proportions. The statistical significance of the difference in means between the two groups was tested using the unpaired t-test. The statistical significance of the difference in medians between the two groups was tested using the Mann-Whitney U-test. Categorical variables were tested using the Chi-square test or Fisher's exact test. To assess the association between cirrhosis etiology and portal vein diameter, and the association between cirrhosis etiology and liver fibrosis markers,multivariable linear regression analysis with a forward stepwise approach was used to adjust for confounders. To assess whether the risk of ascites, splenomegaly, and progression from Child-Pugh grade A to B or C differed between WD-associated cirrhosis patients and hepatitis B-associated cirrhosis patients, logistic regression analysis with a backward stepwise approach was used. Odds ratios (ORs) and 95%confidence intervals (CIs) were estimated. A P-value < 0.05 (two-tailed) was considered statistically significant.
RESULTS
Demographics and clinical characteristics
Based on the medical data, 56 inpatients with hepatitis B-associated cirrhosis and 60 with WD-associated cirrhosis were enrolled. The mean age and age range of these patients recorded in Table 1 clearly demonstrate that WD-associated cirrhosis was more prevalent in the younger age group, whereas, in general, hepatitis B occurred in older adults. The percentage of males, disease duration, LDL level, and prevalence of diabetes, hypertension, alcohol drinking, and smoking were significantly higher in hepatitis B-associated cirrhosis patients than in WD-associated cirrhosis patients(Table 1). In patients with hepatitis B-associated cirrhosis, 48.21% (27/56) were undergoing treatment with antiviral agents, and 47.06% (24/51) presented with low HBV DNA (≤ 2000 IU/mL).
Relationship between cirrhotic etiology and liver fibrosis markers
The levels of PIIINP, type IV collagen, and hyaluronic acid were lower in WD-associated cirrhosis patients than in hepatitis B-associated cirrhosis patients.However, the level of laminin was higher in WD-associated cirrhosis patients (Table 2). Despite presenting with distinct clinical variations, after adjustment for age,gender, disease duration, diabetes, hypertension, alcohol drinking, and smoking, the multivariable linear regression analysis showed no overt differences in any of the four liver fibrosis markers between the two groups of patients.
Relationship between cirrhotic etiology and liver function indices
The PT and the levels of ALT, AST, and bilirubin, but not the level of ALB, were lower in WD-associated cirrhosis patients compared with hepatitis B-associated cirrhosis patients. Additionally, the incidence of hepatic encephalopathy was lower in WD-associated cirrhosis patients. An important observation showed that the percentage of patients with Child-Pugh grades B and C was lower in WD-associated cirrhosis patients compared with hepatitis B-associated cirrhosis patients (Table 3). Logistic regression analysis showed that patients with WD-associated cirrhosis had a significantly decreased risk of progression from Child-Pugh A to B (OR = 0.046, 95%CI: 0.006-0.387, P = 0.005), and a non-significant decreased risk for progression to Child-Pugh C (OR = 0.164, 95% CI: 0.013-2.063, P = 0.162; Table 4), after adjustment for age, gender, disease duration, diabetes, hypertension, alcohol drinking, and smoking, as compared to patients with hepatitis B-associated cirrhosis.
Relationship between cirrhotic etiology and features of portal hypertension
Table 5 shows that the portal vein diameter and incidence of ascites were lower in WD-associated cirrhosis patients than in hepatitis B-associated cirrhosis. However,WD-associated cirrhosis patients had a statistical trend toward a higher incidence of splenomegaly (88.33% vs 75.00%, P = 0.062). Multivariable linear regression analysis showed that WD-associated cirrhosis was associated with a lower portal vein diameter. Moreover, after adjustment for age, gender, disease duration, diabetes,hypertension, alcohol drinking, smoking, and Child-Pugh classification, the logistic regression analysis showed that WD-associated cirrhosis patients had a significantly decreased risk of ascites compared with hepatitis B-associated cirrhosis patients (OR =0.08, 95%CI: 0.01-0.48, P = 0.005). However, the logistic regression analysis showed that WD-associated cirrhosis patients had a significantly increased risk of splenomegaly compared with hepatitis B-associated cirrhosis patients (OR = 4.15,95%CI: 1.38-12.45, P = 0.011).
Splenomegaly for hematocytopenia
Logistic regression analysis showed that splenomegaly was associated with a significantly increased risk of leukopenia (OR = 4.41, 95%CI: 1.29-15.12, P = 0.018) and thrombocytopenia (OR = 23.08, 95%CI: 2.86-186.11, P = 0.003; Table 6), but noterythropenia. Eight patients with WD-associated cirrhosis and seven with hepatitis B-associated cirrhosis had undergone splenectomy. After splenectomy, 50.00% (4/8) of WD-associated cirrhosis patients and 28.57% (2/7) of hepatitis B-associated cirrhosis patients had a normal WBC count; 62.50% (5/8) and 28.57% (2/7) had a normal platelet count.
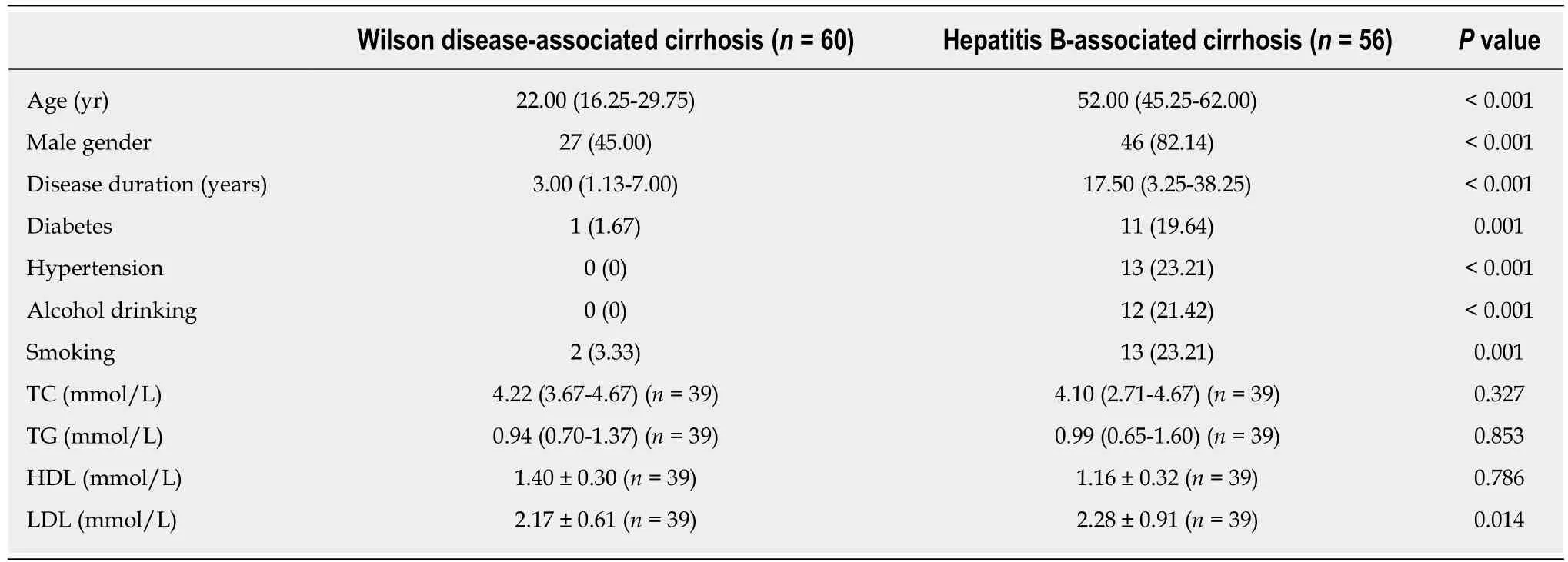
Table 1 Characteristics of patients with cirrhosis
DISCUSSION
Liver disease is the most common clinical manifestation of WD, and cirrhosis is frequently presented in these patients[4]. WD is not a common disease, and its pathogenesis and early onset of age are quite different from those of other liver diseases[2]. The clinical manifestations of WD are diverse[4], and the clinical features of cirrhosis caused by WD are still unclear. To the best of our knowledge, this is the first study to analyze the liver features of WD-associated cirrhosis and present clear distinct features to distinguish WD-associated cirrhosis from hepatitis B-associated cirrhosis.
In this observational study, compared with patients with hepatitis B-associated cirrhosis, WD-associated cirrhosis presented in a younger age group, and patients developed milder liver dysfunction and portal hypertension manifestations.Consistent with our finding, a recent study involving 1357 WD patients showed that 39.5% of children and adolescents had cirrhosis at diagnosis[22]. As shown in a previous study, the prognosis of WD patients was excellent if the disease was treated appropriately[10]. Nonetheless, patients with WD-associated cirrhosis had a higher risk of splenomegaly, which was found to be a risk factor for leukopenia and thrombocytopenia. In contrast, due to long periods of immune tolerant phases and inactive residual phases, liver injury is more likely to occur at more advanced age in patients with HBV infection[23]. Thus, most patients with HBV infection who progress to cirrhosis do so after the age of 35 years[23].
The degree of liver fibrosis can be reflected by the levels of serum type III collagen,type IV collagen, laminin, and hyaluronic acid, which are components of the extracellular matrix during fibrosis[24,25]. Based on the multivariable linear regression analysis, no significant difference in any of these four markers was found between the two groups of patients. The results showed that the degree of liver fibrosis might be similar between WD-associated cirrhosis and hepatitis B-associated cirrhosis patients.However, these markers do not reflect liver fibrosis directly, and liver biopsy remains the gold standard method for fibrosis assessment. Thus, new diagnostic markers may be needed to assess liver damage and prognosis, and discern WD-associated cirrhosis and hepatitis B-associated cirrhosis treatments.
The liver performs many biochemical functions, such as the synthesis of protein and clotting factors and the metabolism of bilirubin and ammonia[26]. Thus, liver dysfunction, as a feature of cirrhosis, was assessed based on liver injury, synthesis function, metabolism function, and hepatic functional reserve. Compared with WD-associated cirrhosis patients, more severe liver injury was found in hepatitis B-associated cirrhosis patients, based on higher levels of ALT and AST. Moreover, thelower ALB level and longer PT in hepatitis B-associated cirrhosis patients indicated a more serious impairment of synthesis function. It is well known that hepatic encephalopathy, associated with hyperammonemia, is caused by impairment of ammonia detoxification in the liver[27]. Thus, a higher incidence of hepatic encephalopathy and a higher level of bilirubin indicated a more severe impairment of metabolism function in hepatitis B-associated cirrhosis patients. Additionally, the Child-Pugh classification system, a comprehensive index, has been the most widely used model to evaluate liver functional reserve[28]. Our results showed that hepatitis B-associated cirrhosis was a risk factor for progressing from Child-Pugh grade A to B,which indicated that hepatitis B-associated cirrhosis could lead to a more serious impairment of liver functional reserve. Therefore, compared with WD-associated cirrhosis, hepatitis B-associated cirrhosis seemed to cause a more serious impairment of liver function.
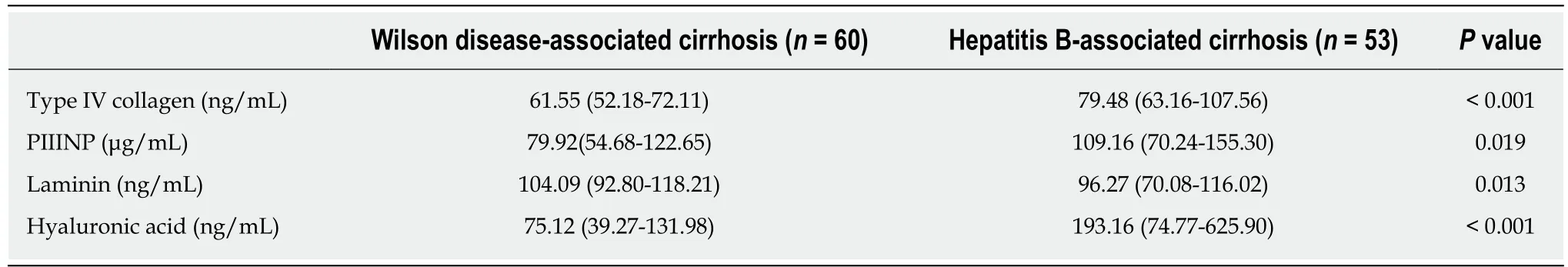
Table 2 Relationship between cirrhotic etiology and liver fibrosis markers
Portal hypertension, as another feature of cirrhosis, was assessed based on the portal vein diameter, ascites, and splenomegaly[29,30]. We found that the portal vein diameter was higher in hepatitis B-associated cirrhosis patients than in WD-associated cirrhosis patients. However, a previous study involving 167 healthy children from 1 mo to 15 years old showed that portal vein diameter was correlated with age and height, which means that the wider portal vein diameter in hepatitis B-associated cirrhosis patients might also result from their more advanced age[31]. Thus, a more precise method, such as hepatic venous pressure gradient measurement, was needed to evaluate the portal vein pressure between the two groups of patients[32]. Hepatitis B-associated cirrhosis patients had a higher risk of ascites, which might result from the more serious portal hypertension and lower level of ALB caused by liver dysfunction[33].
Splenomegaly is the most common imaging finding of portal hypertension[30]. A previous study involving 910 cirrhosis patients showed that 50.5% of the patients presented with splenomegaly[34]. Interestingly, the present study showed that the incidence of splenomegaly (88.3%) was not only much higher than the incidence in the previous study, but also much higher than the incidence in hepatitis B-associated cirrhosis patients (75%). In WD, splenomegaly seems to occur frequently, and it can even be the earliest clinical manifestation, particularly in children[10]. Consistent with our finding, previous research estimated that the incidence of splenomegaly is 49.0%(25/51) in WD patients[35], which is higher than that in chronic hepatitis B patients(41.7%; 65/156)[36]. After adjustment for potential confounders, there was a 3.15-fold increased risk of splenomegaly in WD-associated cirrhosis patients compared to hepatitis B-associated cirrhosis patients. There are three possible explanations for these results. First, non-autoimmune hemolytic anemia, which can lead to splenomegaly, has been shown to be common and an onset symptom in 10%-15% of WD patients[37]. Second, high concentration of serum copper might also have toxic effects on the spleen. Third, with increasing age, the size and function of the spleen are easily affected[38], and the younger age among WD-associated cirrhosis patients might also lead to a higher sensitivity of the spleen to all kinds of stimulation.
Additionally, portal hypertension could bring about hypersplenism, which is characterized by splenomegaly and pancytopenia due to excessive portal flow[39]. In this study, we found that splenomegaly was associated with increased risks of leukopenia and thrombocytopenia. As risk factors for certain fatal infections and bleeding (such as spontaneous bacterial peritonitis, urinary tract infection,pneumonia, and esophageal variceal bleeding), leukopenia and thrombocytopenia in WD-associated cirrhosis patients should receive more attention[40]. Regarding hypersplenism treatment, a clinical study in China revealed that splenectomy was a safe and effective therapeutic method for hypersplenism in WD patients, and it demonstrated obvious improvements in WBC and platelet counts in all the patients after splenectomy[19]. Similarly, in our study, most of the WD-associated cirrhosis patients with hypersplenism had normal WBC and platelet counts after splenectomy.
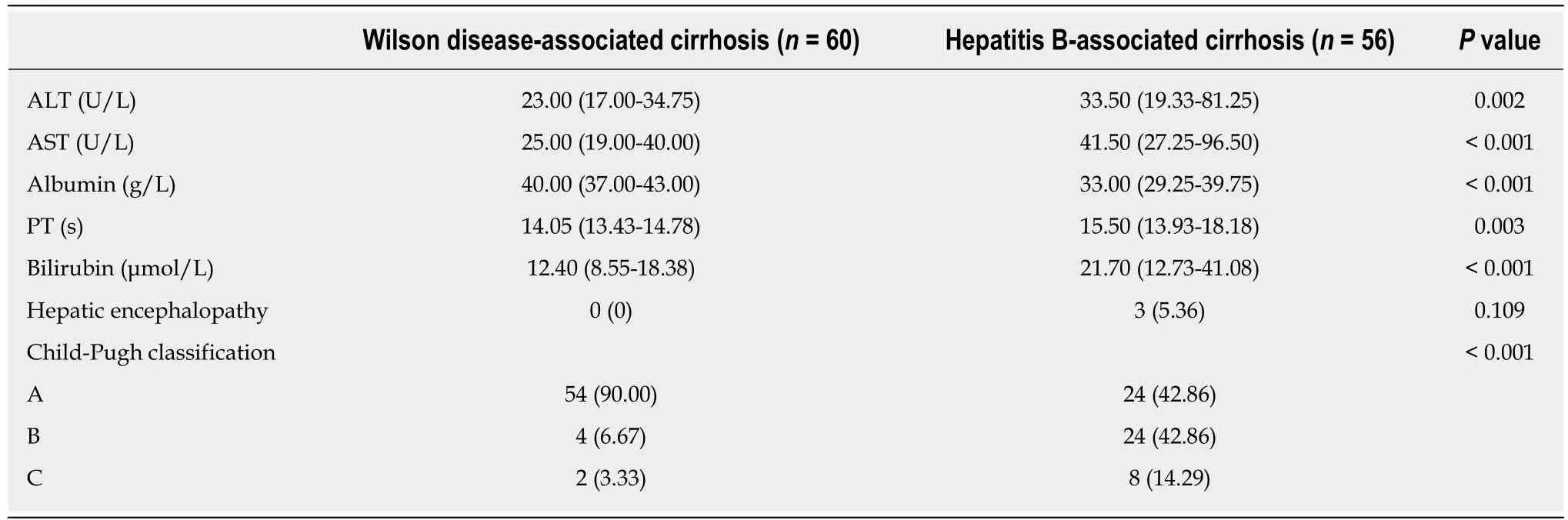
Table 3 Relationship between cirrhotic etiology and liver function indices
The present study had several limitations. First, as gastroscopy was not performed regularly in the cirrhosis patients, esophageal varices, a typical feature of portal hypertension, could not be compared between the two groups of patients. Second,due to the low economic status of some of the patients and the poor medical services in some areas of China, the patients often received a delayed diagnosis, which might have biased the disease duration assessment. Third, some confounders (such as medication use and duration from onset to diagnosis of disease), which might have had an influence on the results, were not taken into consideration. Finally, the study was a single-center study with a limited sample size. Thus, the results regarding the comparison of hepatic features between WD-associated cirrhosis patients and hepatitis B-associated cirrhosis patients should be interpreted with caution, and largescale, multi-center studies are needed to confirm these conclusions.
In conclusion, in this study, we provide evidence to show that cirrhosis is not one disease and there is a need for further classification for treatment options. Depending on the origin, cirrhosis presents different clinical features. Our findings, in concurrence with other studies in the literature, show that clinical features occur earlier in WD patients than in chronic hepatitis B patients. An important observation made in this study is that progression from Child-Pugh grade A to B or C differed between WD-associated cirrhosis patients and hepatitis B-associated cirrhosis patients. Notably, WD-associated cirrhosis patients had a higher risk of splenomegaly,which was found to be a risk factor for leukopenia and thrombocytopenia. Based on these findings, it is highly recommended that young Wilson's disease patients require regular monitoring for blood disorders and infections to alleviate further clinical complications. Additionally, splenectomy might be an effective therapy for hypersplenism in WD-associated cirrhosis patients.
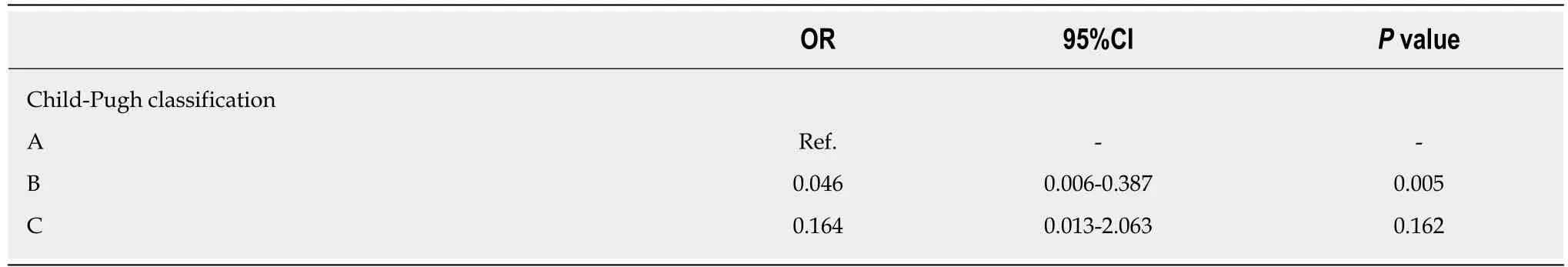
Table 4 Logistic regression analysis of Child-Pugh classification in patients with Wilson disease-associated cirrhosis vs patients with hepatitis B-associated cirrhosis
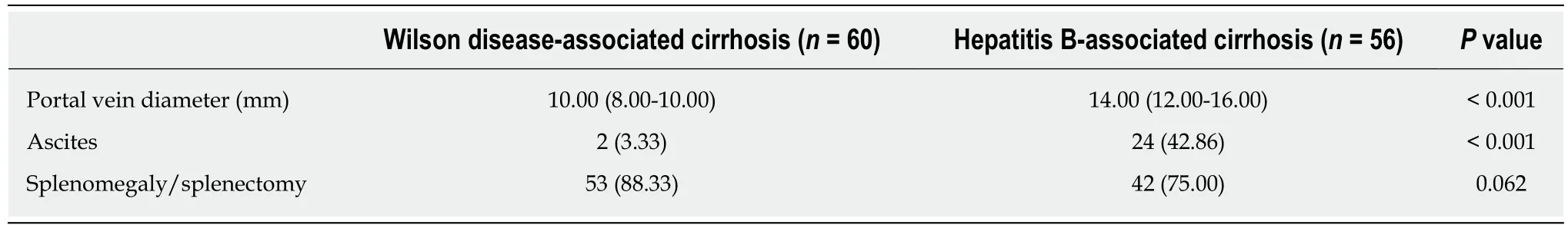
Table 5 Relationship between cirrhotic etiology and features of portal hypertension
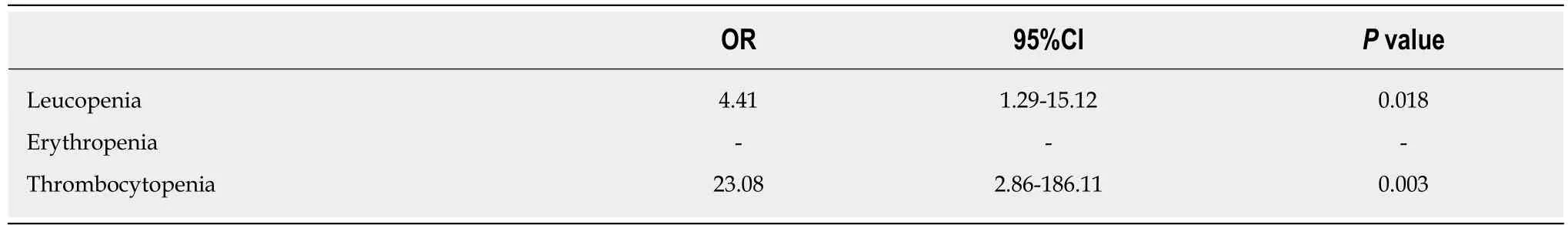
Table 6 Logistic regression analysis of risk of hematocytopenia due to splenomegaly
ARTICLE HIGHLIGHTS
Research background
Cirrhosis is a chronic late stage liver disease associated with hepatitis viruses, alcoholism, and metabolic disorders, such as Wilson disease (WD). As the etiology and onset age of WD-associated cirrhosis are different from those of other kinds of liver cirrhosis, WD-associated cirrhosis may involve a distinct liver injury pathogenesis.
Research motivation
We hypothesized that cirrhosis is not one disease and cirrhosis of different etiology may have differential clinical hepatic features.
Research objectives
To delineate the liver features between WD-associated cirrhosis and hepatitis B-associated cirrhosis in the Chinese population.
Research methods
We performed a cross-sectional study of 60 WD-associated cirrhosis and 56 hepatitis B-associated cirrhosis inpatients. We analyzed the liver fibrosis degree, liver function indices, and portal hypertension features between these two groups.
Research results
No inter-group differences were observed in the diagnostic liver fibrosis markers, however,clinical features clearly defined the origin of cirrhosis. Cirrhosis presenting in WD patients had worse liver function, lower incidence of hepatic encephalopathy, and lower portal vein diameter,compared to cirrhosis resulting from hepatitis B. They had decreased risks of progression from Child-Pugh grade A to B and of ascites. Conversely, WD-associated cirrhosis patients had a higher risk of splenomegaly, which was associated with a significantly increased risk of leukopenia and thrombocytopenia.
Research conclusions
WD-associated cirrhosis presents a higher risk of splenomegaly associated with leukopenia and thrombocytopenia, although revealing milder liver dysfunction and portal hypertension symptoms. These findings indicated that cirrhosis is not one disease and further classification for diagnosis and treatment options, dependent on origin, are needed.
Research perspectives
The higher risk of splenomegaly associated with leucopenia and thrombocytopenia in these younger, vulnerable WD patients with cirrhosis, suggests early and regular monitoring of associated blood disorders and infections to alleviate further clinical complications.
杂志排行
World Journal of Gastroenterology的其它文章
- Chronic hepatitis B and metabolic risk factors: A call for rigorous longitudinal studies
- Roles of Na+/Ca2+ exchanger 1 in digestive system physiology and pathophysiology
- Endoscopic resection techniques for colorectal neoplasia: Current developments
- Elastography-based screening for esophageal varices in patients with advanced chronic liver disease
- NKX6.3 protects against gastric mucosal atrophy by downregulating β-amyloid production
- Effects of positive acceleration (+Gz stress) on liver enzymes,energy metabolism, and liver histology in rats
