Novel abdominal negative pressure lavage-drainage system for anastomotic leakage after R0 resection for gastric cancer
2019-01-29ZhiFangZhengJunLuPengYangZhangBinBinXuChaoHuiZhengPingLiJianWeiXieJiaBinWangJianXianLinQiYueChenChangMingHuang
Zhi-Fang Zheng, Jun Lu, Peng-Yang Zhang, Bin-Bin Xu, Chao-Hui Zheng, Ping Li, Jian-Wei Xie, Jia-Bin Wang,Jian-Xian Lin, Qi-Yue Chen, Chang-Ming Huang
Abstract BACKGROUND Anastomotic leakage (AL) is a severe complication associated with high morbidity and mortality after radical gastrectomy (RG) for gastric cancer (GC).We hypothesized that a novel abdominal negative pressure lavage-drainage system (ANPLDS) can effectively reduce the failure-to-rescue (FTR) and the risk of reoperation, and it is a feasible management for AL.AIM To report our institution's experience with a novel ANPLDS for AL after RG for GC.METHODS The study enrolled 4173 patients who underwent R0 resection for GC at our institution between June 2009 and December 2016. ANPLDS was routinely used for patients with AL after January 2014. Characterization of patients who underwent R0 resection was compared between different study periods. AL rates and postoperative outcome among patients with AL were compared before and after the ANPLDS therapy. We used multivariate analyses to evaluate clinicopathological and perioperative factors for associations with AL and FTR after AL.RESULTS AL occurred in 83 (83/4173, 2%) patients, leading to 7 deaths. The mean time of occurrence of AL was 5.6 days. The AL rate was similar before (2009-2013, period 1) and after (2014-2016, period 2) the implementation of the ANPLDS therapy(1.7% vs 2.3%, P = 0.121). Age and malnourishment were independently associated with AL. The FTR rate and abdominal bleeding rate after AL occurred were respectively 8.4% and 9.6% for the entire period; however, compared with period 1, this significantly decreased during period 2 (16.2% vs 2.2%, P = 0.041;18.9% vs 2.2%, P = 0.020, respectively). Moreover, the reoperation rate was also reduced in period 2, although this result was not statistically significant (13.5% vs 2.2%, P = 0.084). Additionally, only ANPLDS therapy was an independent protective factor for FTR after AL (P = 0.04).CONCLUSION Our experience demonstrates that ANPLDS is a feasible management for AL after RG for GC.
Key words: Gastric cancer; Anastomotic leakage; Drainage; Lavage; Failure-to-rescue
INTRODUCTION
Improvements in surgical techniques and perioperative management have resulted in reduced postoperative mortality after radical gastrectomy (RG) for gastric cancer(GC). However, anastomotic leakage (AL) remains relatively common and represents a major cause of postoperative morbidity after RG for GC. The reported incidence of AL varies between 0% and 15.0%[1], and AL is associated with high mortality[2-4].
For several decades, routine prophylactic placement of abdominal drains has been the standard procedure in abdominal surgery. However, since the introduction of the enhanced recovery after surgery (ERAS) program, routine drain placement after gastrectomy is not warranted anymore, since drains do not reduce postoperative complications after gastrectomy and prolong hospital stay and postoperative recovery[5-7]. Despite these recommendations, prophylactic drainage of the abdominal cavity is still widely performed, because drains are believed to remove intraperitoneal fluids, which can be a source of infection, and drainage fluid might serve as an early warning sign of early complications like AL[7-10].
In January 2014, a novel abdominal negative pressure lavage-drainage system(ANPLDS) was routinely used for patients with AL at our institution. We found that ANPLDS can effectively reduce the failure-to-rescue (FTR) and abdominal bleeding rate after AL, and it is a feasible management for AL. Therefore, in this report, we present our utilization of and experiences with ANPLDS for AL after RG for GC.
MATERIALS AND METHODS
Study population
From a prospective database, clinical data of patients who underwent RG for primary gastric adenocarcinoma at Fujian Medical University Union Hospital (FMUUH)between June 2009 and December 2016 were identified. The case exclusion criteria eliminated the following from the study: distant metastasis, neoadjuvant chemotherapy, thoracoabdominal incision, and incomplete clinical and pathologic data. Finally, 4173 patients were included in this study. Laboratory blood test data were collected within 1 wk before surgery, including preoperative hemoglobin (HB)and albumin (ALB) levels. The type of surgical resection and the extent of lymph node dissection were selected according to the Japanese GC treatment guidelines[11]. The 8thedition of the American Joint Committee on Cancer (AJCC) Staging Manual was used to determine the disease stage[12]. This study was approved by the relevant institutional review board.
Management of AL
AL was defined as a complete intestinal wall defect at the anastomotic suture line that was confirmed via clinical findings, radiologic contrast medium assessment,abdominal computed tomography, a positive color test, or laparoscopic examination[13,14]. AL patients underwent reoperation or interventional therapy if AL led to additional severe complications such as abdominal bleeding, whereas other patients with AL underwent endoscopy or conservative treatment, including fasting,gastrointestinal decompression, drainage, anti-infection therapy, and nutritional support, among other therapeutic measures. During the entire study period, two #28 Penrose drains (Mingchuang Health, Suzhou, Jiangsu Province, China) were routinely placed in the surgical resection bed in patients at the end of the procedure, one at the anastomotic site (tube A) and the other under the left diaphragm (tube B) (Figure 1). A radiological contrast study was performed at the 4thor 5thpostoperative day to assess anastomotic integrity. The drains were subsequently removed 1 or 2 d after starting a soft blended diet. At our institution, ANPLDS therapy (Figure 2) has been a supported first-line treatment for the management of these nonreoperation patients since January 2014. This therapy was started on the day when AL was confirmed and continued until healing of the leak had been confirmed. The healing of the leak was confirmed by the radiological contrast study. For patients with AL, a radiological contrast study was performed once a week.
Design of ANPLDS
In the ward, a #6 sputum suction tube (tube C) was placed next to the anastomotic stoma from the inside of tube A if AL occurred (Figure 1). The inner end of the sputum suction tube was exposed to 0.3-0.5 cm inside tube A (Figure 1), and saline was used for continuous irrigation (150-200 mL/h, 3000 mL/d). The position of tube C was confirmed via X- ray if necessary. Tube A was attached to the drainage bottle(hole a), and a needle was maintained on the outside end of tube A as a blowhole(Figure 1). A suction drain with a negative pressure of 10-20 mmHg was attached to hole b of the drainage bottle (Figure 1).
Outcome measures
The primary outcome of interest was FTR after AL. FTR was defined as mortality after the complication of interest[15,16]. Other postoperative outcomes included other complications, reoperation, and length of stay. The secondary outcomes of interest were clinicopathological and perioperative factors for associations with AL and FTR after AL. In this study, malnourishment was defined by the presence of at least one of the following criteria according to the Guidelines of the European Society for Clinical Nutrition and Metabolism (ESPEN)[17]: weight loss 10%-15% within 6 mo, body mass index (BMI) < 18.5 kg/m2, Subjective Global Assessment Grade C, or serum albumin <30 g/L. However, patients who only met the criterion of BMI < 18.5 kg/m2were considered lean but well-nourished[17,18].
Statistical analysis
Continuous data are reported as the mean ± standard deviation, and categorical data are presented as the proportion percentage and were analyzed by the Chi square test or Fisher's exact test. To identify factors that predicted AL and the FTR rate after AL,variables significant in the univariable analysis (P < 0.05) were included in a multivariate analysis. A binary logistic regression with the forward entry method for the covariates was used to perform a multivariate analysis. All tests were two-sided,and a P-value lower than 0.05 was used to define statistical significance. Statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, United States).
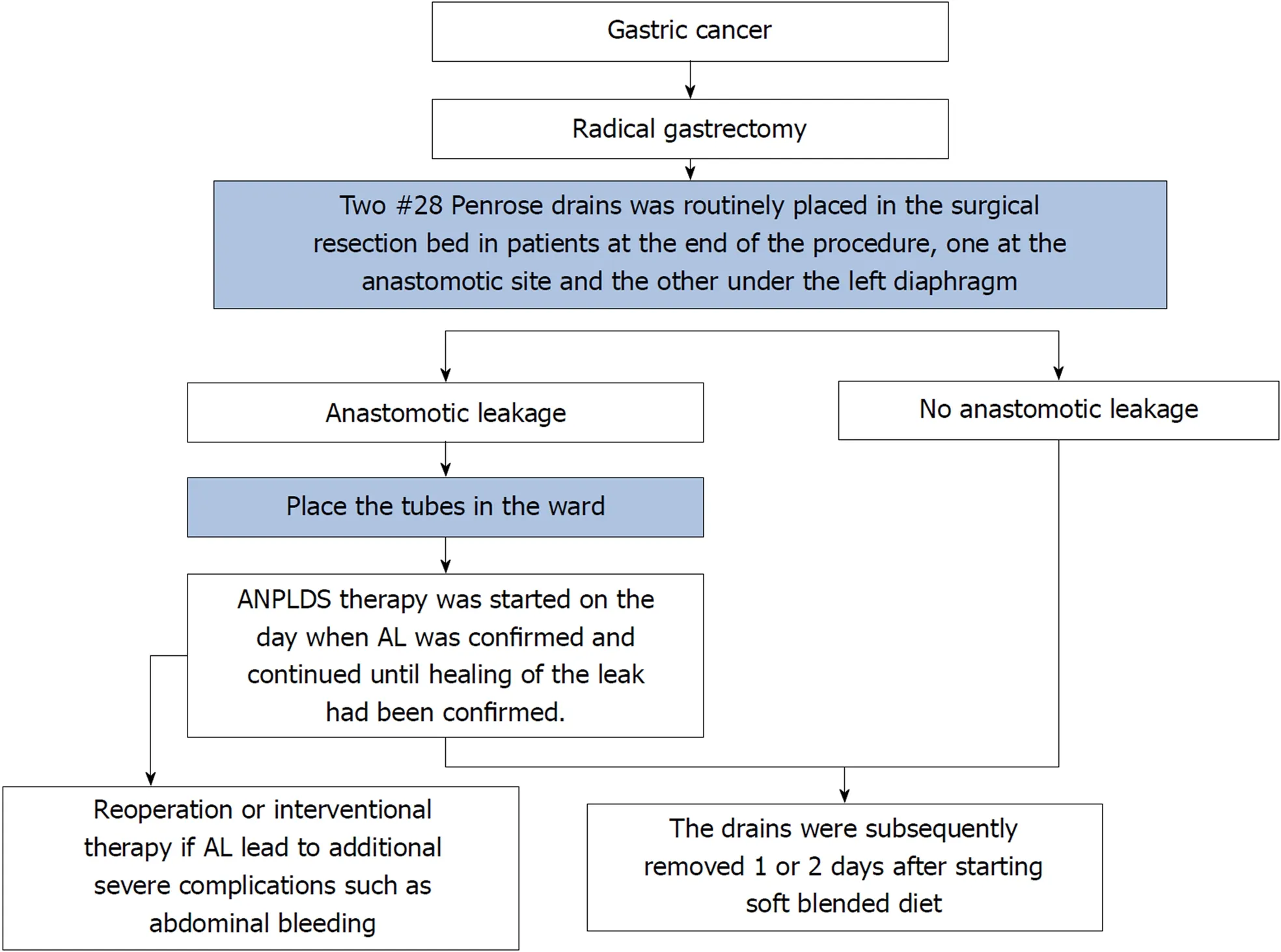
Figure 1 Schematic diagram of the novel abdominal negative pressure lavage-drainage system. During the entire study period, two #28 Penrose drains were routinely placed in the surgical resection bed in patients at the end of the procedure, one at the anastomotic site (tube A) and the other under the left diaphragm (tube B). In the ward, a#6 sputum suction tube (tube C) was placed next to the anastomotic stoma from the inside of tube A if anastomotic leakage occurred. ANPLDS: Abdominal negative pressure lavage-drainage system; AL: Anastomotic leakage.
RESULTS
Population
Between June 2009 and December 2016, a total of 83 patients experienced AL among the 4173 identified patients. Data are compared between 2009 and 2013, which was the period before implementation of the ANPLDS therapy (period 1); as well as between 2014 and 2016, which was after the implementation (period 2). The incidence of AL before and after implementation of the ANPLDS therapy was similar [1.7%(37/2219) vs 2.3% (46/1958), P = 0.121]. Clinicopathological, preoperative, and operative data are reported in Table 1.
Postoperative morbidity and mortality
AL occurring in 83 patients resulted in 7 deaths. The mean time of occurrence of AL was 5.6 d. The mean length of postoperative stay was 30.2 d. These AL required no invasive treatment in 58 (69.9%) patients, CT-guided puncture drainage in 16 (19.3%)patients, endoscopy in 3 (3.6%) patients, and reoperation in 6 (7.2%) patients.Postoperative morbidity, mortality, and treatment are summarized in Table 2.Compared with period 1, the rates significantly decreased for FTR (16.2% vs 2.2%, P =0.041) and abdominal bleeding (18.9% vs 2.2%, P = 0.020) in period 2, but the time of AL occurrence and postoperative hospital stay for patients with AL were similar for the two periods (5.4 d vs 5.7 d, P = 0.738; 31.6 d vs 28.4 d, P = 0.458, respectively).Moreover, the reoperation rate was also reduced in period 2, although this result was not statistically significant (13.5% vs 2.2%, P = 0.084).
The univariate analysis showed that AL were most significantly associated with age≥ 65, malnourishment, comorbidities, HB < 90 g/dL, and total gastrectomy(Supplemental Table 1). The multivariate analysis showed that the two factors independently associated with major complications were age ≥ 65 and malnourishment (Table 3).
FTR
The FTR rate after AL was 8.4% (7/83) over the whole study period. The univariate analysis showed that the only factor independently associated with the risk of FTR rate after AL was ANPLDS therapy [odds ratio (OR) = 0.103, 95%CI: 0.012-0.898, P =0.040] (Table 4). The detailed clinical characteristics of the deaths with AL are presented in Supplemental Table 2.
DISCUSSION
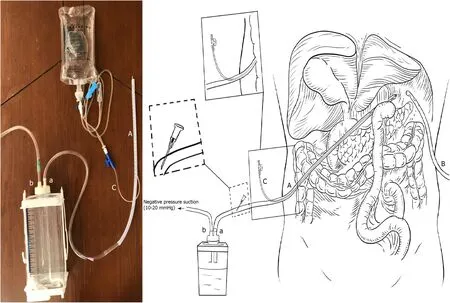
Figure 2 The abdominal negative pressure lavage-drainage system therapy for anastomotic leakage after radical gastrectomy.
AL is a common serious complication after gastrectomy in patients with GC. It is also the most important cause of postoperative abdominal infection, abscess, and abdominal bleeding. Improper management of AL may also increase the risk of death,prolong the length of stay, increase the cost of hospitalization, and even affect longterm survival[3,4]. Therefore, it is essential to identify the risk factors for AL and to take effective treatment measures.
Several risk factors have been reported to be associated with AL, such as age, sex,smoking, malnutrition, longer operative time, tumor location, and tumor stage[19-22]. In this study, we found that age ≥ 65 and malnutrition were independent risk factors for AL after RG, which is consistent with previous studies by our center[23]. Elderly or malnourished patients often suffer from poor body conditions and insufficient blood and energy supply in the anastomotic area, which increases the risk of anastomotic fistula. Therefore, clinicians need to pay more attention to these patients and take appropriate measures to prevent postoperative AL, such as preoperative correction of malnutrition, intraoperative protection of perianastomotic tissue, perioperative supplemental oxygen administration[22], and appropriate use of antibiotics. Even with this, AL cannot be completely avoided. Therefore, it is the goal of clinical attention to select reasonable treatment methods and reduce the FTR rate in a situation of AL.However, the choice of treatment measures after the onset of AL is rarely reported.
When AL occurs, the most important treatment is effective and unobstructed drainage. However, traditional drainage techniques to treat AL depend on gravity and pressure in the cavity with AL. In addition, viscous secretions greatly affect drainage and may even clog the drainage tube. Moreover, secretions that fail to discharge in a timely manner can cause abdominal infection or abscess and may also corrode vascular stumps in the local area, resulting in anastomotic or abdominal bleeding.
For better drainage, negative pressure-flush is often used clinically. Lin et al[24]found that continuous negative pressure-flush through an extraperitoneal dual tube can increase the successful rate of conservative therapy, decrease the reoperation rate,and improve the quality of life when combined with the use of an intra-rectal dual tube. Jiang et al[25]achieved an early intervention for severe bile leakage and pancreatic fistula after pancreaticoduodenectomy using an enclosed passive infraversion lavagedrainage system (EPILDS). However, the application of negative pressure flush in the treatment of GC gastrointestinal fistula has not been reported. Therefore, we present our utilization of and experiences with ANPLDS for AL after RG for GC in this study.We believe that the key reasons for our success with ANPLDS therapy were the use of local continuous irrigation and negative pressure drainage. First, continuous irrigation dilutes secretions, which is beneficial for the discharge of secretions via the drainage tube. Second, liquid is actively drawn off using negative pressure. The sustained air flow in the tubes makes the pressure in the tube lower than that in the area to be rinsed. Thus, secretions and necrotic tissue can be removed in a timely manner. Therefore, ANPLDS reduces local inflammation and provides a good environment for the closing and healing of an AL-inducing rupture.
FTR or death after major complications has gained acceptance as an interestingmetric evaluation of quality after surgery[26,27]. Although the definition of FTR varies widely in the previous literature, surgeons and researchers agree that the ability torescue patients from severe postoperative complications, thus preventing mortality, is key to improve the quality and safety of surgery. We found that ANPLDS therapy was the only independent protective factor associated with FTR after AL. Our simple ANPLDS reduced the FTR, primarily due to decreases in reoperation and in the occurrence of severe complications such as abdominal bleeding. It is reasonable to believe that the decline in FTR is a direct external effect of this new treatment, because the FTR rate decreased suddenly after the implementation of ANPLDS. Additionally,our surgical team had performed more than 1000 cases and had sufficiently mastered the RG procedure for GC before the study period. Therefore, the impact of increasing experience on mortality that is expected to be progressive can be ignored. Of course,other factors that cannot be specifically measured in this study, such as the improvement of ICU care or postoperative care practices, may have an impact on FTR, but it does not seem likely to significantly reduce mortality in the short term.Therefore, we believe that this system is a potentially advantageous alternative to the treatment of AL.
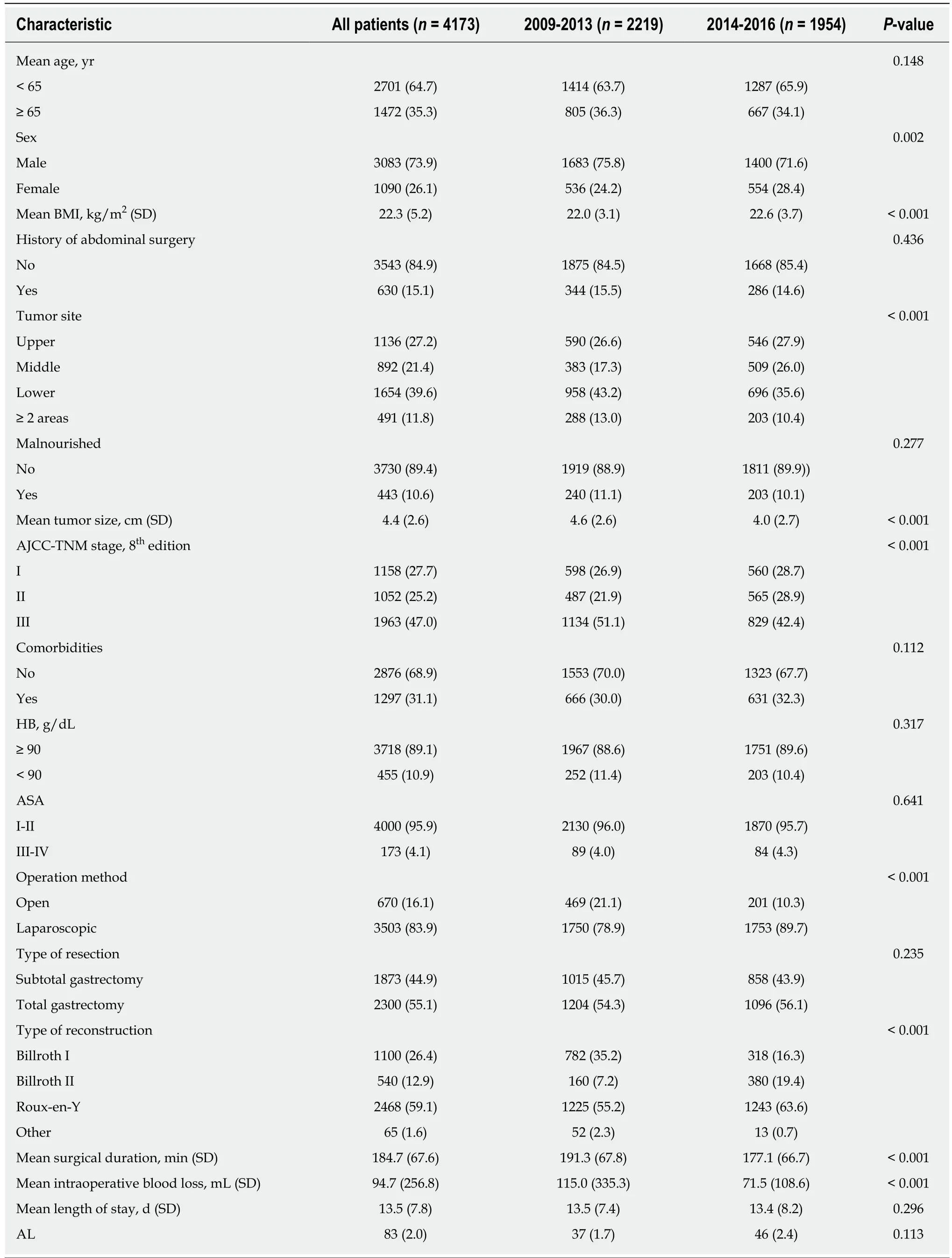
Table 1 Characteristics of patients who underwent R0 resection for gastric cancer n (%)
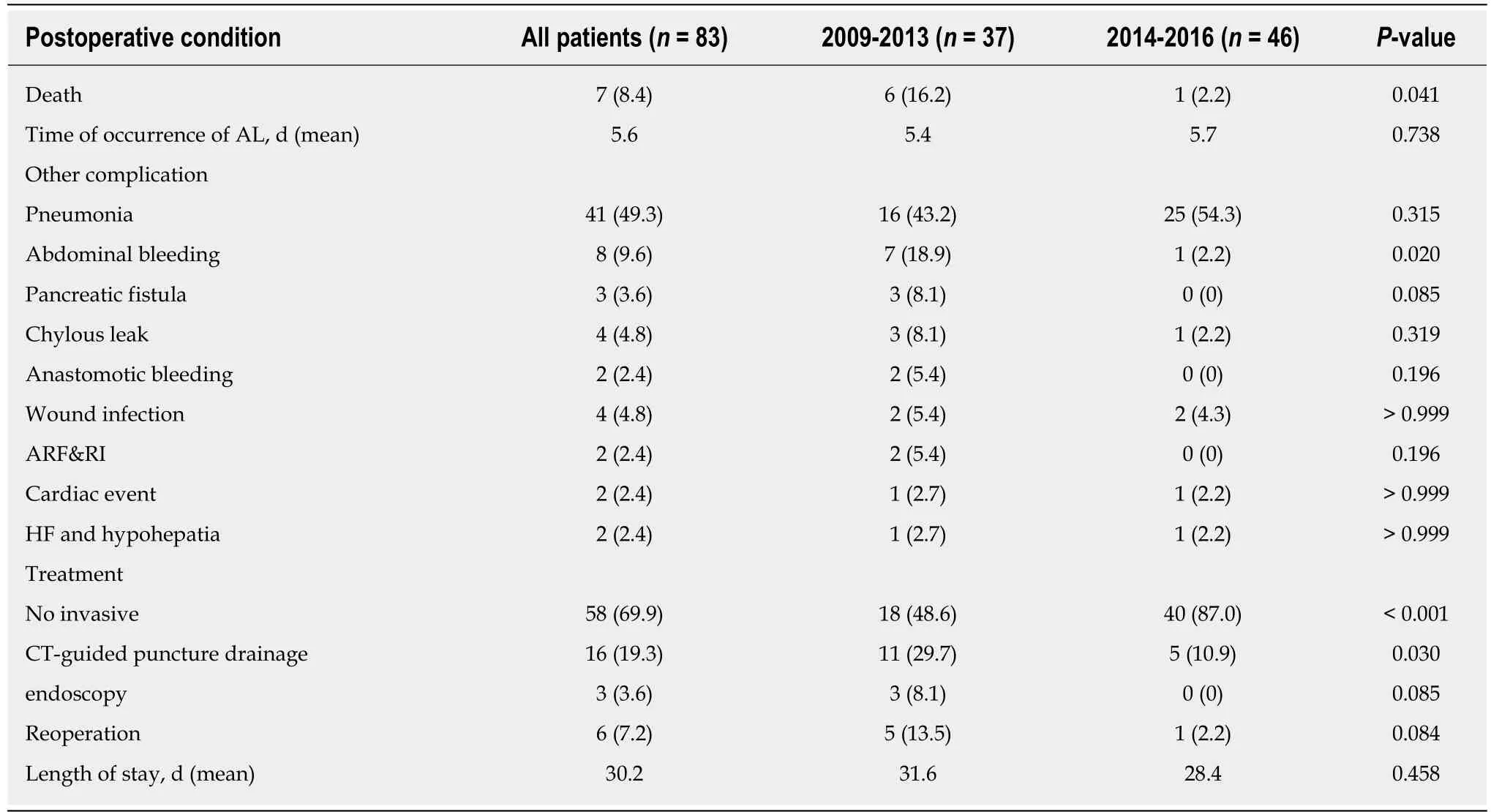
Table 2 Postoperative mortality, morbidity, and treatment modality among patients with anastomotic leakage after radical gastrectomy before (2009-2013) and after (2014-2016) implementation of the abdominal negative pressure lavage-drainage system n (%)
This study had several limitations. First, it is a single-center retrospective study that needs to be verified by a multi-center, large sample prospective trial. Second, due to the limited number of AL cases, we analyzed all reconstruction methods instead of focusing solely on one type of anastomosis, which may increase the heterogeneity of the patient's material. However, we first reported the feasible management of AL and the successful implementation of this system at our institution may serve as a model for treating AL at other centers.
In conclusion, ANPLDS can effectively reduce the FTR and abdominal bleeding rates after AL. Our experience demonstrates that ANPLDS is a feasible management for AL after RG for GC.
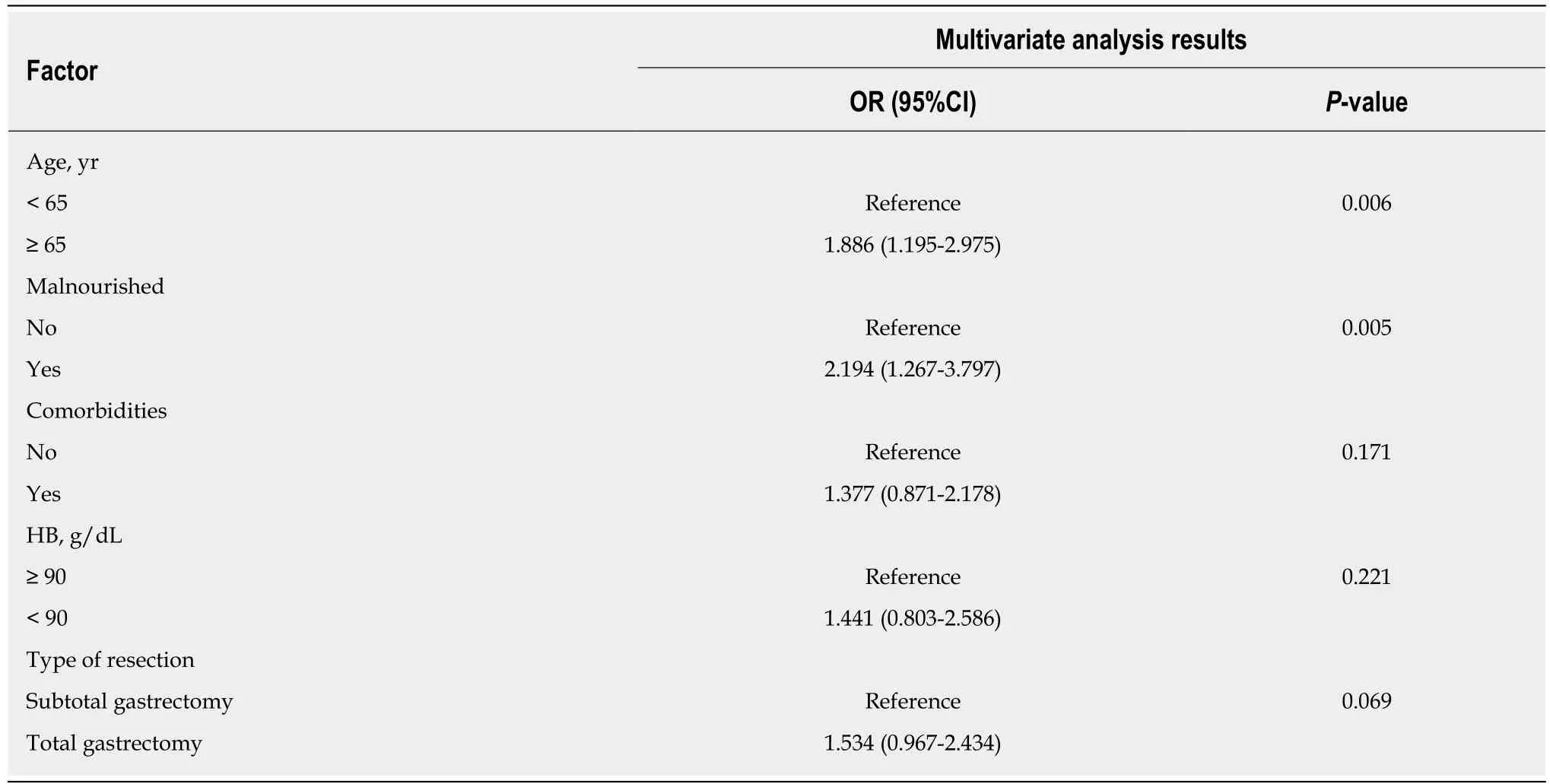
Table 3 Risk factors predictive of anastomotic leakage after radical gastrectomy
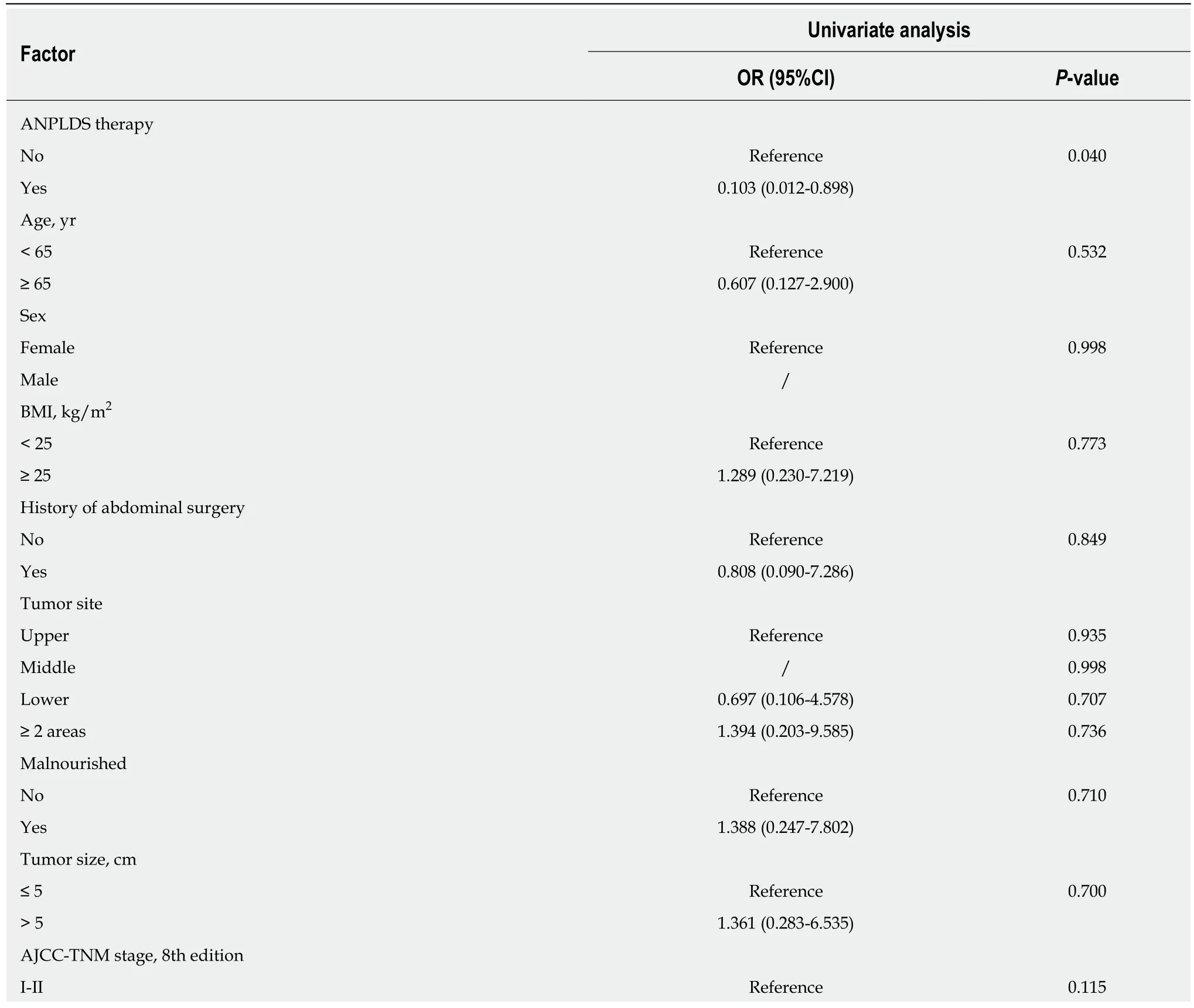
Table 4 Risk factors predictive of failure-to-rescue after anastomotic leakage with radical gastrectomy for gastric cancer
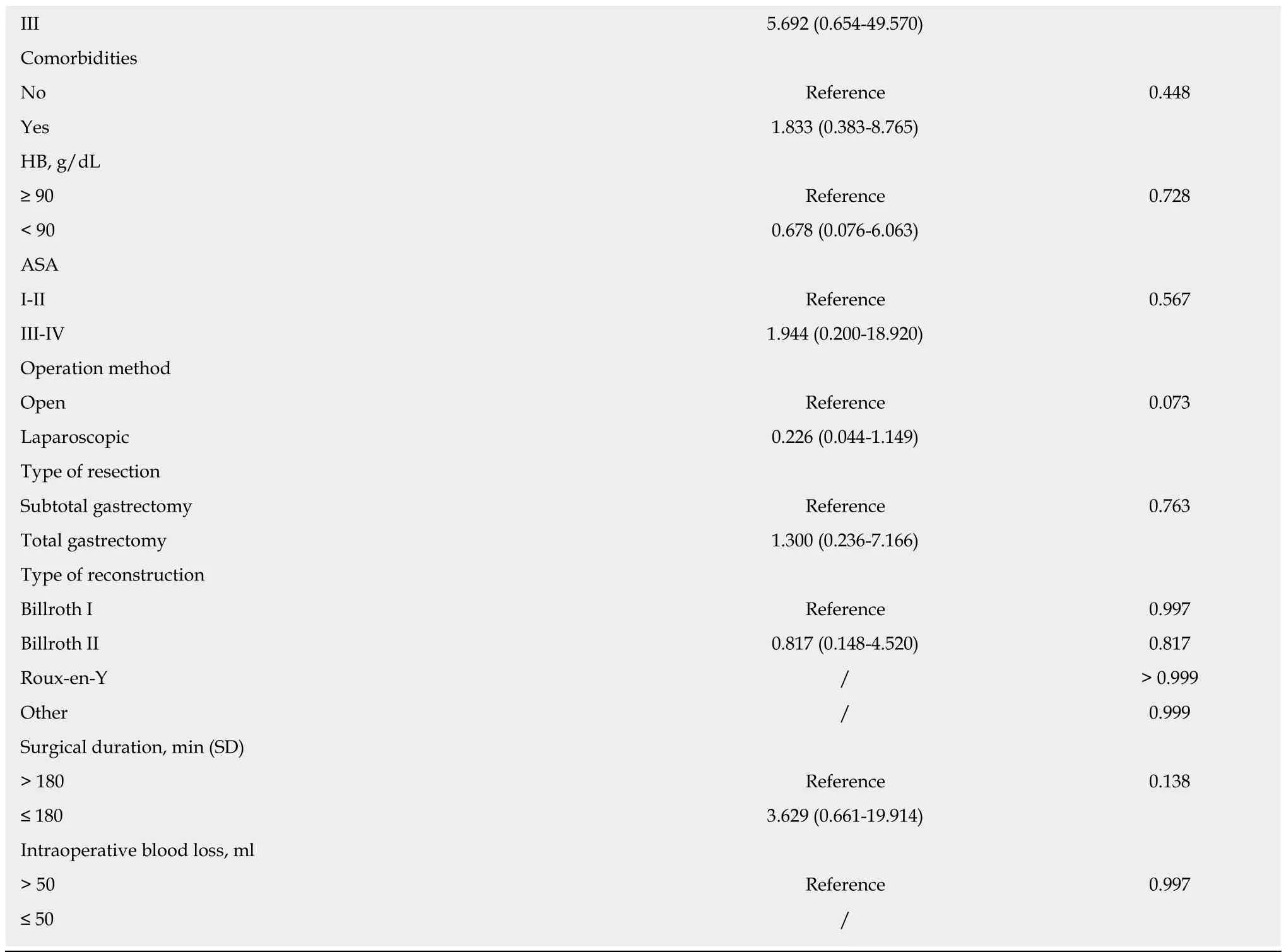
ANPLDS: Abdominal negative pressure lavage-drainage system; BMI: Body mass index; HB: Hemoglobin; ASA: American Society of Anesthesiologists.
ARTICLE HIGHLIGHTS
Research background
Anastomotic leakage (AL) remains relatively common and represents a major cause of postoperative morbidity after radical gastrectomy (RG) for gastric cancer (GC). AL is associated with high mortality.
Research motivation
Prophylactic drainage of the abdominal cavity is widely performed. The optimal creation of drainage in AL patients after RG remains controversial.
Research objectives
The novel abdominal negative pressure lavage-drainage system (ANPLDS) is a feasible management for AL. Therefore, we present our utilization of and experiences with ANPLDS for AL after RG for GC.
Research methods
In January 2014, a novel ANPLDS was routinely used for patients with AL at our institution. AL rates and postoperative outcome were compared before and after the ANPLDS therapy.
Research results
The novel ANPLDS can effectively reduce the failure-to-rescue and abdominal bleeding rates after AL.
Research conclusions
Our experience demonstrates that the novel ANPLDS is a feasible management for AL after RG for GC.
Research perspectives
The successful implementation of the novel ANPLDS at our institution may serve as a model for treating AL after RG for GC at other centers.
杂志排行
World Journal of Gastroenterology的其它文章
- Role of diet and gut microbiota on colorectal cancer immunomodulation
- Current status, problems, and perspectives of non-alcoholic fatty liver disease research
- Prevention of overuse: A view on upper gastrointestinal endoscopy
- Adverse events related to colonoscopy: Global trends and future challenges
- Human antigen R mediated post-transcriptional regulation of inhibitors of apoptosis proteins in pancreatic cancer
- Six-long non-coding RNA signature predicts recurrence-free survival in hepatocellular carcinoma
